Approach
Confirmatory laboratory tests should be performed before starting therapy for those in whom amebiasis is suspected. Diagnostic tools include stool antigen detection, stool (or abscess aspirate in the case of extraintestinal disease) polymerase chain reaction (PCR) testing, stool microscopy, serology, and colonoscopy with histologic exam.
Clinical evaluation
Amebiasis should be considered in any individual who presents with diarrhea or liver abscess and who has traveled or lived in an endemic area in the previous 12 months. Other populations at risk of infection are institutionalized individuals, men who have sex with men, and commercial sex workers and their sexual contacts.[13]
Presentation is subacute in many cases; most patients have a gradual illness onset days or weeks after infection.[9] Key symptoms of infection are diarrhea that has lasted for several days or longer and abdominal pain. Entamoeba histolytica diarrhea is usually lacking blood or mucus, and is therefore indistinguishable from diarrhea caused by a variety of other enteropathogens. However, the patient may report blood in their stool, however. Weight loss is reported by about 50% of patients.[1] Right upper quadrant (RUQ) abdominal pain in a man aged 20 to 40 years, with or without coincident diarrhea, could indicate an amebic liver abscess.[1][2][3][4][5] Patients may report altered mental status if brain abscess is present. Amebic acute appendicitis is a possible but rare manifestation of amebiasis; amebic appendicitis is more likely to be complicated than non-amebic appendicitis.[8]
Physical examination
Fever is rare with intestinal infection but common with hepatic infection.
With hepatic infection, jaundice, RUQ tenderness, and hepatomegaly may be present. Liver abscesses may extend into the pleural or pericardial cavities (rare), resulting in signs of a pleural or pericardial effusion. Splenic abscess is a rare manifestation of amebiasis.
Neurologic abnormalities, such as limb weakness, may be present in patients with a brain abscess.
Laboratory evaluation
Of the available diagnostic tests, antigen testing and PCR can differentiate between E histolytica and the nonpathogenic E dispar. PCR has the highest sensitivity and is the method of choice for diagnosis; however, protocols (DNA extraction and primer-probe sets) are not fixed, and only limited institutes can return reliable results. Also, cost is a barrier to its use as a routine test in many endemic areas. Laboratory diagnosis of intestinal amebiasis in many countries still relies on antigen detection or ova and parasite microscopy.[22]
Microscopy
Stool microscopy relies on observation of cysts and trophozoites in feces, colonic scrapings, aspirates and tissue samples.[23] It is not specific for the diagnosis of amebiasis, as E histolytica cysts and trophozoites are indistinguishable from those of E dispar, E moshkovskii, and E bangladeshi. Historically, E dispar and E moshkovskii have been considered nonpathogenic, but evidence is mounting that E moshkovskii can cause illness; E bangladeshi has only recently been identified, so its pathogenic potential is not well understood.[9] Whilst it lacks specificity, stool microscopy for ova, cysts, and parasites has the advantage of being readily available and may demonstrate other infectious causes. The presence of erythrophagocytic trophozoites is highly suggestive of E histolytica infection. UK guidelines recommend that stool samples which are positive on microscopy for Entamoeba spp. should be sent for confirmatory PCR testing.[23]
PCR
Where available, PCR is now the method of choice for diagnosis of E histolytica.[9][23] PCR and real-time quantitative PCR (qPCR) testing of stool is highly sensitive and specific for the detection of E histolytica.[24] Real-time qPCR is more sensitive than traditional PCR.[24] Stool samples which are positive on microscopy for E histolytica/dispar should be sent for confirmatory PCR testing.[23]
Liver abscesses should be aspirated to determine etiology. The pus should be analyzed by PCR or qPCR to identify whether the causal infection is amebic and cultured to determine whether it is pyogenic.[1][2]
Antigen testing
Antigen testing on stool samples is an alternative to PCR. Antigen tests have been well studied and have several advantages, including their technical simplicity, relative low cost and rapid turnaround.[23] Available testing kits include the TechLab E histolytica II (ELISA), the TechLab E. HISTOLYTICA QUIK CHEK, or The Cellabs Entamoeba CELISA Path. These are highly specific for E histolytica; other detection kits detect the E histolytica-E dispar-E moshkovskii species complex.[25]
Serum antibody testing
In patients with suspected amebic disease, especially possible liver abscess without concurrent intestinal infection (where there are unlikely to be detectable parasites in the stool), serum antibody testing for E histolytica can be a useful diagnostic adjunct.[2][25] Tests for antibodies are approximately 90% sensitive for amebic liver abscess and 70% sensitive for amebic colitis.[2] A major problem with serological tests however, is that the patient continues to test positive for years after an episode of amebiasis; as a result, a substantial number (10% to 35%) of residents of developing countries have antibodies to amebae. Therefore, negative serology is helpful for exclusion of disease, but positive serology cannot distinguish between acute and previous infection.[2]
[Figure caption and citation for the preceding image starts]: Cyst of Entamoeba histolytica: iodine stain of stool sampleReproduced from Current Concepts (2003); used with permission [Citation ends]. [Figure caption and citation for the preceding image starts]: Cyst of Entamoeba histolytica: unstained (A), and iodine stained (B) after formalin-ether concentration of stool sample.Original photos from National Center for Global Health and Medicine, Tokyo, Japan. [Citation ends].
[Figure caption and citation for the preceding image starts]: Cyst of Entamoeba histolytica: unstained (A), and iodine stained (B) after formalin-ether concentration of stool sample.Original photos from National Center for Global Health and Medicine, Tokyo, Japan. [Citation ends].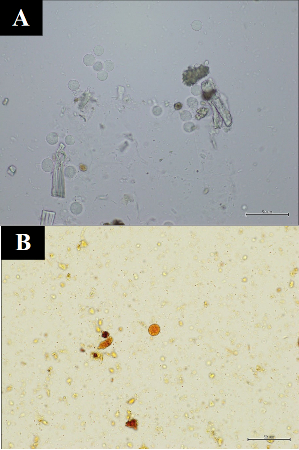 [Figure caption and citation for the preceding image starts]: Trophozoites of Entamoeba histolytica: trichrome stain of stool sampleReproduced from Clinical Infectious Diseases (1999); used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Trophozoites of Entamoeba histolytica: trichrome stain of stool sampleReproduced from Clinical Infectious Diseases (1999); used with permission [Citation ends].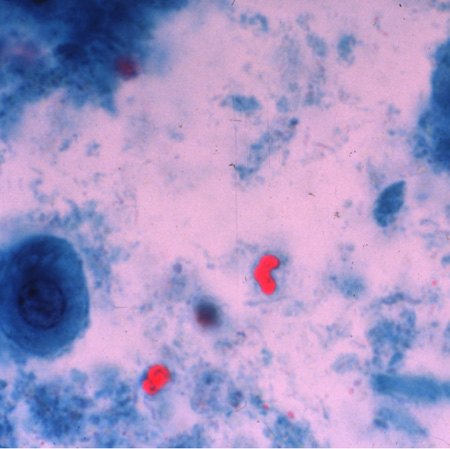 [Figure caption and citation for the preceding image starts]: Trophozoite of Entamoeba histolytica with pseudopod (red arrow): direct unstained stool sample.Original photo from National Center for Global Health and Medicine, Tokyo, Japan. [Citation ends].
[Figure caption and citation for the preceding image starts]: Trophozoite of Entamoeba histolytica with pseudopod (red arrow): direct unstained stool sample.Original photo from National Center for Global Health and Medicine, Tokyo, Japan. [Citation ends].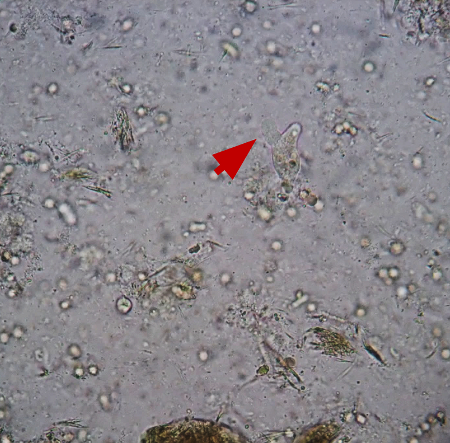
Colonoscopy
May be helpful if clinical suspicion is high and antigen detection tests are negative.[2] Biopsy specimens should be taken from the edge of an ulcer. Histology may show trophozoites, but the sensitivity of histopathological diagnosis using biopsy samples obtained by colonoscopy is low (45.5%).[26] Endocytoscopy may allow for real-time visualization of amebae in the colonic mucosa of patients with colitis.[27] Amebiasis is occasionally diagnosed during detailed examination to investigate chronic diarrhea and positive results on fecal occult blood testing.[28][29][Figure caption and citation for the preceding image starts]: Amebic ulcerations of the colon: colonic ulcers averaging 1 mm to 2 mm in diameter on gross pathologyReproduced from New England Journal of Medicine (2003); used with permission [Citation ends].
Imaging
If liver involvement is suspected, a liver ultrasound should initially be performed. CXR and chest/abdominal CT are indicated if an effusion due to abscess extension is suggested by clinical findings.
[Figure caption and citation for the preceding image starts]: Posterior-anterior and lateral CXR of a patient with amebic liver abscess: CXR findings include elevated right hemidiaphragm and evidence of atelectasisReproduced from New England Journal of Medicine (2003); used with permission [Citation ends].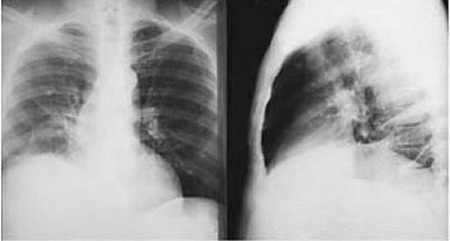
Patients with neurologic symptoms should have a CT or MRI of the brain.[1][5]
[Figure caption and citation for the preceding image starts]: Entamoeba histolytica brain abscessReproduced from Transactions of the Royal Society of Tropical Medicine and Hygiene (2007); used with permission [Citation ends].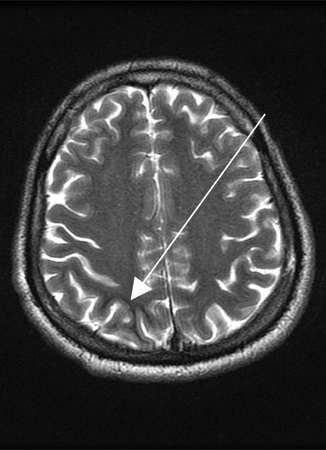
Use of this content is subject to our disclaimer