Etiology
Causative agents can vary according to age group, country, or region. Globally, the most common pathogens causing bacterial meningitis are Neisseria meningitidis and Streptococcus pneumoniae, accounting for 9.1% to 36.2% and 2.1% to 41.2% of bacterial meningitis cases, respectively.[16] In children, S pneumoniae is the most common pathogen, causing 22.5% (Europe) to 41.1% (Africa) of cases. In adults, S pneumoniae causes 9.6% (Western Pacific) to 75.2% (Africa) of cases.[16]
N meningitidis serogroup B is the predominant cause of meningococcal meningitis in Europe, the US, and the Western Pacific. Meningococcal serogroups C and W are most common in most of Africa and Latin America. Serogroup Y cases mostly occur in Nordic countries.[16]
The routine use of Haemophilus influenzae type b (Hib) and conjugate pneumococcal vaccines in the UK and other developed countries has markedly reduced the overall incidence of bacterial meningitis.[5][10][11][17][18] However, because of limited economic resources and poor living conditions, many developing countries continue to have high rates of disease.
In neonates, Escherichia coli and Streptococcus agalactiae (group B streptococci) are major causative agents of bacterial meningitis.[16]
Gram-negative enteric bacilli (e.g., Serratia, Acinetobacter, Klebsiella, and Pseudomonas aeruginosa) contribute to <10% of cases. They can cause disease in neonates, older adults, and people with diabetes mellitus.
Listeria monocytogenes is a common cause of bacterial meningitis in patients using immunosuppressive drugs, people who misuse alcohol, and patients with diabetes.[19][20]
Zoonotic causes of bacterial meningitis are rare, but important to consider when there is a history of exposure to animals. Streptococcus suis, most prevalent in Southeast Asia, is associated with raw pork meat and pig farming. Other zoonotic pathogens include Capnocytophaga canimorsus (associated with dogs), Campylobacter fetus (cattle), and Streptococcus equi (horses).[21][22][23]
Pathophysiology
Bacteria reach the central nervous system either by hematogenous spread (the most common route) or by direct extension from a contiguous site such as the paranasal sinuses or the mastoid bone. Neonates can acquire pathogens from nonsterile maternal genital secretions, through the placenta, or from their surroundings.[9] The bacteria multiply quickly once they have entered the subarachnoid space. Bacterial components in the cerebrospinal fluid induce the production of various inflammatory mediators, which in turn enhance the influx of leukocytes into the cerebrospinal fluid.[24] The inflammatory cascade leads to cerebral edema and increased intracranial pressure, which contribute to neurologic damage and even death. [Figure caption and citation for the preceding image starts]: Ventral view of human brain showing purulent basilar meningitis infection due to Streptococcus pneumoniaeImage provided by the CDC Public Health Image Library [Citation ends].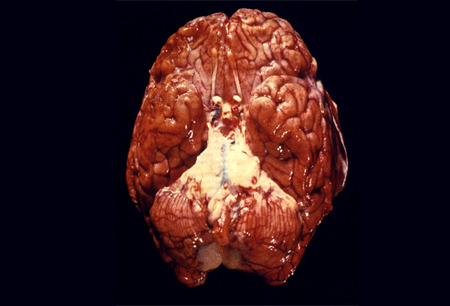
Classification
Common types of bacterial meningitis
Pneumococcal meningitis
Caused by Streptococcus pneumoniae
Meningococcal meningitis
Caused by Neisseria meningitidis
Hib meningitis
Caused by Haemophilus influenzae type b
Use of this content is subject to our disclaimer