Case history
Case history #1
A 20-year-old US college student has recently returned from a 2-month training session in an Amazon rainforest diversity station in Peru. She reports a 2-month history of painless open sores on her leg. Other students in her group have similar skin findings. She also reports intermittent use of personal protective measures and having slept in open-air housing with evening exposure to insect bites. Physical exam reveals two nontender 3 × 3 cm skin ulcerations with indurated rims on her left leg and an enlarged femoral lymph node. No other symptoms are reported.
Case history #2
An 8-year-old boy from the province of Bihar, India is visiting his uncle in Chicago. He reports a 3-month history of intermittent fever, weight loss, fatigue, epistaxis, and abdominal distension. Physical exam reveals pallor, emaciation, and a grossly enlarged spleen.
Other presentations
Localized cutaneous leishmaniasis (CL) tends to affect skin areas readily exposed to sand fly bites (i.e., face, arms, and lower limbs). Occasionally, lesions are reported on atypical areas (e.g., sexual organs).[9] An auricular manifestation of CL is a single ulcerative lesion, typically involving the ear pinna (known as "chiclero's" ulcer in southeast Mexico and Latin America when caused by Leishmania mexicana).[10] Lesions may develop at sites distant from the sand fly bite, such as sites of minor trauma (e.g., bee sting, new tattoo, surgical incision), or may be disseminated in immunocompromised hosts.[11] Skin lesions are chronic, usually painless, and can have various appearances, but cutaneous induration is present. There may be multiple or single lesions. Small subcutaneous nodules may be palpated (nodular lymphangitis) often in a sporotrichoid pattern, and regional lymphadenopathy may be present in some cases.
Mucosal leishmaniasis (also known as espundia) may occur concurrently with localized CL or years later after the skin lesion has healed. It is restricted to the mucosa (generally nasal, oropharyngeal, or laryngeal) with patients complaining of nasal congestion, discharge, epistaxis, throat irritation, or, most concerningly, changes in their voice. Physical exam usually reveals inflammation of the anterior nasal septum (sometimes with perforation), hypertrophy of the tissue of the upper lip and mucosa, or granulomatous tissue on the pharynx/larynx that may ulcerate. A hypopigmented atrophic scar may be noted, indicative of a prior infection.[12][13]
Visceral leishmaniasis (VL) is characterized by a spectrum of clinical presentations from asymptomatic, to paucisymptomatic, to symptomatic (characterized by fever, weight loss, organomegaly, cytopenias, and hypergammaglobulinemia).
Skin darkening of the hands, feet, forehead, or abdomen, which led to the name of kala-azar ("black fever" in Hindi), is sometimes present in patients with VL from South Asia. Enlarged lymph nodes are observed frequently in Sudanese patients with VL, but rarely in patients from other areas. Concomitant bacterial infections (e.g., pneumonia, diarrhea, or tuberculosis) may confuse the initial clinical presentation. Digestive (e.g., persistent diarrhea, dysphagia) or respiratory symptoms may be presenting symptoms in patients with severe cell-mediated immunosuppression.
Post-kala-azar dermal leishmaniasis (PKDL) may occur months or years after treatment of VL.[6] Characterized by a macular, maculopapular, or nodular rash, PKDL is mainly found in East African, particularly Sudanese, and also Bangladeshi patients; less frequently it is found in patients from other Leishmania donovani-endemic countries (i.e., India); and, rarely, in Leishmania infantum(synonym: Leishmania chagasi)-infected patients with immunosuppression.
CDC: parasites – leishmaniasis
Opens in new window
WHO: leishmaniasis
Opens in new window[Figure caption and citation for the preceding image starts]: Ulcerative Leishmania braziliensis lesion from a student who traveled to PeruFrom the collection of Dr N. Aronson; used with permission [Citation ends]. [Figure caption and citation for the preceding image starts]: Mucosal leishmaniasis in 2 Brazilian patients. A-D: patient 1 with positron emission tomography/computed tomography (PET/CT) images showing enhancement and subcutaneous thickening adjacent to erosion of the left nasal wing and obliteration of the posterolateral recess (A and B), 3D volume-rendered image of multislice CT data (3D CT) and picture with erosion of the left nasal wing (C and D). F-H: patient 2 with PET/CT images showing preserved glycolytic metabolism of facial structures (E and F), 3D CT with collapse of the nasal pyramids (G), and bone window CT with diffuse thickening of nasal wings and collapse of the nasal pyramid (H)Am J Trop Med Hyg; CC BY-4.0 (https://creativecommons.org/licenses/by/4.0/) [Citation ends].
[Figure caption and citation for the preceding image starts]: Mucosal leishmaniasis in 2 Brazilian patients. A-D: patient 1 with positron emission tomography/computed tomography (PET/CT) images showing enhancement and subcutaneous thickening adjacent to erosion of the left nasal wing and obliteration of the posterolateral recess (A and B), 3D volume-rendered image of multislice CT data (3D CT) and picture with erosion of the left nasal wing (C and D). F-H: patient 2 with PET/CT images showing preserved glycolytic metabolism of facial structures (E and F), 3D CT with collapse of the nasal pyramids (G), and bone window CT with diffuse thickening of nasal wings and collapse of the nasal pyramid (H)Am J Trop Med Hyg; CC BY-4.0 (https://creativecommons.org/licenses/by/4.0/) [Citation ends].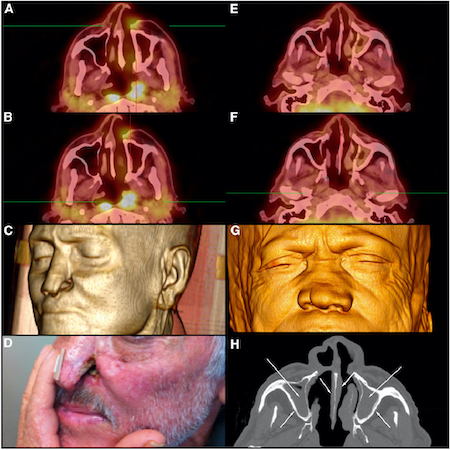 [Figure caption and citation for the preceding image starts]: Ulcerative Leishmania mexicana lesion, pre- and post-treatmentFrom the collection of Dr N. Aronson; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Ulcerative Leishmania mexicana lesion, pre- and post-treatmentFrom the collection of Dr N. Aronson; used with permission [Citation ends]. [Figure caption and citation for the preceding image starts]: Hepatosplenomegaly in an Ethiopian patient with visceral leishmaniasisImage courtesy of the World Health Organization [Citation ends].
[Figure caption and citation for the preceding image starts]: Hepatosplenomegaly in an Ethiopian patient with visceral leishmaniasisImage courtesy of the World Health Organization [Citation ends]. [Figure caption and citation for the preceding image starts]: Nodular post-kala-azar dermal leishmaniasis in an Ethiopian patientImage courtesy of the World Health Organization [Citation ends].
[Figure caption and citation for the preceding image starts]: Nodular post-kala-azar dermal leishmaniasis in an Ethiopian patientImage courtesy of the World Health Organization [Citation ends].
Use of this content is subject to our disclaimer