Tests
1st tests to order
renal ultrasound
Test
Test is performed when diagnosis is suspected. It is noninvasive, safe, relatively inexpensive, and widely available.
The unified criteria for ultrasonographic diagnosis of autosomal-dominant PKD (ADPKD) was developed for testing individuals who are at risk for ADPKD (those with a positive family history, who are at 50% risk for the disease) as molecular genotyping is seldom performed.[42]
In a child ages under 15 years with a positive family history of ADPKD, detection of one or more renal cysts on ultrasound is highly suggestive of ADPKD.[7]
Result
disease confirmation if: 15 to 39 years of age - at least 3 (unilateral or bilateral) renal cysts; 40 to 59 years of age - at least 2 cysts in each kidney; >60 years of age - at least 4 cysts in each kidney
CT abdomen/pelvis
Test
A contrast-enhanced CT scan can detect cysts of 2 to 3 mm in diameter and is particularly useful for diagnosis in younger patients.[4][Figure caption and citation for the preceding image starts]: CT scan of abdomen and pelvis of patient with mild diseaseFrom collection of Dr M. Hogan [Citation ends].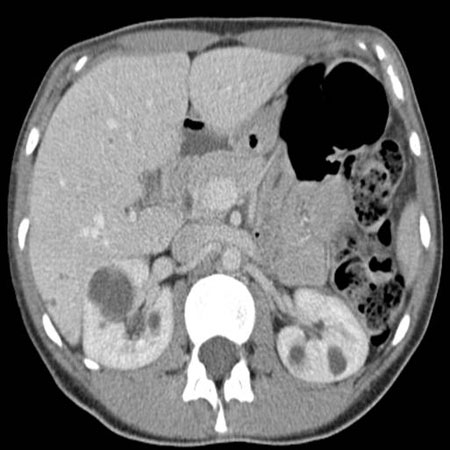
Imaging by CT scan or MRI should be part of the initial evaluation of autosomal-dominant PKD, as it provides precise, standardized measurement of maximum kidney length, width, and depth measurements, and an estimate of total kidney volume.[31] These quantitative data are of prognostic value.[1]
An image-based classification system based on total kidney volumes from CT scan or MRI has been used to identify potential cases of more rapidly progressive disease. This classification system may optimize patient selection for specific disease therapy.[44]
Result
detection of cystic disease (renal and extrarenal); quantitative data on total kidney volume
MRI abdomen/pelvis
Test
A MRI scan can detect cysts of 2 to 3 mm in diameter and is particularly useful for diagnosis in younger patients.[4][Figure caption and citation for the preceding image starts]: MRI of abdomen and pelvis of patient with symptomatic polycystic kidney diseaseFrom collection of Dr M. Hogan [Citation ends].
In one study of at-risk individuals (a positive family history with a 50% risk of autosomal-dominant PKD [ADPKD]) younger than 30 years of age, using a criterion of a total of >10 cysts seen on MRI can be considered as sufficient for diagnosis.[43]
Imaging by CT scan or MRI should be part of the initial evaluation of ADPKD, as it provides precise, standardized measurement of maximum kidney length, width, and depth measurements, and an estimate of total kidney volume.[31] These quantitative data are of prognostic value.[1]
An image-based classification system based on total kidney volumes from CT scan or MRI has been used to identify potential cases of more rapidly progressive disease. This classification system may optimize patient selection for specific disease therapy.[44]
Use of gadolinium contrast should be avoided in patients with advanced kidney disease (GFR <30 mL/minute/1.73 m²).
Result
detection of cystic disease (renal and extrarenal); a total of >10 renal cysts confirms diagnosis in at-risk individuals; quantitative data on total kidney volume
urinalysis/Gram stain and urine culture
Test
Ordered in all patients to detect presence of increased urinary albumin excretion or proteinuria.
Increased urinary albumin excretion or proteinuria indicate a higher likelihood of progression to chronic kidney disease.[31][40]
Microscopic or macroscopic hematuria are common.
Leukocyturia does not always indicate urinary tract infection (UTI), and a urine culture should be obtained in this situation.
Urine culture is always obtained if there are symptoms of UTI or fever.[1]
Urine culture may be negative, even with serious urine infection, because cysts do not communicate with the urinary tract.
Result
significant bacteriuria in setting of UTI, microscopic hematuria, proteinuria, increased urinary albumin excretion
serum electrolytes, BUN, creatinine
Test
Not a sensitive test. Creatinine is often normal in these patients but can be used to estimate GFR.[31] [ Glomerular Filtration Rate Estimate by the IDMS-Traceable MDRD Study Equation Opens in new window ]
Electrolytes should be followed in patients on ACE inhibitors or diuretics.
End-stage renal disease develops in approximately 50% of affected patients by 60 years of age.[1] In most people renal function remains in the normal range, despite cyst growth, until the fourth to sixth decade of life.
Result
normal or elevated
fasting lipid profile
Test
Elevated total and LDL cholesterol and low HDL levels have been associated with increased risk of renal insufficiency and should be treated appropriately.[40]
Result
normal or elevated (prognostic marker)
ECG
Test
Ordered in patients with cardiac murmurs or suspected left ventricular dysfunction.
Result
left ventricular hypertrophy changes in setting of cardiovascular complications
Tests to consider
genetic testing
Test
Genetic testing (linkage analysis or complete gene sequencing) should be considered when imaging studies are inconclusive, to confirm a presumed diagnosis in the absence of family history of the disease, or in rare cases for prenatal diagnosis or possibly for preimplantation genetic diagnosis.[21]
Whole-genome sequencing has been validated to identify all types of variants in the PKD1 gene and can be considered in the assessment of patients with PKD, particularly in atypical disease.[19]
Despite comprehensive screening, 10% to 15% of patients suspicious of autosomal-dominant PKD (ADPKD) have no mutation detected in either PKD1 or PKD2.[21] Patients can be rescreened for mutations of a newly identified gene for ADPKD, GANAB, and somatic mosaicism.[20] If there are existing genetic test results, do not order a duplicate test unless there is uncertainty about the existing result, e.g., the result is inconsistent with the patient’s clinical presentation or the test methodology has changed.[55]
Result
PKD1 or PKD2 mutation
echocardiogram
Test
Considered in selected patients for assessment of left ventricular hypertrophy (LVH), cardiac function, and valvular abnormalities.[45]
Result
mitral valve prolapse, aortic root dilation, diastolic dysfunction, or LVH in setting of cardiovascular complications
24-hour urine collection
Test
All patients with metabolically active stone disease should have 24-hour urine collection for urine biochemistry (urine volume, pH, oxalate, uric acid, citrate, phosphate, sodium, calcium, and creatinine) to assess the completeness of the collection, and urinary supersaturation should be calculated.
Low urine citrate is consistent with distal renal tubular acidosis; high urine uric acid or oxalate may be found.
Proteinuria is quantified. Increased urinary albumin excretion or proteinuria indicate a higher likelihood of progression to chronic kidney disease.[31][40]
Result
low citrate, high uric acid, or oxalate in setting of stones, proteinuria
dual-energy CT of abdomen/pelvis
Test
Dual-energy CT can discriminate uric acid stones from other (non-uric acid) renal stones.[31]
Differences in attenuation values are usually higher in stones containing no uric acid.
Result
differences in attenuation values differentiate between stones if present
lumbar puncture and cerebrospinal fluid analysis
Test
Considered only in selected patients where ruptured intracranial aneurysm is a concern.
If noncontrast CT brain is negative and index of suspicion of intracranial bleed remains high, a lumbar puncture is obtained.[47] If xanthochromia is present this result is highly suggestive of intracranial hemorrhage.
How to perform a diagnostic lumbar puncture in adults. Includes a discussion of patient positioning, choice of needle, and measurement of opening and closing pressure.
Result
elevated cerebrospinal fluid pressure or xanthochromia in setting of ruptured intracranial aneurysm
C-reactive protein
Test
Useful in diagnosis of infected renal or hepatic cyst(s).[1] In one study, cyst infection was probable if all 4 of the following criteria were met: temperature of >100.4°F (>38°C) for >3 days, loin or liver tenderness, C-reactive protein plasma level of >5 mg/dL, and no CT evidence for intracystic bleeding.[58]
Result
>5 mg/dL suggests infection
Use of this content is subject to our disclaimer
