Differentials
Common
Peptic ulcer disease (PUD)
History
history of NSAID use (often with concomitant use of corticosteroids) or past ulcers is common; ingestion of food often transiently improves abdominal pain; coffee-ground emesis and hematemesis are very common; hematochezia (bright red blood from the rectum) is rare, and is usually associated with extremely brisk UGIB and significant hemodynamic compromise
Exam
midepigastric tenderness to palpation
1st investigation
Esophageal varices
History
any history of intravenous drug use that could lead to chronic hepatitis, chronic alcoholism, or cirrhosis should immediately arouse suspicions of portal hypertension and thus varices; variceal bleeds often lead to brisk hematemesis
Exam
stigmata of chronic liver disease are often present (e.g., jaundice, hepatomegaly, splenomegaly, ascites)
1st investigation
- esophagogastroduodenoscopy:
direct visualization of the varices
More
Other investigations
- CT scan/portal angiography:
can show collateral veins and recanalized umbilical vein
Esophagitis
History
often seen in the context of GERD; sometimes associated with dysphagia or odynophagia; history may include chronic heartburn; patients may mention a globus sensation; hoarseness can also be present; many patients who present with melena and who are suspected of peptic ulcer disease will be found to have esophagitis on endoscopy
Exam
reproducible pain can be demonstrated on swallowing
1st investigation
- esophagogastroduodenoscopy:
direct visualization of esophageal irritation/inflammation
Other investigations
Mallory-Weiss tear
History
classically, patients note hematemesis following retching or vomiting, but any increase in intraesophageal pressure (e.g., from seizures, hiccups, or straining) can cause a tear; some tears develop spontaneously; alcohol use, advanced age, and presence of hiatal hernias are common underlying features
Exam
bleeding is sometimes accompanied by midepigastric or retrosternal pain
1st investigation
- esophagogastroduodenoscopy:
direct visualization of intramural dissections
More
Other investigations
Uncommon
Boerhaave syndrome (spontaneous esophageal perforation)
History
classically, patients note retching or vomiting followed by severe retrosternal pain and/or epigastric pain; history of alcohol intake is common; other common symptoms and signs include dyspnea, tachypnea, cyanosis, sepsis, and shock
Exam
important to look for subcutaneous emphysema, which may be absent in some patients
1st investigation
- chest x-ray:
may reveal free mediastinal, peritoneal, or prevertebral air; pleural effusion with or without pneumothorax, widened mediastinum, and subcutaneous emphysema may be seen in late presentations
More
Other investigations
- pleural fluid amylase measurement:
indicative of esophageal rupture
- water-soluble contrast swallow study (Gastrografin):
helpful for localizing the lesion
- CT scan:
may be used as a confirmatory test; findings include esophageal wall edema, peri-esophageal fluid with or without bubbles, and widened mediastinum
Gastric varices
History
any history of intravenous drug use that could lead to chronic hepatitis, chronic alcoholism, or cirrhosis should immediately arouse suspicions of portal hypertension and thus varices; strongly associated with massive bleeding and rapid hemodynamic compromise
Exam
stigmata of chronic liver disease are often present (e.g., jaundice, hepatomegaly, splenomegaly, ascites)
1st investigation
- esophagogastroduodenoscopy:
classically, varices are seen in cardia of stomach
More
Other investigations
- CT scan/portal angiography:
collateral veins and recanalized umbilical vein
Arteriovenous malformations (AVMs)
History
usually painless and, as such, are often asymptomatic until they cause overt bleeding; associated with cirrhosis, end-stage renal disease, advanced age, and von Willebrand disease
Exam
often present with a nonfocal physical exam due to their frequently painless nature; patients can have chronic bleeding of which they are unaware
1st investigation
- esophagogastroduodenoscopy:
direct visualization of centrifugally expanding dilated capillaries
More
Other investigations
- CT angiography:
accumulation of vessels in the intestinal wall, early-filling vein, or enlarged supplying artery
More
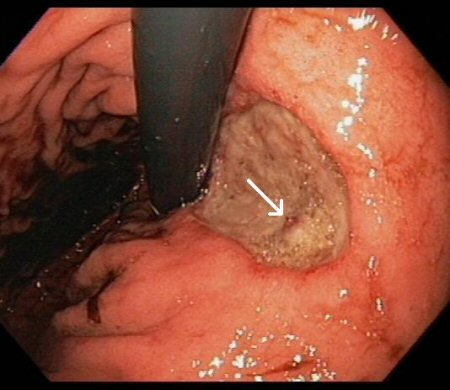
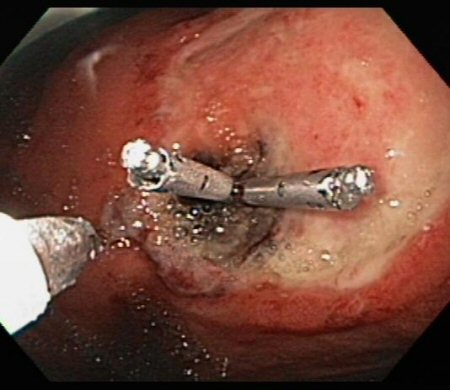
Dieulafoy lesions
History
often present painlessly; lesions are submucosal vessels that dive toward the gastric lumen and, through erosion, rupture and produce rapid blood loss; regarded as congenital arterial dysplasias but are most often symptomatic in men with alcohol histories, cardiovascular disease including hypertension, diabetes, or chronic kidney disease
Exam
often present with a nonfocal physical exam; the bleeding can be intermittent
1st investigation
- esophagogastroduodenoscopy (EGD):
direct visualization of lesion
More
Other investigations
- endoscopic ultrasound:
identification of lesion
More
Upper GI tumors
History
constitutional symptoms such as involuntary weight loss or night sweats
Exam
cachectic patient, sometimes with a palpable abdominal mass
1st investigation
- esophagogastroduodenoscopy and biopsy:
direct visualization of mass and positive histology
More
Aortoenteric fistulae (AEF)
History
often present with a "herald bleed" (an episode of self-limited bleeding before a massive bleed that can result in exsanguination), either in the form of hematochezia or of hematemesis; can also present with significant abdominal or back pain and fever; history of a vascular graft or aortic aneurysm should markedly heighten clinical suspicion
Exam
septic shock can occur; abdominal bruits or pulsatile masses can infrequently be detected
1st investigation
- esophagogastroduodenoscopy:
direct visualization of fistula
More
Other investigations
- abdominal CT, aortography, abdominal ultrasound:
contiguity of aorta with bowel
More
Coagulopathy
History
history may include liver disease, anticoagulant medication, genetic abnormalities of clotting (e.g., hemophilia, von Willebrand disease)
Exam
may be signs of underlying liver disease (e.g., jaundice, hepatomegaly, splenomegaly, ascites)
1st investigation
- clotting profile:
abnormal prothrombin time: prolonged INR
Other investigations
Use of this content is subject to our disclaimer