Etiology
Patients with UGIB can typically be separated into two groups: those with variceal lesions (either esophageal or gastric) and those with nonvariceal lesions (most commonly peptic ulcers). [Figure caption and citation for the preceding image starts]: Moderate to severe esophagitis with multiple linear, clean-based esophageal ulcersFrom the collection of Douglas G. Adler, MD [Citation ends].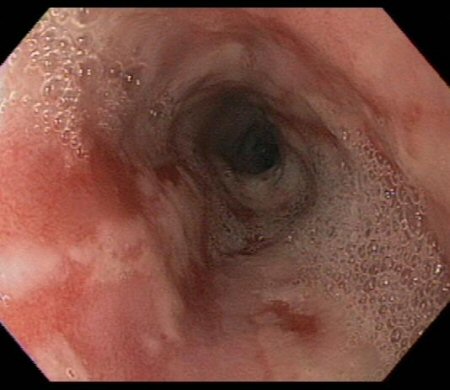 [Figure caption and citation for the preceding image starts]: Large gastric ulcer along the lesser curvature with a visible vessel in the ulcer bed (arrow)From the collection of Douglas G. Adler, MD [Citation ends].
[Figure caption and citation for the preceding image starts]: Large gastric ulcer along the lesser curvature with a visible vessel in the ulcer bed (arrow)From the collection of Douglas G. Adler, MD [Citation ends].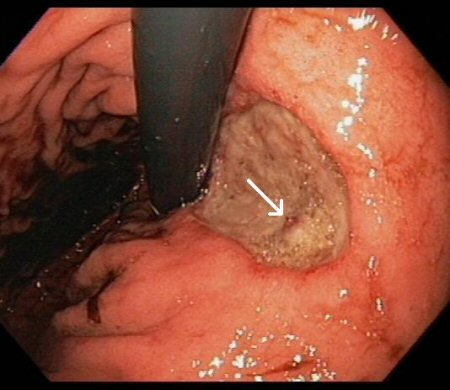 [Figure caption and citation for the preceding image starts]: Large gastric ulcer with large, protuberant visible vesselFrom the collection of Douglas G. Adler, MD [Citation ends].
[Figure caption and citation for the preceding image starts]: Large gastric ulcer with large, protuberant visible vesselFrom the collection of Douglas G. Adler, MD [Citation ends]. [Figure caption and citation for the preceding image starts]: Grade II esophageal varices in a patient with portal hypertensionFrom the collection of Douglas G. Adler, MD [Citation ends].
[Figure caption and citation for the preceding image starts]: Grade II esophageal varices in a patient with portal hypertensionFrom the collection of Douglas G. Adler, MD [Citation ends]. [Figure caption and citation for the preceding image starts]: Ulcer in the mid-esophagus with a visible vesselFrom the collection of Douglas G. Adler, MD [Citation ends].
[Figure caption and citation for the preceding image starts]: Ulcer in the mid-esophagus with a visible vesselFrom the collection of Douglas G. Adler, MD [Citation ends].
The most frequently encountered etiologies of UGIB are:[5][6]
Peptic ulcer disease (26% to 36%)
Gastritis/erosions (16% to 22%)
Esophagitis (17% to 24%)
No cause found (12% to 17%)
Erosive duodenitis (9% to 13%)
Varices (8% to 11%)
Portal hypertensive gastropathy (4.0% to 4.5%)
Mallory-Weiss tears (3.0% to 4.3%)
Malignancy (3.0% to 3.7%)
Other: including vascular ectasia and hemobilia (2.6%)
UGIB from malignant lesions is usually low-level and chronic, and only infrequently leads to acute bleeding.
It should be noted that varices should not be eliminated as a consideration in young pediatric patients; portal hypertension can be caused by vascular abnormalities and conditions other than alcoholic cirrhosis.
In most patients, likely causes of the bleeding can be ascertained through a thorough history and physical exam.
Use of this content is subject to our disclaimer