Etiology
Aspergillus is a ubiquitous environmental mold that grows in organic matter in the soil. The organism grows as a soil mycelium (filamentous form) and forms aerial hyphal stalks.[1] The conidia (spores) are about 2 to 10 micrometers in diameter. They are formed at the tips of the stalks (conidiophores) by asexual reproduction. Their hydrophobic nature aids in aerosolization.[1][17] Humans routinely inhale the aerosolized conidia. The conidia are promptly eliminated from the respiratory tract, or colonization or infection may occur, depending on the underlying local and general immune status of the individual.
Approximately 34 of 180 Aspergillus species are known to cause disease in humans. Aspergillus fumigatus is the most common pathogenic species, accounting for 50% to 70% of the aspergillosis syndromes. Increasingly, however, aspergillosis is caused by nonfumigatus species, including A flavus, A terreus, A niger, and A versicolor.[9][18]A niger is less pathogenic, perhaps due to its large conidia failing to reach the pulmonary alveoli.[18]A terreus, unlike the other species, is resistant to amphotericin B. Because of this, aspergillosis caused by A terreus has a poor prognosis, and occasionally is associated with positive blood cultures.[19] Rarely, the organism gains entry via direct cutaneous inoculation, particularly after trauma.[20]
In aspergilloma, A fumigatus remains the most common species. [Figure caption and citation for the preceding image starts]: Morphology of conidiophores and conidia of Aspergillus fumigatusFrom the collection of Dr P. Chandrasekar; used with permission [Citation ends].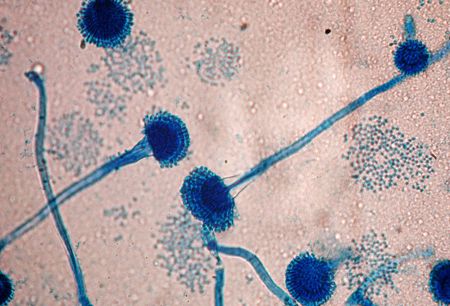
Pathophysiology
Upon inhalation of the conidia, the underlying immune defenses determine the fate of the organism. Immunocompetent people with intact ciliary clearance promptly eliminate the organism from the respiratory tract.[21] The early immune defense is provided by pulmonary macrophages that attempt to phagocytose and destroy the conidia.[21][22]
Invasive aspergillosis (IA)
IA mostly affects immunocompromised patients (e.g., stem cell transplant recipients, prolonged severe neutropenia, immunosuppressive therapy). It is rare in immunocompetent individuals. When conidia survive, germination leads to hyphae (filamentous form), which invade the pulmonary parenchyma. Polymorphonuclear leukocytes phagocytose the swollen conidia and hyphae.[22][23]
During invasion, interaction occurs between Aspergillus ligands and the pattern recognition receptors, including Toll-like receptors (TLR) and Dectin, on macrophages leading to the production of pro-inflammatory cytokines.[24] Fever is the resultant clinical manifestation.
TLR-4 polymorphisms in humans have been implicated as a risk factor of IA.[25] Angioinvasive hyphae gain entry and locally disseminate via the pulmonary microvasculature and cause thrombus formation and tissue infarction. Infected areas of lung with associated inflammation and pulmonary infarction contribute to clinical symptoms of cough, shortness of breath, and pleuritic chest pain. Lung function may worsen with increased areas of involvement.
Dissemination from the lung via the hematogenous route may commonly occur into the brain and skin, leading to tissue infarction at those sites. Virtually all body sites, including the heart, kidney, liver/spleen, bone, and gastrointestinal tract, may be affected.[2] Direct invasion from the paranasal sinus cavity into the orbit, sphenoidal sinus, and brain parenchyma may also occur.[2]
Chronic pulmonary aspergillosis (CPA)
CPA generally affects people who are not immunocompromised, but have underlying respiratory pathology with cavitation, for example, tuberculosis.[4][26] Aspergillus colonizes and grows in the cavities, damaging the pulmonary parenchyma. Aspergilloma may form in the cavities.
In chronic cavitary pulmonary aspergillosis (CCPA), disease progression is slow, involving one or more cavities, with or without aspergilloma, and with pleural fibrosis.[4][26]
Subacute invasive aspergillosis (SAIA) may develop in some patients who are immunocompromised. Hyphae invade lung parenchyma with necrosis and inflammation. Disease progression is more rapid, with earlier development of symptoms.[3][4][26]
Chronic fibrosing pulmonary aspergillosis (CFPA) results from untreated CCPA, with extensive pulmonary fibrosis and loss of lung function.[3][4]
Aspergilloma (fungal ball) consist of Aspergillus mycelia, inflammatory cells, fibrin, mucus, and tissue debris.[4] May form in pulmonary cavities. The growth of Aspergillus on the walls of the cavity is facilitated by inadequate drainage. Bleeding is uncommon; however, severe hemoptysis may sometimes occur secondary to erosion of bronchial blood vessels lining the cavity, and mechanical friction of the fungal ball against the blood vessels.[27]
Classification
Types of aspergillosis
Invasive aspergillosis (IA)[1][2]
Invasive sino-pulmonary aspergillosis: inhalation of conidia most commonly results in sinus and pulmonary involvement.
Disseminated aspergillosis: in profoundly immunocompromised patients, focal disease may spread to multiple organ sites.
Single-organ IA: common sites include skin (via trauma), bone, and brain.
Chronic pulmonary aspergillosis[3]
There are five different clinical forms of chronic pulmonary aspergillosis (with some overlapping):
Chronic cavitary pulmonary aspergillosis (previously termed complex aspergilloma)
Aspergillus colonizes and grows in pulmonary cavities. Aspergilloma may grow in the cavities.
Chronic fibrosing pulmonary aspergillosis
Occurs following untreated chronic cavitary pulmonary aspergillosis.
Aspergilloma (fungal ball)
Consists of mycelia, inflammatory cells, fibrin, mucus, and tissue debris. Occurs in pre-existing lung cavities. [Figure caption and citation for the preceding image starts]: Aspergilloma in a pre-existing tuberculous lung cavityFrom the collection of Dr P. Chandrasekar; used with permission [Citation ends].

A single aspergilloma in a single cavity, with no progression and few or no symptoms is termed simple aspergilloma.
Subacute invasive aspergillosis (previously termed chronic necrotizing aspergillosis)
An indolent destructive process due to invasion by Aspergillus.
Usually seen in patients with lung disease such as COPD, pneumoconiosis, or cystic fibrosis, and in patients with mild immunosuppression.
Aspergillus nodule
Nodules do not usually form cavities; an unusual form of aspergillosis.
Allergic bronchopulmonary aspergillosis[1][2]
Hypersensitivity reaction to Aspergillus antigens, mostly due to A fumigatus.
Typically seen in patients with long-standing asthma or cystic fibrosis.
Use of this content is subject to our disclaimer