Tests
1st tests to order
CBC
Test
All patients should have a CBC on initial presentation.[70][71]
Anemia can be due to chronic inflammation, chronic blood loss, iron malabsorption, and/or malabsorption of vitamin B12 or folate.
Leukocytosis is associated with acute or chronic inflammation, abscess, or corticosteroid treatment.
Thrombocytosis is a useful marker of active inflammation.
Result
anemia; leukocytosis; may be thrombocytosis
iron studies (serum iron, serum ferritin, total iron binding capacity [TIBC], transferrin saturation)
Test
Patients should undergo serum iron studies.[71][72]
Patients with inflammatory bowel disease who are malnourished or at risk of malnutrition should have relevant screening blood tests to assess for macronutrient and micronutrient deficiencies.[70]
Iron deficiency may be associated with gastrointestinal bleeding or malabsorption of iron.
Result
normal, or may demonstrate changes consistent with iron deficiency
serum vitamin B12
Test
B12 levels should be checked.[70]
Deficiency may be secondary to malabsorption. Patients with inflammatory bowel disease who are malnourished or at risk of malnutrition should have relevant screening blood tests to assess for macronutrient and micronutrient deficiencies.[70]
Deficiency most common in ileocecal Crohn disease and post-ileocecal resection.
Result
may be normal or low
serum folate
Test
Serum folate levels should be checked.[70]
Deficiency may be secondary to malabsorption. Patients with inflammatory bowel disease who are malnourished or at risk of malnutrition should have relevant screening blood tests to assess for macronutrient and micronutrient deficiencies.[70]
Result
may be normal or low
comprehensive metabolic panel (CMP)
Test
All patients should have a CMP on initial presentation.
Hypomagnesemia and hypophosphatemia can be caused by diarrhea and hypoprothrombinemia may reflect vitamin K deficiency.
Result
hypoalbuminemia, hypocholesterolemia, hypocalcemia
CRP and erythrocyte sedimentation rate (ESR)
Test
All patients should have CRP and ESR on initial presentation.[70][71]
Inflammatory markers correlate closely with the activity of Crohn disease (CD).[94]
In patients with CD with moderate to severe symptoms, elevated fecal calprotectin or serum CRP suggests endoscopic activity and endoscopic evaluation can be avoided.[66]
Result
elevated
stool testing
Test
Testing for Clostridium difficile toxin is indicated especially if history of recent antibiotic use, as C difficile infection is associated with increased short- and long-term mortality in patients with inflammatory bowel disease.[9][73]
Result
absence of infectious elements seen on microscopy or culture
Yersinia enterocolitica serology
Test
Important to exclude Y enterocolitica, a bowel pathogen that causes an acute ileitis.[74] May be ordered in the acute setting.
Result
negative
plain abdominal x-ray
Test
Plain abdominal x-rays may be part of the initial tests ordered in the acute setting. They are not diagnostic of Crohn disease, but may be suggestive and help in assessing severity. Bowel loop distension and pneumoperitoneum may be visible.
Result
small bowel or colonic dilation; calcification; sacroiliitis; intra-abdominal abscesses
MRI abdomen/pelvis
Test
Patients who are able to tolerate oral contrast are candidates for CT enterography or magnetic resonance (MR) enterography.[75] MR enterography characteristics (sensitivity 77% to 82%, specificity 80% to 100%) are similar to those of CT enterography, but availability may be limited.[75]
MR imaging has also been shown to yield robust diagnostic accuracy in detecting fibrotic strictures, distinguishing between fibrotic and inflammatory strictures, and evaluating stricture severity in patients with Crohn disease.[76]
Guidelines suggest that MR enterography should be the test of choice as it does not expose the patient to ionizing radiation.[70][71][77][Figure caption and citation for the preceding image starts]: CT scan demonstrating thickening of the terminal ileum in a patient with Crohn disease exacerbationProvided by Drs Wissam Bleibel, Bishal Mainali, Chandrashekhar Thukral, and Mark A. Peppercorn, the previous authors of this topic [Citation ends]. [Figure caption and citation for the preceding image starts]: CT scan demonstrating thickening of the terminal ileum in a patient with Crohn disease exacerbationProvided by Drs Wissam Bleibel, Bishal Mainali, Chandrashekhar Thukral, and Mark A. Peppercorn, the previous authors of this topic [Citation ends].
[Figure caption and citation for the preceding image starts]: CT scan demonstrating thickening of the terminal ileum in a patient with Crohn disease exacerbationProvided by Drs Wissam Bleibel, Bishal Mainali, Chandrashekhar Thukral, and Mark A. Peppercorn, the previous authors of this topic [Citation ends].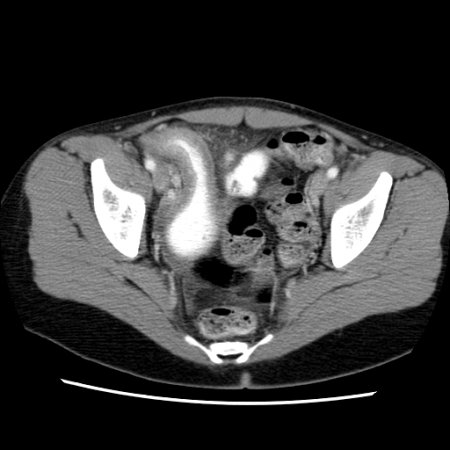
Result
skip lesions, bowel wall thickening, surrounding inflammation, abscess, fistulae
CT abdomen
Test
Patients who are able to tolerate oral contrast are candidates for CT enterography or magnetic resonance (MR) enterography.[75] CT enterography is sensitive (75% to 90%), and can assess for alternative diagnoses, and potential complications of Crohn disease (e.g., obstruction, abscess, fistula).[75]
Guidelines suggest that MR enterography should be the test of choice as it does not expose the patient to ionizing radiation.[70][71][77]
If CT is indicated, do not order unenhanced CT alongside intravenous contrast-enhanced CT because the addition of unenhanced CT does not provide additional diagnostic information and exposes patients to unnecessary radiation.[75][79][Figure caption and citation for the preceding image starts]: CT scan demonstrating thickening of the terminal ileum in a patient with Crohn disease exacerbationProvided by Drs Wissam Bleibel, Bishal Mainali, Chandrashekhar Thukral, and Mark A. Peppercorn, the previous authors of this topic [Citation ends]. [Figure caption and citation for the preceding image starts]: CT scan demonstrating thickening of the terminal ileum in a patient with Crohn disease exacerbationProvided by Drs Wissam Bleibel, Bishal Mainali, Chandrashekhar Thukral, and Mark A. Peppercorn, the previous authors of this topic [Citation ends].
[Figure caption and citation for the preceding image starts]: CT scan demonstrating thickening of the terminal ileum in a patient with Crohn disease exacerbationProvided by Drs Wissam Bleibel, Bishal Mainali, Chandrashekhar Thukral, and Mark A. Peppercorn, the previous authors of this topic [Citation ends].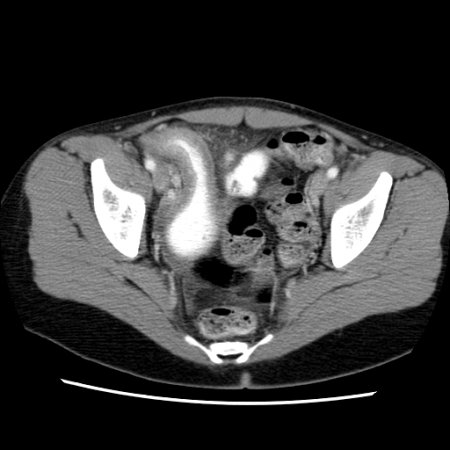
Result
skip lesions, bowel wall thickening, surrounding inflammation, abscess, fistulae
Tests to consider
abdominal and pelvic ultrasonography
Test
Ultrasound of the abdomen and pelvis may be considered.[70][71][75]
Sensitivity and specificity range from 75% to 94% and 67% to 100%, respectively.[75] Ultrasound may facilitate detection of extramural complications, detection and evaluation of stenotic strictures, and monitoring of disease course.[71][80]
Obesity, overlying bowel gas, and guarding (in the acutely unwell patient) may preclude adequate compression of the ultrasound probe.[81]
An accuracy comparable to CT or MR modalities has been noted for visualization of ileum when intestinal ultrasound is performed by trained practitioners.[81] Limitations of this technique include limited visualization of the stomach, esophagus, and rectum and inability for performing interventional procedure.[81]
Result
bowel wall thickening, surrounding inflammation, abscess; tubo-ovarian abscess
ileocolonoscopy
Test
Ileocolonoscopy and imaging studies are complementary in the diagnosis of Crohn disease (CD).[70][71][75]
Mucosal changes suggestive of CD include mucosal nodularity, erythema, edema, ulcerations, friability, stenosis, and the identification of fistulous tract opening.[71]
Lesions are discontinuous, with intermittent areas of normal-appearing bowel (skip lesions). [Figure caption and citation for the preceding image starts]: Endoscopic view of Crohn ileitisProvided by Drs Wissam Bleibel, Bishal Mainali, Chandrashekhar Thukral, and Mark A. Peppercorn, the previous authors of this topic [Citation ends].
Evidence of a normal rectum and isolated involvement of the terminal ileum support the diagnosis.
Result
aphthous ulcers, hyperemia, edema, cobblestoning, skip lesions
tissue biopsy
Test
Segmental colonic and ileal biopsies should be obtained to assess for microscopic evidence of Crohn disease (CD).[70] The microscopic features that help distinguish ulcerative colitis and CD include granulomas, architectural change, and disease distribution.[82] Granulomatous inflammation is, however, reported in a minority of patients with CD (30% to 50%); it is not required for diagnosis.[71][82][Figure caption and citation for the preceding image starts]: Significant inflammation in the colonic wall, widening of submucosa, and dense lymphoid aggregates in the submucosaProvided by Drs Wissam Bleibel, Bishal Mainali, Chandrashekhar Thukral, and Mark A. Peppercorn, the previous authors of this topic [Citation ends].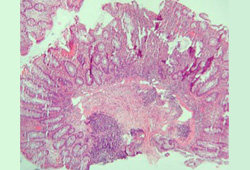 [Figure caption and citation for the preceding image starts]: Granulomas in a patient with Crohn disease; note the aggregate of epithelioid histiocytesProvided by Drs Wissam Bleibel, Bishal Mainali, Chandrashekhar Thukral, and Mark A. Peppercorn, the previous authors of this topic [Citation ends].
[Figure caption and citation for the preceding image starts]: Granulomas in a patient with Crohn disease; note the aggregate of epithelioid histiocytesProvided by Drs Wissam Bleibel, Bishal Mainali, Chandrashekhar Thukral, and Mark A. Peppercorn, the previous authors of this topic [Citation ends].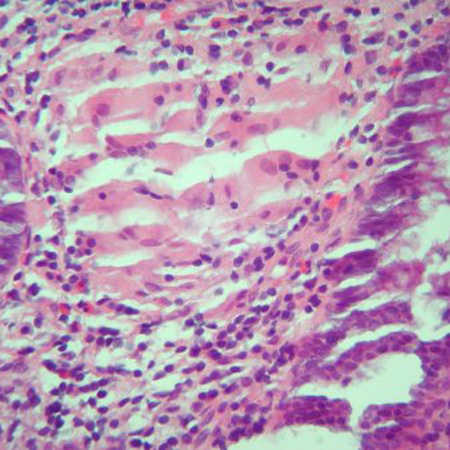 [Figure caption and citation for the preceding image starts]: Cryptitis and crypt abscess with morphologic distortion of the crypts accompanied by inflammation and abundant lymphatic and plasma cellsProvided by Drs Wissam Bleibel, Bishal Mainali, Chandrashekhar Thukral, and Mark A. Peppercorn, the previous authors of this topic [Citation ends].
[Figure caption and citation for the preceding image starts]: Cryptitis and crypt abscess with morphologic distortion of the crypts accompanied by inflammation and abundant lymphatic and plasma cellsProvided by Drs Wissam Bleibel, Bishal Mainali, Chandrashekhar Thukral, and Mark A. Peppercorn, the previous authors of this topic [Citation ends].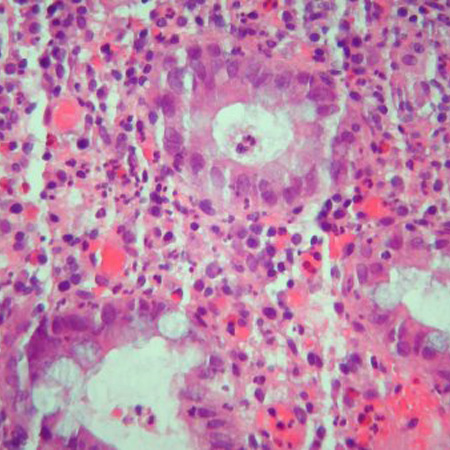 [Figure caption and citation for the preceding image starts]: Cryptitis and crypt abscess with morphologic distortion of the crypts accompanied by inflammation and abundant lymphatic and plasma cellsProvided by Drs Wissam Bleibel, Bishal Mainali, Chandrashekhar Thukral, and Mark A. Peppercorn, the previous authors of this topic [Citation ends].
[Figure caption and citation for the preceding image starts]: Cryptitis and crypt abscess with morphologic distortion of the crypts accompanied by inflammation and abundant lymphatic and plasma cellsProvided by Drs Wissam Bleibel, Bishal Mainali, Chandrashekhar Thukral, and Mark A. Peppercorn, the previous authors of this topic [Citation ends].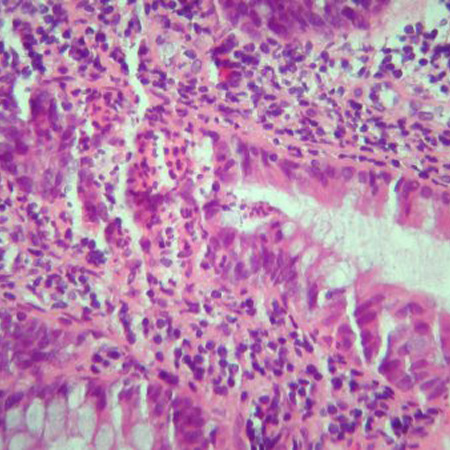
Biopsies of uninvolved mucosa help to identify the extent of histologic disease.[71] If tuberculosis is being considered, tissue from ileocecal biopsies can be tested for Mycobacterium tuberculosis.[69]
Result
mucosal bowel biopsies demonstrate transmural involvement with noncaseating granulomas
esophagogastroduodenoscopy
Test
Esophagogastroduodenoscopy (upper gastrointestinal [GI] endoscopy) is not routinely required as part of the diagnostic evaluation, but may be performed in patients with upper GI signs and symptoms.[70][71]
Eesophagogastroduodenoscopy with biopsy is helpful in differentiating Crohn disease from peptic ulcer disease in patients with upper GI tract symptoms.
Result
aphthous ulcers; mucosal inflammation
wireless capsule endoscopy
Test
Can be used as an alternative to MR imaging to assess small bowel involvement. Visualizes the small bowel and may detect suggestive lesions not visible by other small bowel studies. Capsule endoscopy can be used to monitor mucosal healing and postoperative recurrence in selected patients.[95] It is a safe and useful investigation in children.
Patency capsule evaluation is advised prior to endoscopy to reduce the risk of capsule retention if there is a possibility of strictures.[71] Capsule endoscopy is contraindicated in patients with small bowel strictures or stenosis.[96]
Result
aphthous ulcers; hyperemia; edema; cobblestoning; skip lesions
fecal calprotectin
Test
Noninvasive marker of bowel inflammation.[9][83][84] Fecal calprotectin is released into feces when neutrophils gather at the site of any gastrointestinal tract inflammation.
In patients ages <60 years having lower gastrointestinal symptoms and normal initial workup, fecal calprotectin testing can be performed to exclude causes of colonic inflammation. However, in patients ages >60 years with suspected colorectal cancer, fecal calprotectin testing should be interpreted with caution.[85]
Fecal calprotectin can help to differentiate inflammatory bowel disease from irritable bowel syndrome.[71] Fecal calprotectin is not specific for Crohn disease (CD) and can be increased in the stool in other gut pathologies (e.g., infectious gastroenteritis, diverticulitis, or colorectal cancer) or in patients on nonsteroidal anti-inflammatory drugs [NSAIDs] and aspirin).[71][85] This lack of specificity limits their diagnostic role.
Fecal calprotectin is widely used, particularly in the primary care setting, as a “rule out” test where inflammatory bowel disease (IBD) is unlikely in the presence of a normal calprotectin.
In IBD it is used to monitor relapse in patients with quiescent IBD, and for detection and monitoring of disease activity in symptomatic patients, potentially avoiding invasive and resource-intensive endoscopic monitoring.[66][70][86][87][88] A fecal calprotectin value of <150 micrograms/g and normal CRP suggests no active inflammation in patients in symptomatic remission; endoscopic assessment can be avoided in such patients. However, elevated biomarker levels in these patients warrant an endoscopic evaluation.[66]
In patients with CD with moderate to severe symptoms, elevated fecal calprotectin or serum CRP suggests endoscopic activity and endoscopic evaluation can be avoided.[66]
Result
may be elevated
Emerging tests
serologic markers
Test
Research is focused on antiglycan antibodies (e.g., anti-Saccharomyces cerevisiae [ASCA], anti-laminaribiose [ALCA], anti-chitobioside [ACCA], anti-laminarin [anti-L], anti-chitin [anti-C]) and antibodies to microbial antigens (anti-outer membrane porin C [anti-OmpC], anti-Cbir1 flagellin, anti-I2, and p-ANCA).[71]
Antiglycan antibodies are more prevalent in Crohn disease (CD) than in ulcerative colitis, but have a low sensitivity.[71]
Routine use of serologic markers of inflammatory bowel disease to establish the diagnosis of CD is not recommended.[71]
ASCA may be of prognostic value in children with CD.[97][98]
Result
positive antiglycan antibodies
Use of this content is subject to our disclaimer