Tests
1st tests to order
CBC with differential
peripheral blood smear
Test
Peripheral blood smear will show cytopenias (most commonly anemia) and dysplasia.[16]
Anemia is usually normochromic or macrocytic.
May see hypogranular and hypolobulated granulocytes (pseudo-Pelger-Huet anomaly).[62][Figure caption and citation for the preceding image starts]: Blood film showing normal neutrophil (right) and dysplastic neutrophil with agranular cytoplasm and hypolobated nucleusImage used with permission from BMJ 1997;314:883 [Citation ends].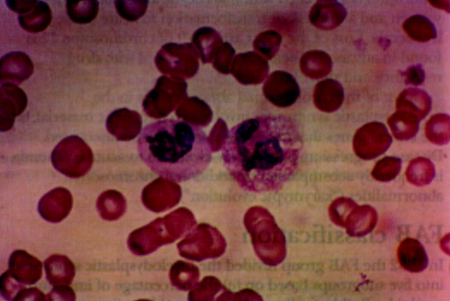
Result
cytopenias; normochromic or macrocytic red cells; dysplasia; hypogranular and hypolobulated granulocytes (pseudo-Pelger-Huet anomaly)
reticulocyte count
Test
Often low in MDS.[50]
Inadequate reticulocyte response for degree of anemia; if an adequate response is present, other diagnoses are more likely.
Result
inappropriately normal or low
red blood cell folate
Test
Used to rule out folate deficiency as cause of anemia.
Result
normal
serum vitamin B12
Test
Used to rule out vitamin B12 deficiency as cause of anemia.
Result
normal
iron studies
Test
Serum iron, total iron-binding capacity, ferritin used to rule out iron deficiency.
Result
normal
bone marrow aspiration with iron stain
Test
A diagnosis of MDS can be made in a patient with persistent cytopenia in the presence of one of the following three criteria: significant bone marrow dysplasia (≥10% in one or more of three major bone marrow lineages); blasts in the peripheral blood and/or bone marrow (<20%); or a clonal cytogenetic abnormality or somatic mutation.[1][2][11] Biologic features are more important than a strict blast cutoff value.[15] Patients with blasts ≥20% should be assessed for acute myeloid leukemia. (See Acute myeloid leukemia)
Prussian blue iron staining of bone marrow aspirate can show ringed sideroblasts - abnormal erythroid precursor cells that have granules around the nucleus.
May need to repeat to assess: transformation into AML; persistence of morphologic abnormalities (as other conditions such as vitamin B12 deficiency and infections can cause transient dysplastic abnormalities).
[Figure caption and citation for the preceding image starts]: Large mononuclear megakaryocyte in bone marrow of patient with MDS-del(5q)Image used with permission from BMJ 1997;314:883 [Citation ends].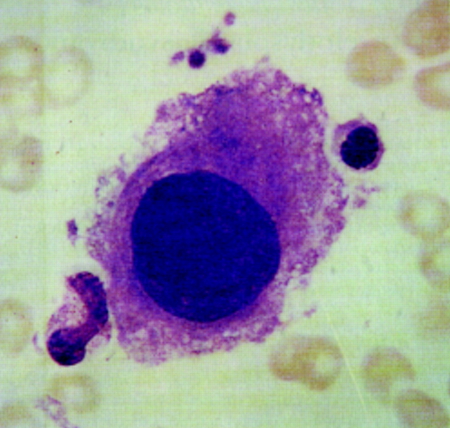
Result
dysplasia (≥10% in one or more of three major bone marrow lineages); ringed sideroblasts; bone marrow blasts (<20%)
bone marrow core biopsy
Test
Can assess overall bone marrow cellularity and architecture and help differentiate MDS from myeloproliferative disorder (reticulin deposits, fibrosis). Hypocellular marrow may be seen in some patients with MDS, but this is rare.
May need to repeat to assess: transformation into AML; persistence of morphologic abnormalities (as other conditions such as vitamin B12 deficiency and infections can cause transient dysplastic abnormalities).
Result
usually hypercellular marrow; rarely hypocellular marrow
genetic testing
Test
Genetic testing for MDS-associated cytogenetic abnormalities (e.g., -5, del(5q), -7, del(7q), del(11q), del(12p), -17, del(17p), del(20q)) and somatic mutations (e.g., DNMT3A, TET2, ASXL1, TP53, SF3B1) informs the diagnosis and prognostic risk stratification.[11][15]
The presence of certain cytogenetic abnormalities or somatic mutations (e.g., -7/del(7q), del(5q), or SF3B1) may establish a diagnosis without dysplasia.[1][2]
Genetic testing may be carried out on peripheral blood if bone marrow testing is not possible.
Patients with significant dysplasia who do not have a clonal cytogenetic abnormality or somatic mutation should undergo further evaluation to exclude a nonmalignant cause of dysplasia.
Result
MDS-associated cytogenetic abnormalities (e.g., -5, del(5q), -7, del(7q), del(11q), del(12p), -17, del(17p), del(20q)); MDS-associated somatic mutations (e.g., DNMT3A, TET2, ASXL1, TP53, SF3B1)
Investigations to avoid
Tests to consider
viral serology
Test
Testing for viral infection (e.g., HIV; hepatitis B, C, and E; cytomegalovirus; parvovirus) can be carried out if there are risk factors for prior exposure.[11][15][16]
HIV infection can cause dysplastic bone marrow changes that are similar to those seen in MDS.[51]
Result
may be positive for viral infection
serum erythropoietin
lactate dehydrogenase
HLA typing
Test
Useful for candidates for hematopoietic stem cell transplantation, or those requiring extensive platelet transfusions.[54]
Result
varies
flow cytometry
Test
Can be performed on bone marrow samples to support a diagnosis of MDS (by identifying dysplastic features and blasts).[52]
May be used (alongside STAT3 mutation testing) for the evaluation of a concurrent paroxysmal nocturnal hemoglobinuria clone, and possible large granular lymphocytic leukemia.[3][15]
Result
dysplasia (≥10% in one or more of three major bone marrow lineages); bone marrow blasts (<20%)
Use of this content is subject to our disclaimer