Approach
Clinical diagnosis is based on the appearance of pearly papules with a central dell.[Figure caption and citation for the preceding image starts]: Extensive molluscum lesions on the flank of a young child; lesions are flesh to pearly colored with central dellsFrom the collection of Dr Nanette Silverberg [Citation ends]. Some of the lesions may be inflamed with surrounding erythema. Often lesions are excoriated and surrounded by dermatitis, similar to atopic dermatitis.[Figure caption and citation for the preceding image starts]: Molluscum on the arm of a child with atopic dermatitis demonstrating pearly papules with a central dell and areas of excoriation and erythema due to inflammationReproduced with permission from dermnetnz.org [Citation ends].
Some of the lesions may be inflamed with surrounding erythema. Often lesions are excoriated and surrounded by dermatitis, similar to atopic dermatitis.[Figure caption and citation for the preceding image starts]: Molluscum on the arm of a child with atopic dermatitis demonstrating pearly papules with a central dell and areas of excoriation and erythema due to inflammationReproduced with permission from dermnetnz.org [Citation ends].
In small children, the lesions may be small enough to mimic milia, small cysts created by blockage of sweat glands. In the genital region, particularly the intergluteal cleft, the central dell may be imperceptible and thus the lesions may mimic condyloma acuminatum. The smooth, pearly appearance of the lesions gives away their true etiology. Immunocompromised patients may have large molluscum or widespread molluscum with >20 papules.
An online tool has been developed to help parents diagnose the condition in their children, and has been shown to have a sensitivity of over 95% and specificity of over 90%.[18] Molluscum contagiosum diagnostic tool for parents (MCDTP) Opens in new window
History
Many children acquire lesions from close contacts, so an infected sibling or close friend provides a strong clue. Onset occurs within 6 weeks of contact in most cases; thus, there appears to be a peak in onset in August and September, reflecting swimming pool exposures. Maternal transmission to child post delivery has also been reported.[2] Any history of recent sexual contact is also important information.
Children and adults with atopic dermatitis are much more likely to present with molluscum, and presentation should trigger an evaluation of current eczema management.[4] Persistent or atypical presentation in adults could be the first presentation of immunocompromise, and this should be evaluated. Patients who are HIV positive are more likely to present with lesions on the face or anogenital region and therefore should be evaluated with a full sexual health history.[12][Figure caption and citation for the preceding image starts]: Molluscum contagiosum on the face of an adult, which may be the presenting sign of HIV infection as in this caseMaybury C et al. Peri-oral papules. BMJ. 2013 Feb 11;346:f750; used with permission [Citation ends].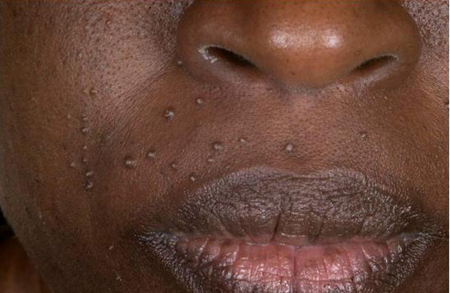
Investigations
In the majority of cases, molluscum can be clinically diagnosed.
Dermoscopy may facilitate diagnosis by revealing a central, polylobular, white-yellow, structureless area, surrounded by vessels in a crown pattern.[12]
[Figure caption and citation for the preceding image starts]: Dermatoscopic findings of Molluscum contagiosum. Red arrows indicate white-to-yellow polylobular structures; blue arrows: crown vessels. (Polarized-light dermoscopy, original magnification 10x)Clinical, Cosmetic and Investigational Dermatology 2019:12 373-381. Originally published by and used with permission from Dove Medical Press Ltd. [Citation ends].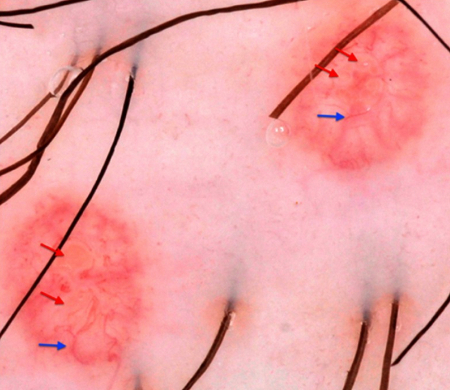
Routine screening for a full panel of sexually transmitted infections is recommended for patients presenting with anogenital molluscum.
Widespread or persistent molluscum should prompt consideration of immunocompromise. Investigation is mandated, including complete blood count and viral screen. Examine for presence of underlying inflammatory skin disease.[12]
On occasion, lesions in children in the genital region look like condyloma. Curettage biopsy can be used to confirm diagnosis (particularly if sexual abuse is suspected). In rare cases, curette or tangential excision and biopsy can aid or confirm diagnosis. Inflamed molluscum can abscess with sterile neutrophilic infiltrates picked up on Gram stain; however, bacterial culture of such abscesses may reveal a true bacterial superinfection with flora similar to that of impetigo.
Use of this content is subject to our disclaimer