Case history
Case history
A 75-year-old man presents with an acute stroke including right-sided paralysis and altered mental status. Two days after admission, he notes cough and right-sided pleuritic chest pain. He is tachycardic, tachypneic, and has a fever of 102°F (38.8°C). His breath is foul smelling. Examination reveals egophony, decreased breath sounds, and dullness to percussion in the right lower lung field.[Figure caption and citation for the preceding image starts]: Early ill-defined opacities of the right upper lobe above the minor fissure consistent with early changes of aspiration pneumoniaUsed with kind permission from Roy Hammond, MD [Citation ends].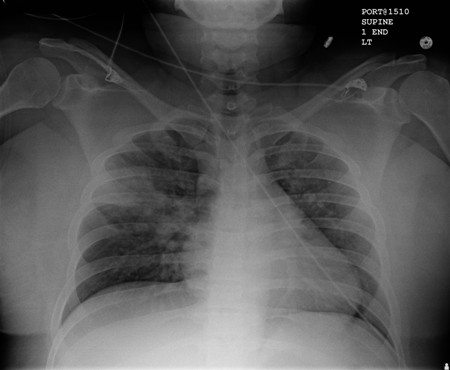 [Figure caption and citation for the preceding image starts]: Increased opacification of the right perihilar region and superior segment of the right lower and upper lobes consistent with worsening aspiration pneumoniaUsed with kind permission from Roy Hammond, MD [Citation ends].
[Figure caption and citation for the preceding image starts]: Increased opacification of the right perihilar region and superior segment of the right lower and upper lobes consistent with worsening aspiration pneumoniaUsed with kind permission from Roy Hammond, MD [Citation ends].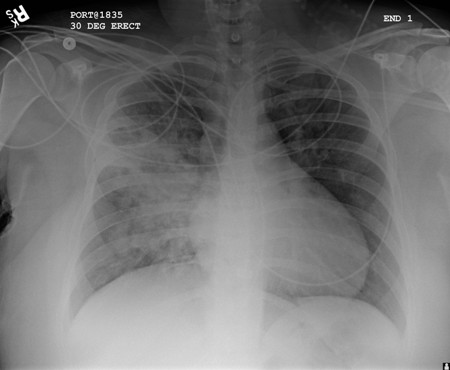
Other presentations
Aspiration pneumonia is more common in older people who have comorbid conditions that may lead to alteration in mental status. This population includes patients with swallowing dysfunction, disruption of the gastroesophageal junction, or anatomic abnormalities of the upper airway or digestive tract. Additionally, patients undergoing upper airway or endoscopic procedures are at risk. Any situation in which there is altered mental status and loss of airway protection mechanisms, such as seizure, places the patient at risk of aspiration. Nasogastric tube or percutaneous endoscopic gastrostomy provide no protection from colonized oral secretions and increase the risk for aspiration.[8]
Use of this content is subject to our disclaimer