Aspiration pneumonia is diagnosed based on clinical signs or symptoms of pneumonia in a person with a history or risk factors for aspiration.
Sputum or tracheal Gram stain reveals mixed flora.
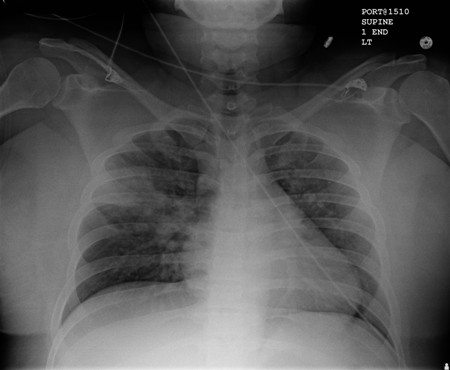
Infection usually involves the dependent lung lobe.
Complications of disease include lung abscess and empyema.
Aspiration pneumonia results from inhalation of oropharyngeal contents into the lower airways that leads to lung injury and resultant bacterial infection. It commonly occurs in patients with altered mental status who have an impaired gag or swallowing reflex.
The bacteriology and presentation of aspiration pneumonia have changed over the past five decades. Older studies characterized an anaerobic pleuropulmonary syndrome, with necrotizing pneumonia, putrid sputum, and abscess formation as a result of the presence of anaerobic bacteria.[1]Bartlett JG, Gorbach SL, Finegold SM. The bacteriology of aspiration pneumonia. Am J Med. 1974 Feb;56(2):202-7.
http://www.ncbi.nlm.nih.gov/pubmed/4812076?tool=bestpractice.com
More recent literature suggests that aspiration pneumonia resulting from anaerobic bacteria is less common than previously thought, and often is not distinct from pneumonia caused by aerobic bacteria.[2]El-Solh AA, Pietrantoni C, Bhat A, et al. Microbiology of severe aspiration pneumonia in institutionalized elderly. Am J Respir Crit Care Med. 2003 Jun 15;167(12):1650-4.
https://www.atsjournals.org/doi/full/10.1164/rccm.200212-1543OC
http://www.ncbi.nlm.nih.gov/pubmed/12689848?tool=bestpractice.com
[3]Marik PE. Pulmonary aspiration syndromes. Curr Opin Pulm Med. 2011 May;17(3):148-54.
http://www.ncbi.nlm.nih.gov/pubmed/21311332?tool=bestpractice.com
There is debate on whether aspiration pneumonia represents a distinct entity from typical pneumonia, or whether it is one end of the spectrum of pneumonia syndromes.[4]Lanspa MJ, Peyrani P, Wiemken T, et al. Characteristics associated with clinician diagnosis of aspiration pneumonia: a descriptive study of afflicted patients and their outcomes. J Hosp Med. 2015 Feb;10(2):90-6.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4310822
http://www.ncbi.nlm.nih.gov/pubmed/25363892?tool=bestpractice.com
[5]Taylor JK, Fleming GB, Singanayagam A, et al. Risk factors for aspiration in community-acquired pneumonia: analysis of a hospitalized UK cohort. Am J Med. 2013 Nov;126(11):995-1001.
http://www.ncbi.nlm.nih.gov/pubmed/24054176?tool=bestpractice.com
[6]Mandell LA, Niederman MS. Aspiration pneumonia. N Engl J Med. 2019 Feb 14;380(7):651-663.
http://www.ncbi.nlm.nih.gov/pubmed/30763196?tool=bestpractice.com
There is no definition that separates patients with aspiration pneumonia from typical pneumonia.[7]Metlay JP, Waterer GW, Long AC, et al. Diagnosis and treatment of adults with community-acquired pneumonia. An official clinical practice guideline of the American Thoracic Society and Infectious Diseases Society of America. Am J Respir Crit Care Med. 2019 Oct 1;200(7):e45-e67.
https://www.atsjournals.org/doi/full/10.1164/rccm.201908-1581ST
http://www.ncbi.nlm.nih.gov/pubmed/31573350?tool=bestpractice.com
Typical pneumonia can also occur from microaspiration of oronasopharyngeal contents, and can present with similar microbiology and clinical course as aspiration pneumonia, as well as needing similar treatment.