Nasopharyngeal cancer (NPC) arises from epithelial cells within the lymphocyte-rich nasopharyngeal mucosa.
Worldwide, NPC is a rare cancer with such a unique geographic distribution that patient ethnicity alone can point toward a diagnosis of NPC. NPC has an especially high incidence in southern China and southeast Asia (>70% of new cases) where the predominant form of NPC is the undifferentiated (nonkeratinizing) type and associated with Epstein-Barr virus infection.[1]Chen YP, Ismaila N, Chua MLK, et al. Chemotherapy in combination with radiotherapy for definitive-intent treatment of stage II-IVA nasopharyngeal carcinoma: CSCO and ASCO guideline. J Clin Oncol. 2021 Mar 1;39(7):840-59.
https://ascopubs.org/doi/10.1200/JCO.20.03237?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub%20%200pubmed
http://www.ncbi.nlm.nih.gov/pubmed/33405943?tool=bestpractice.com
[7]Chen YP, Chan ATC, Le QT, et al. Nasopharyngeal carcinoma. Lancet. 2019 Jul;394(10192):64-80.
http://www.ncbi.nlm.nih.gov/pubmed/31178151?tool=bestpractice.com
NPC is most frequently diagnosed after patients present with a neck mass from lymph node metastases, including in the posterior triangle/level V of the neck, rather than with symptoms associated with the primary tumor.
Compared with smoking-associated head and neck cancers, NPC tends to affect a younger population and is more responsive to systemic therapy and radiation therapy.[18]Chan AT, Teo PM, Leung TW, et al. The role of chemotherapy in the management of nasopharyngeal carcinoma. Cancer. 1998 Mar 15;82(6):1003-12.
http://www.ncbi.nlm.nih.gov/pubmed/9506343?tool=bestpractice.com
History
The patient may report epistaxis, nasal obstruction, unilateral otitis media with effusion (serous otitis media), tinnitus, or impaired hearing in one ear. Aural symptoms are common in people presenting with NPC (62%) and should raise suspicion of NPC, particularly in an Asian patient.[4]Lee AW, Foo W, Law SC, et al. Nasopharyngeal carcinoma: presenting symptoms and duration before diagnosis. Hong Kong Med J. 1997 Dec;3(4):355-61.
https://www.hkmj.org/system/files/hkm9712p355.pdf
http://www.ncbi.nlm.nih.gov/pubmed/11847385?tool=bestpractice.com
The presenting symptoms are common but are not specific to NPC. Headaches, facial numbness, or diplopia may suggest cranial nerve involvement. Fever, night sweats, and unintentional weight loss should raise suspicion of malignancy in general.
Ask about risk factors for NPC, such as a diet rich in preserved foods (salted fish in particular), smoking or other tobacco use, or a family history of NPC in a first-degree relative. In patients who smoke, document the pack years smoked.[19]National Comprehensive Cancer Network. NCCN clinical practice guidelines in oncology: head and neck cancers [internet publication].
https://www.nccn.org/guidelines/category_1
Physical exam
Perform a comprehensive head and neck exam and, in particular, palpate the neck for masses that may indicate lymphadenopathy.[19]National Comprehensive Cancer Network. NCCN clinical practice guidelines in oncology: head and neck cancers [internet publication].
https://www.nccn.org/guidelines/category_1
Perform a targeted physical exam, including visualizing the mucosa of the larynx, base of tongue, and pharynx.[20]Pynnonen MA, Gillespie MB, Roman B, et al. Clinical practice guideline: evaluation of the neck mass in adults. Otolaryngol Head Neck Surg. 2017 Sep;157(2 suppl):S1-30.
https://aao-hnsfjournals.onlinelibrary.wiley.com/doi/10.1177/0194599817722550
http://www.ncbi.nlm.nih.gov/pubmed/28891406?tool=bestpractice.com
A neck mass in patients >40 years should increase suspicion of malignancy and is the most common presenting symptom for NPC.[4]Lee AW, Foo W, Law SC, et al. Nasopharyngeal carcinoma: presenting symptoms and duration before diagnosis. Hong Kong Med J. 1997 Dec;3(4):355-61.
https://www.hkmj.org/system/files/hkm9712p355.pdf
http://www.ncbi.nlm.nih.gov/pubmed/11847385?tool=bestpractice.com
[21]Expert Panel on Neurologic Imaging; Aulino JM, Kirsch CFE, et al. ACR appropriateness criteria(®) neck mass-adenopathy. J Am Coll Radiol. 2019 May;16(5s):S150-60.
https://www.jacr.org/article/S1546-1440(19)30167-X/fulltext
http://www.ncbi.nlm.nih.gov/pubmed/31054741?tool=bestpractice.com
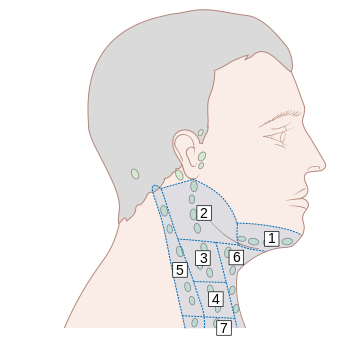
Nodal metastases are usually present at diagnosis. Among people with NPC who present with neck masses, lymphadenopathy in level II is the most common location, which is similar to other head and neck mucosal squamous cell carcinomas.[5]Ho FC, Tham IW, Earnest A, et al. Patterns of regional lymph node metastasis of nasopharyngeal carcinoma: a meta-analysis of clinical evidence. BMC Cancer. 2012 Mar 21;12:98.
https://jamanetwork.com/journals/jamaotolaryngology/fullarticle/484065
http://www.ncbi.nlm.nih.gov/pubmed/22433671?tool=bestpractice.com
[6]Ludwig R, Hoffmann JM, Pouymayou B, et al. Detailed patient-individual reporting of lymph node involvement in oropharyngeal squamous cell carcinoma with an online interface. Radiother Oncol. 2022 Apr;169:1-7.
https://www.thegreenjournal.com/article/S0167-8140(22)00061-5/fulltext
http://www.ncbi.nlm.nih.gov/pubmed/35121032?tool=bestpractice.com
However, level V lymphadenopathy in the posterior cervical triangle is relatively common in NPC and this pattern of lymph node spread distinguishes NPC from many other head and neck cancers.
[Figure caption and citation for the preceding image starts]: Lymph node groups in the head and neck; the numbers refer to the anatomic levels of the lymph nodesCancer Research UK [Citation ends].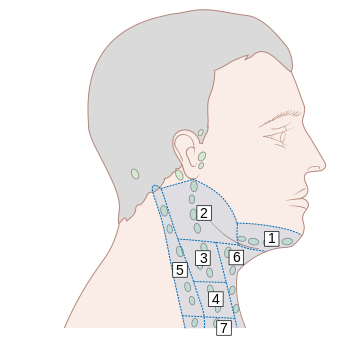
Examine the cranial nerves. Cranial nerves III, IV, V, and VI are most commonly affected due to disease invading the skull base/cavernous sinus.
Initial investigations
Perform nasopharyngoscopy.[19]National Comprehensive Cancer Network. NCCN clinical practice guidelines in oncology: head and neck cancers [internet publication].
https://www.nccn.org/guidelines/category_1
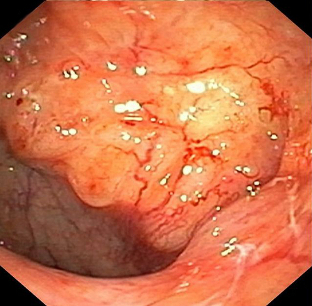
Most NPC arises from the lateral pharyngeal recess (fossa of Rosenmüller).[2]Bossi P, Chan AT, Licitra L, et al. Nasopharyngeal carcinoma: ESMO-EURACAN clinical practice guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2021 Apr;32(4):452-65.
https://www.annalsofoncology.org/article/S0923-7534(20)43210-7/fulltext
http://www.ncbi.nlm.nih.gov/pubmed/33358989?tool=bestpractice.com
[22]Maghami E, Ismaila N, Alvarez A, et al. Diagnosis and management of squamous cell carcinoma of unknown primary in the head and neck: ASCO guideline. J Clin Oncol. 2020 Aug 1;38(22):2570-96.
https://ascopubs.org/doi/10.1200/JCO.20.00275?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub%20%200pubmed
http://www.ncbi.nlm.nih.gov/pubmed/32324430?tool=bestpractice.com
Establish the diagnosis with an endoscopic biopsy of the primary tumor and/or fine-needle aspiration/core biopsy of neck nodal metastasis.[2]Bossi P, Chan AT, Licitra L, et al. Nasopharyngeal carcinoma: ESMO-EURACAN clinical practice guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2021 Apr;32(4):452-65.
https://www.annalsofoncology.org/article/S0923-7534(20)43210-7/fulltext
http://www.ncbi.nlm.nih.gov/pubmed/33358989?tool=bestpractice.com
[19]National Comprehensive Cancer Network. NCCN clinical practice guidelines in oncology: head and neck cancers [internet publication].
https://www.nccn.org/guidelines/category_1
[22]Maghami E, Ismaila N, Alvarez A, et al. Diagnosis and management of squamous cell carcinoma of unknown primary in the head and neck: ASCO guideline. J Clin Oncol. 2020 Aug 1;38(22):2570-96.
https://ascopubs.org/doi/10.1200/JCO.20.00275?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub%20%200pubmed
http://www.ncbi.nlm.nih.gov/pubmed/32324430?tool=bestpractice.com
[Figure caption and citation for the preceding image starts]: Endoscopic image of left-sided nasopharyngeal tumourSakthivel P et al. BMJ Case Reports CP 2020;13:e237392; used with permission [Citation ends].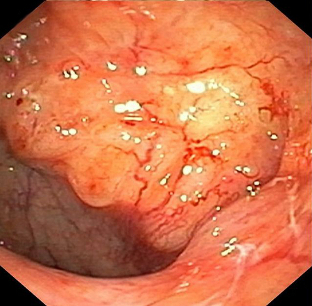
Use magnetic resonance imaging (MRI) with or without contrast (preferred) or computed tomography (CT) with contrast for T and N staging.[2]Bossi P, Chan AT, Licitra L, et al. Nasopharyngeal carcinoma: ESMO-EURACAN clinical practice guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2021 Apr;32(4):452-65.
https://www.annalsofoncology.org/article/S0923-7534(20)43210-7/fulltext
http://www.ncbi.nlm.nih.gov/pubmed/33358989?tool=bestpractice.com
[19]National Comprehensive Cancer Network. NCCN clinical practice guidelines in oncology: head and neck cancers [internet publication].
https://www.nccn.org/guidelines/category_1
MRI is superior to CT to evaluate skull base and cranial nerve involvement.[2]Bossi P, Chan AT, Licitra L, et al. Nasopharyngeal carcinoma: ESMO-EURACAN clinical practice guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2021 Apr;32(4):452-65.
https://www.annalsofoncology.org/article/S0923-7534(20)43210-7/fulltext
http://www.ncbi.nlm.nih.gov/pubmed/33358989?tool=bestpractice.com
Use 18F-fluorodeoxyglucose positron emission tomography and/or chest CT with contrast for M staging.[2]Bossi P, Chan AT, Licitra L, et al. Nasopharyngeal carcinoma: ESMO-EURACAN clinical practice guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2021 Apr;32(4):452-65.
https://www.annalsofoncology.org/article/S0923-7534(20)43210-7/fulltext
http://www.ncbi.nlm.nih.gov/pubmed/33358989?tool=bestpractice.com
[19]National Comprehensive Cancer Network. NCCN clinical practice guidelines in oncology: head and neck cancers [internet publication].
https://www.nccn.org/guidelines/category_1
Bone is the most common site for metastasis, followed by lung and liver.
Other investigations
Consider the following pretreatment laboratory studies:
Plasma EBV DNA level is prognostic.[2]Bossi P, Chan AT, Licitra L, et al. Nasopharyngeal carcinoma: ESMO-EURACAN clinical practice guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2021 Apr;32(4):452-65.
https://www.annalsofoncology.org/article/S0923-7534(20)43210-7/fulltext
http://www.ncbi.nlm.nih.gov/pubmed/33358989?tool=bestpractice.com
[19]National Comprehensive Cancer Network. NCCN clinical practice guidelines in oncology: head and neck cancers [internet publication].
https://www.nccn.org/guidelines/category_1
[23]Lee AWM, Lee VHF, Ng WT, et al. A systematic review and recommendations on the use of plasma EBV DNA for nasopharyngeal carcinoma. Eur J Cancer. 2021 Aug;153:109-22.
http://www.ncbi.nlm.nih.gov/pubmed/34153713?tool=bestpractice.com
High plasma EBV (>4000 copies/mL) is associated with a higher chance of distant metastasis.
EBV-encoded RNA in situ hybridization (EBER ISH) is not routinely performed on tumor tissues in endemic countries, but it is useful in establishing a diagnosis in cases of occult primary tumors, particularly in nonendemic countries.[2]Bossi P, Chan AT, Licitra L, et al. Nasopharyngeal carcinoma: ESMO-EURACAN clinical practice guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2021 Apr;32(4):452-65.
https://www.annalsofoncology.org/article/S0923-7534(20)43210-7/fulltext
http://www.ncbi.nlm.nih.gov/pubmed/33358989?tool=bestpractice.com
Complete blood counts, serum biochemistry, and liver and thyroid function tests.
Hepatitis B (HBsAg, anti-HBc, and anti-HBs) and HCV (anti-HCV) screening.
Serum or urine pregnancy test and contraceptive counseling.[19]National Comprehensive Cancer Network. NCCN clinical practice guidelines in oncology: head and neck cancers [internet publication].
https://www.nccn.org/guidelines/category_1
Other investigations/assessments that are useful to perform as baseline evaluations prior to starting treatment include:[2]Bossi P, Chan AT, Licitra L, et al. Nasopharyngeal carcinoma: ESMO-EURACAN clinical practice guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2021 Apr;32(4):452-65.
https://www.annalsofoncology.org/article/S0923-7534(20)43210-7/fulltext
http://www.ncbi.nlm.nih.gov/pubmed/33358989?tool=bestpractice.com
[19]National Comprehensive Cancer Network. NCCN clinical practice guidelines in oncology: head and neck cancers [internet publication].
https://www.nccn.org/guidelines/category_1
Audiogram (not required, but highly recommended prior to platinum chemotherapy)
Speech and swallowing consultation and formal assessment by modified barium swallow/videofluoroscopy
Dental evaluation and counseling in preparation for radiation therapy
Nutrition evaluation
Screening for hepatitis B
Smoking cessation advice, where necessary
Consider ophthalmologic and endocrine evaluation, especially baseline pituitary function tests.