History and exam
Key diagnostic factors
common
increased risk of exposure to HPV
immunocompromise
sessile exophytic papillomas
Lesions are usually 1 to 3 mm, discrete, sessile, smooth-surfaced exophytic papillomas or they may coalesce into larger plaques.[Figure caption and citation for the preceding image starts]: Wart on shaft of penisFrom Dr Tyring's personal collection; used with permission [Citation ends]. [Figure caption and citation for the preceding image starts]: Close-up of penile wartFrom Dr Tyring's personal collection; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Close-up of penile wartFrom Dr Tyring's personal collection; used with permission [Citation ends].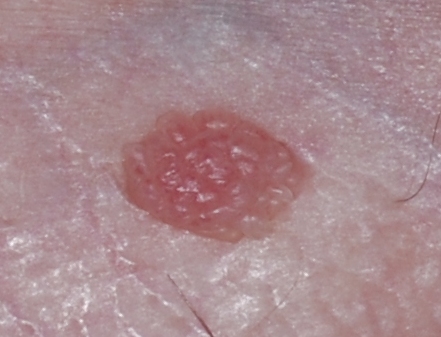
Colour varies from flesh-coloured to whitish to hyperpigmented.
Maceration may be present, particularly in moist areas.[Figure caption and citation for the preceding image starts]: Venereal warts in the anal region of the perineumCDC/Dr Wiesner [Citation ends].
Other diagnostic factors
common
asymptomatic
Lesions are generally asymptomatic, and can be in an area that the patient has difficulty viewing.
uncommon
pruritus
Lesions are usually asymptomatic, but patient may present with itch.
bleeding
Usually due to local trauma or maceration of the area, depending on where the warts are located (e.g., if the warts are in the inguinal area, they can be rubbed by underwear or with walking).
pain
Occurs when the lesions become friable or become irritated from local trauma/maceration.
urinary symptoms
Symptoms such as terminal haematuria or abnormal stream of urine can indicate lesions in the distal urethra and meatus.
Risk factors
strong
intercourse at an early age
increasing number of lifetime sexual partners
young sexually active adults
Females aged 19 to 22 years and males 22 to 26 years are susceptible to get infected with human papillomavirus.[7]
increasing number of partner's lifetime sexual partners
Use of this content is subject to our disclaimer