Recommendations
Key Recommendations
During periods of high COVID-19 prevalence, for patients with suspected or confirmed COVID-19 pneumonia with symptoms and signs that start at any point after hospital admission, see Coronavirus disease 2019 (COVID-19).
Consider all patients with cough, fever, or other suggestive symptoms to have COVID-19 until proven otherwise. Pneumonia due to COVID-19 is not covered in this topic.
For patients with symptoms and signs consistent with bacterial pneumonia (not secondary to COVID-19), that start on days 1 or 2 after hospital admission, see Community-acquired pneumonia in adults (non-Covid-19).
Clinical history is especially important because witnessed aspiration is not seen in the majority of patients. Risk factors for aspiration pneumonia include poor dentition, advanced age, swallowing dysfunction, altered mental status, intubation or tracheostomy tube, gastrointestinal disease, recumbent position, and presence of a feeding tube. Symptoms include cough, dyspnea, and pleuritic chest pain, but may be nonspecific and be present for a week or more after the event. Rigors or a more acute presentation is uncommon. Signs such as fever, crepitations, tachypnea, and frothy or purulent sputum should raise the suspicion for aspiration pneumonia. Sputum is foul smelling if there is infection by anaerobes, although anaerobic infection is less commonly observed than in prior decades.
Diagnostic tests
The initial tests for aspiration pneumonia are essentially the same as those for typical pneumonia. Chest x-ray (CXR) and complete blood count are recommended as first-line tests. CXR should be obtained even in the absence of significant pulmonary symptoms in order to look for a new infiltrate in dependent regions of the lungs. [Figure caption and citation for the preceding image starts]: Early ill-defined opacities of the right upper lobe above the minor fissure consistent with early changes of aspiration pneumoniaUsed with kind permission from Roy Hammond, MD [Citation ends].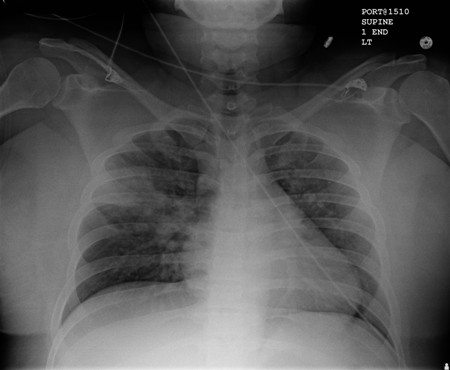 [Figure caption and citation for the preceding image starts]: Increased opacification of the right perihilar region and superior segment of the right lower and upper lobes consistent with worsening aspiration pneumoniaUsed with kind permission from Roy Hammond, MD [Citation ends].
[Figure caption and citation for the preceding image starts]: Increased opacification of the right perihilar region and superior segment of the right lower and upper lobes consistent with worsening aspiration pneumoniaUsed with kind permission from Roy Hammond, MD [Citation ends].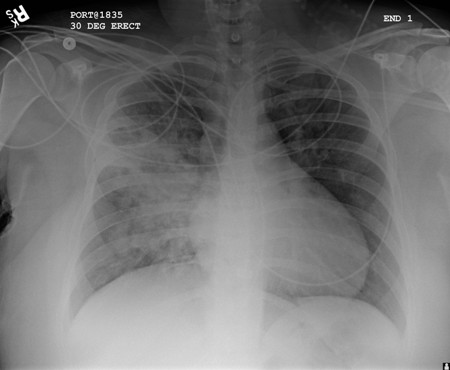 A lung ultrasound should be considered if the CXR is negative and the patient is elderly and frail or the clinical suspicion is uncertain.[40] The American College of Physicians recommends point-of-care ultrasound if there is diagnostic uncertainty in patients with acute dyspnea.[41]
A lung ultrasound should be considered if the CXR is negative and the patient is elderly and frail or the clinical suspicion is uncertain.[40] The American College of Physicians recommends point-of-care ultrasound if there is diagnostic uncertainty in patients with acute dyspnea.[41]
Leukocytosis is often present. O2 saturations should be done, and an arterial blood gas test is recommended based on the clinical scenario of a patient (e.g., worsening oxygenation, increased work of breathing, and other systemic signs of organ dysfunction).
Sputum Gram stain is recommended because of low cost and ease of obtaining the sample. Gram stain may reveal white blood cells and mixed bacterial flora. Gram stain result is often inconclusive, although occasionally it may verify the infecting organism.
When available, culture of expectorated sputum should be obtained. Although sputum cultures are not specifically indicated and their results are not very informative, they are routinely performed owing to the lack of other available diagnostic tests. They are inexpensive and a noninvasive way to obtain a bacterial specimen. Most culture results are inconclusive. Culture results usually fail to grow common pulmonary pathogens. Results may guide therapy if organism identification and sensitivities are available.
Evidence is lacking for blood cultures as a diagnostic test because aspiration is an acute event. Blood cultures are usually not necessary because the aspiration pneumonia is usually diagnosed and treated prior to the development of bacteremia.
Bronchoscopy may be used in large-volume particulate aspirates, but there are no studies showing benefits of such an intervention. Protected brush specimens have been used only in research studies trying to identify an etiology for aspiration pneumonia; the impact of such an intervention in managing aspiration pneumonia has not been determined. For aspiration pneumonia, particularly in a nursing-home or a hospital setting, obtaining a good sputum or lower respiratory tract sample is recommended as per the guidelines for hospital-acquired and community-acquired pneumonia.[7][20]
Use of this content is subject to our disclaimer