History
Clinicians should suspect PCP when caring for adult or adolescent patients who are HIV-positive, especially if they are nonadherent with combination antiretroviral therapy (ART) or PCP prophylaxis, have had a previous episode of PCP, and/or have a CD4 cell count <200 cells/microliter.[60]Katz MH, Baron RB, Grady D. Risk stratification of ambulatory patients suspected of Pneumocystis pneumonia. Arch Intern Med. 1991 Jan;151(1):105-10.
http://www.ncbi.nlm.nih.gov/pubmed/1985585?tool=bestpractice.com
HIV-positive children and HIV-indeterminate infants of HIV-infected mothers who present with respiratory symptoms should also be evaluated for PCP.
Other groups of patients in whom to suspect PCP are those who are immunocompromised with a history of:[31]Stern A, Green H, Paul M, et al. Prophylaxis for Pneumocystis pneumonia (PCP) in non-HIV immunocompromised patients. Cochrane Database Syst Rev. 2014 Oct 1;(10):CD005590.
http://onlinelibrary.wiley.com/doi/10.1002/14651858.CD005590.pub3/full
http://www.ncbi.nlm.nih.gov/pubmed/25269391?tool=bestpractice.com
[47]Taplitz RA, Kennedy EB, Bow EJ, et al. Antimicrobial prophylaxis for adult patients with cancer-related immunosuppression: ASCO and IDSA clinical practice guideline update. J Clin Oncol. 2018 Oct 20;36(30):3043-54.
https://ascopubs.org/doi/10.1200/JCO.18.00374?url_ver=Z39.88-2003&rfr_id=ori%3Arid%3Acrossref.org&rfr_dat=cr_pub++0pubmed
http://www.ncbi.nlm.nih.gov/pubmed/30179565?tool=bestpractice.com
[48]Tomblyn M, Chiller T, Einsele H, et al. Guidelines for preventing infectious complications among hematopoietic cell transplantation recipients: a global perspective. Biol Blood Marrow Transplant. 2009 Oct;15(10):1143-238.
https://www.bbmt.org/article/S1083-8791(09)00300-0/fulltext
http://www.ncbi.nlm.nih.gov/pubmed/19747629?tool=bestpractice.com
[49]Fishman JA, Gans H, AST Infectious Diseases Community of Practice. Pneumocystis jiroveci in solid organ transplantation: guidelines from the American Society of Transplantation Infectious Diseases Community of Practice. Clin Transplant. 2019 Sep;33(9):e13587.
http://www.ncbi.nlm.nih.gov/pubmed/31077616?tool=bestpractice.com
Hematologic malignancy
Hematopoietic cell transplantation
Other malignancies where chemotherapy regimen is associated with >3.5% risk of PCP
Solid-organ transplantation
Chronic use of corticosteroids with or without other immunosuppressive drugs
Certain primary immunodeficiencies (e.g., severe combined immunodeficiency)
In patients with atypical presentations of pneumonia, assessing for HIV risk factors and performing HIV testing can also help identify patients at risk of PCP.
In HIV-positive PCP, presentation is often an insidious progression of fatigue, fevers, chills, sweats, nonproductive cough, and dyspnea over several weeks. Other findings associated with PCP are a history of recurrent bacterial pneumonias, weight loss, and oral candidiaisis.[43]Salzer HJF, Schäfer G, Hoenigl M, et al. Clinical, diagnostic, and treatment disparities between HIV-infected and non-HIV-infected immunocompromised patients with Pneumocystis jirovecii pneumonia. Respiration. 2018;96(1):52-65.
https://www.doi.org/10.1159/000487713
http://www.ncbi.nlm.nih.gov/pubmed/29635251?tool=bestpractice.com
In HIV-negative patients, the presentation is typically more rapid and more severe.[43]Salzer HJF, Schäfer G, Hoenigl M, et al. Clinical, diagnostic, and treatment disparities between HIV-infected and non-HIV-infected immunocompromised patients with Pneumocystis jirovecii pneumonia. Respiration. 2018;96(1):52-65.
https://www.doi.org/10.1159/000487713
http://www.ncbi.nlm.nih.gov/pubmed/29635251?tool=bestpractice.com
The onset of symptoms may occur while the usual dose of immunosuppressive agents is being decreased or discontinued.[61]Pareja JGR, Garland R, Koziel H. Use of adjunctive corticosteroids in severe adult non-HIV Pneumocystis carinii pneumonia. Chest. 1998 May;113(5):1215-24.
http://www.ncbi.nlm.nih.gov/pubmed/9596297?tool=bestpractice.com
Rarely, infection causes extrapulmonary manifestations in those with advanced HIV; however, in patients with advanced AIDS or in HIV-positive patients who are not taking their prophylaxis, there may be systemic infection with visual symptoms, cognitive impairment owing to central nervous system involvement, and gastrointestinal symptoms, such as diarrhea.
Investigations
If PCP is suspected based on clinical presentation, and the chest x-ray is compatible with PCP, the first step in diagnosis should be an induced sputum for visualization of Pneumocystis jirovecii.[62]Singh N, Shafer RW, Swindells S (eds). HIV clinical manual. Pittsburgh, PA: ESun Technologies; 2003. Sputum that is spontaneously expectorated has low sensitivity for the diagnosis of PCP and should not be used. Sensitivity of induced sputum testing is 50% to 90% depending on the quality of the sample, the pathogen load, the staining method used, and the experience of the institution.[32]National Institutes of Health, Centers for Disease Control and Prevention, HIV Medicine Association, and Infectious Diseases Society of America. Panel on Guidelines for the Prevention and Treatment of Opportunistic Infections in Adults and Adolescents with HIV. Guidelines for the prevention and treatment of opportunistic infections in adults and adolescents with HIV. Pneumocystis pneumonia. Sep 2024 [internet publication].
https://clinicalinfo.hiv.gov/en/guidelines/adult-and-adolescent-opportunistic-infection/pneumocystis-pneumonia
[63]Fortun J, Navas E, Marti-Belda P, et al. Pneumocystis carinii pneumonia in HIV-infected patients: diagnostic yield of induced sputum and immunofluorescent stain with monoclonal antibodies. Eur Respir J. 1992 Jun;5(6):665-9.
http://www.ncbi.nlm.nih.gov/pubmed/1628723?tool=bestpractice.com
[64]Kovacs JA, Ng VL, Masur H, et al. Diagnosis of Pneumocystis carinii pneumonia: improved detection in sputum with use of monoclonal antibodies. N Engl J Med. 1988 Mar 10;318(10):589-93.
http://www.ncbi.nlm.nih.gov/pubmed/2449613?tool=bestpractice.com
[65]Midgley J, Parsons P, Leigh TR, et al. Increased sensitivity of immunofluorescence for detection of Pneumocystis carinii. Lancet. 1989 Dec 23-30;2(8678-8679):1523.
http://www.ncbi.nlm.nih.gov/pubmed/2574793?tool=bestpractice.com
[66]Ng VL, Virani NA, Chaisson RE, et al. Rapid detection of Pneumocystis carinii using a direct fluorescent monoclonal antibody stain. J Clin Microbiol. 1990 Oct;28(10):2228-33.
http://www.ncbi.nlm.nih.gov/pubmed/1699968?tool=bestpractice.com
If sputum induction is negative, bronchoscopic examination with BAL should be performed. The sensitivity for BAL is 90% to 99% in HIV-positive patients, so it is usually performed without transbronchial biopsy.[32]National Institutes of Health, Centers for Disease Control and Prevention, HIV Medicine Association, and Infectious Diseases Society of America. Panel on Guidelines for the Prevention and Treatment of Opportunistic Infections in Adults and Adolescents with HIV. Guidelines for the prevention and treatment of opportunistic infections in adults and adolescents with HIV. Pneumocystis pneumonia. Sep 2024 [internet publication].
https://clinicalinfo.hiv.gov/en/guidelines/adult-and-adolescent-opportunistic-infection/pneumocystis-pneumonia
In general, if BAL is negative in an HIV-positive patient, then another etiology should be considered and treatment can be discontinued.
Transbronchial biopsies can be performed if initial BAL is negative but clinical suspicion of PCP is high or other diagnoses are considered likely. Sensitivity of transbronchial biopsies is 95% to 100%.[32]National Institutes of Health, Centers for Disease Control and Prevention, HIV Medicine Association, and Infectious Diseases Society of America. Panel on Guidelines for the Prevention and Treatment of Opportunistic Infections in Adults and Adolescents with HIV. Guidelines for the prevention and treatment of opportunistic infections in adults and adolescents with HIV. Pneumocystis pneumonia. Sep 2024 [internet publication].
https://clinicalinfo.hiv.gov/en/guidelines/adult-and-adolescent-opportunistic-infection/pneumocystis-pneumonia
In HIV-negative patients, transbronchial biopsy is more often necessary to confirm a diagnosis because BAL is less sensitive. Transbronchial biopsy does have a higher risk of complications, such as bleeding and pneumothorax. Pneumothorax occurred in 9% of HIV-positive patients who had transbronchial biopsies in one series with 5% requiring insertion of a chest tube.[67]Harcup C, Baier HJ, Pitchenik AE. Evaluation of patients with the acquired immunodeficiency syndrome (AIDS) by fiberoptic bronchoscopy. Endoscopy. 1985 Nov;17(6):217-20.
http://www.ncbi.nlm.nih.gov/pubmed/3877629?tool=bestpractice.com
If clinical suspicion for PCP remains high or prior testing does not reveal the etiology for the patient's illness, an open lung biopsy can be considered to confirm or rule out PCP as well as to determine if another pathology is present. The sensitivity of open lung biopsies is 95% to 100%.[32]National Institutes of Health, Centers for Disease Control and Prevention, HIV Medicine Association, and Infectious Diseases Society of America. Panel on Guidelines for the Prevention and Treatment of Opportunistic Infections in Adults and Adolescents with HIV. Guidelines for the prevention and treatment of opportunistic infections in adults and adolescents with HIV. Pneumocystis pneumonia. Sep 2024 [internet publication].
https://clinicalinfo.hiv.gov/en/guidelines/adult-and-adolescent-opportunistic-infection/pneumocystis-pneumonia
Elevated serum LDH (>220 international units/L) has both diagnostic and prognostic significance with a higher LDH level being associated with increased mortality.[68]Zaman MK, White DA. Serum lactate dehydrogenase levels and Pneumocystis carinii pneumonia. Diagnostic and prognostic significance. Am Rev Respir Dis. 1988 Apr;137(4):796-800.
http://www.ncbi.nlm.nih.gov/pubmed/3258483?tool=bestpractice.com
Arterial blood gas is used to determine severity:[32]National Institutes of Health, Centers for Disease Control and Prevention, HIV Medicine Association, and Infectious Diseases Society of America. Panel on Guidelines for the Prevention and Treatment of Opportunistic Infections in Adults and Adolescents with HIV. Guidelines for the prevention and treatment of opportunistic infections in adults and adolescents with HIV. Pneumocystis pneumonia. Sep 2024 [internet publication].
https://clinicalinfo.hiv.gov/en/guidelines/adult-and-adolescent-opportunistic-infection/pneumocystis-pneumonia
Patients with a clinical presentation suggestive of PCP, but a normal or unchanged chest x-ray, should undergo either a high-resolution computed tomography (HRCT) scan of the chest or pulmonary function tests with measurement of diffusing capacity for carbon monoxide (DLCO). If the HRCT scan shows ground glass opacities or the DLCO is decreased, then the patient should undergo sputum induction followed by BAL (if sputum induction is negative), as the presence of ground glass opacities or decreased DLCO are sensitive, but not specific, tests for PCP.[69]Gruden JF, Huang L, Turner J, et al. High-resolution CT in the evaluation of clinically suspected Pneumocystis carinii pneumonia in AIDS patients with normal, equivocal, or nonspecific radiographic findings. AJR Am J Roentgenol. 1997 Oct;169(4):967-75.
http://www.ajronline.org/doi/pdf/10.2214/ajr.169.4.9308446
http://www.ncbi.nlm.nih.gov/pubmed/9308446?tool=bestpractice.com
[70]Huang L, Stansell J, Osmond D, et al. Performance of an algorithm to detect Pneumocystis carinii pneumonia in symptomatic HIV-infected persons. Chest. 1999 Apr;115(4):1025-32.
http://www.ncbi.nlm.nih.gov/pubmed/10208204?tool=bestpractice.com
[71]Sankary RM, Turner J, Lipavsky A, et al. Alveolar-capillary block in patients with AIDS and Pneumocystis carinii pneumonia. Am Rev Respir Dis. 1988 Feb;137(2):443-9.
http://www.ncbi.nlm.nih.gov/pubmed/3257662?tool=bestpractice.com
If both tests are negative, then another etiology should be considered and appropriate diagnostic workup performed. If all diagnostic samples for Pneumocystis jirovecii are negative, then the patient is very unlikely to have PCP and the patient should be observed and other etiologies considered. Further testing may be necessary depending on the clinical situation.
A diagnosis of PCP does not rule out the possibility of a second, concurrent process. Although it is preferable to confirm the diagnosis of PCP microscopically because many conditions can have similar presentations, empiric treatment of patients with a clinical presentation suggestive of PCP may be undertaken, particularly in places where there are limited resources for performing induced sputum or BAL.
The identification of Pneumocystis jirovecii in sputum or BAL fluid has typically been performed with stains, such as toluidine blue, Geimsa, Diff-Quik, and methenamine silver. Immunofluorescent assays (direct fluorescent-antigen testing) may also be used, which have a higher sensitivity.[72]Shelhamer JH, Gill VJ, Quinn TC, et al. The laboratory evaluation of opportunistic pulmonary infections. Ann Intern Med. 1996 Mar 15;124(6):585-99.
http://www.ncbi.nlm.nih.gov/pubmed/8597323?tool=bestpractice.com
Transbronchial biopsies along with BAL can increase the diagnostic yield.[73]Broaddus C, Dake MD, Stulbarg MS, et al. Bronchoalveolar lavage and transbronchial biopsy for the diagnosis of pulmonary infections in the acquired immunodeficiency syndrome. Ann Intern Med. 1985 Jun;102(6):747-52.
http://www.ncbi.nlm.nih.gov/pubmed/2986505?tool=bestpractice.com
Other assays, such as polymerase chain reaction (PCR), real-time PCR, and reverse transcriptase PCR, can detect low levels of Pneumocystis jirovecii DNA. These assays, along with plasma levels of S-adenosylmethionine, may increase sensitivity of diagnosing PCP but are often not clinically available. PCR techniques have a higher false-positive rate than histochemical staining.[74]Fillaux J, Malvy S, Alvarez M, et al. Accuracy of a routine real-time PCR assay for the diagnosis of Pneumocystis jiroveci pneumonia. J Microbiol Methods. 2008 Oct;75(2):258-61.
http://www.ncbi.nlm.nih.gov/pubmed/18606198?tool=bestpractice.com
[75]Tuncer S, Erguven S, Kocagoz S, et al. Comparison of cytochemical staining, immunofluorescence and PCR for diagnosis of Pneumocystis carinii on sputum samples. Scand J Infect Dis. 1998;30(2):125-8.
http://www.ncbi.nlm.nih.gov/pubmed/9730296?tool=bestpractice.com
[76]Larsen HH, Masur H, Kovacs JA, et al. Development and evaluation of a quantitative, touch-down, real-time PCR assay for diagnosing Pneumocystis carinii pneumonia. J Clin Microbiol. 2002 Feb;40(2):490-4.
http://www.ncbi.nlm.nih.gov/pubmed/11825961?tool=bestpractice.com
[77]Helweg-Larsen J, Jensen JS, Lundgren B. Diagnostic use of PCR for detection of Pneumocystis carinii in oral wash samples. J Clin Microbiol. 1998 Jul;36(7):2068-72.
http://www.ncbi.nlm.nih.gov/pubmed/9650964?tool=bestpractice.com
[78]Larsen HH, Huang L, Kovacs JA, et al. A prospective, blinded study of quantitative touch-down polymerase chain reaction using oral-wash samples for diagnosis of Pneumocystis pneumonia in HIV-infected patients. J Infect Dis. 2004 May 1;189(9):1679-83.
http://www.ncbi.nlm.nih.gov/pubmed/15116305?tool=bestpractice.com
[79]Skelly MJ, Holzman RS, Merali S. S-adenosylmethionine levels in the diagnosis of Pneumocystis carinii pneumonia in patients with HIV infection. Clin Infect Dis. 2008 Feb 1;46(3):467-71.
http://cid.oxfordjournals.org/content/46/3/467.long
http://www.ncbi.nlm.nih.gov/pubmed/18177224?tool=bestpractice.com
[80]Summah H, Zhu YG, Falagas ME, et al. Use of real-time polymerase chain reaction for the diagnosis of Pneumocystis pneumonia in immunocompromised patients: a meta-analysis. Chin Med J (Engl). 2013;126(10):1965-73.
http://www.ncbi.nlm.nih.gov/pubmed/23673119?tool=bestpractice.com
There has also been interest in measuring serum (1,3)-beta-D-glucan, an element of the fungal wall, for the diagnosis of PCP.[81]Watanabe T, Yasuoka A, Tanuma J, et al. Serum (1-->3) beta-D-glucan as a noninvasive adjunct marker for the diagnosis of Pneumocystis pneumonia in patients with AIDS. Clin Infect Dis. 2009 Oct 1;49(7):1128-31.
http://cid.oxfordjournals.org/content/49/7/1128.long
http://www.ncbi.nlm.nih.gov/pubmed/19725788?tool=bestpractice.com
[82]Shimizu Y, Sunaga N, Dobashi K, et al. Serum markers in interstitial pneumonia with and without Pneumocystis jirovecii colonization: a prospective study. BMC Infect Dis. 2009 Apr 22;9:47.
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2676289/?tool=pubmed
http://www.ncbi.nlm.nih.gov/pubmed/19383170?tool=bestpractice.com
[83]Desmet S, Van Wijngaerden E, Maertens J, et al. Serum (1-3)-beta-D-glucan as a tool for diagnosis of Pneumocystis jirovecii pneumonia in patients with human immunodeficiency virus infection or hematological malignancy. J Clin Microbiol. 2009 Dec;47(12):3871-4.
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2786638/?tool=pubmed
http://www.ncbi.nlm.nih.gov/pubmed/19846641?tool=bestpractice.com
[84]Del Bono V, Mularoni A, Furfaro E, et al. Clinical evaluation of a (1,3)-beta-D-glucan assay for presumptive diagnosis of Pneumocystis jiroveci pneumonia in immunocompromised patients. Clin Vaccine Immunol. 2009 Oct;16(10):1524-6.
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2756857/?tool=pubmed
http://www.ncbi.nlm.nih.gov/pubmed/19692624?tool=bestpractice.com
[85]Nakamura H, Tateyama M, Tasato D, et al. Clinical utility of serum beta-D-glucan and KL-6 levels in Pneumocystis jirovecii pneumonia. Intern Med. 2009;48(4):195-202.
https://www.jstage.jst.go.jp/article/internalmedicine/48/4/48_4_195/_article
http://www.ncbi.nlm.nih.gov/pubmed/19218768?tool=bestpractice.com
These studies show (1,3)-beta-D-glucan to be significantly elevated in patients with PCP, although less so in HIV-negative patients with PCP, and the levels did not correlate with severity or response to therapy.[86]Huang L. Clinical and translational research in pneumocystis and pneumocystis pneumonia. Parasite. 2011 Feb;18(1):3-11.
http://www.ncbi.nlm.nih.gov/pubmed/21395200?tool=bestpractice.com
One 2012 meta-analysis of studies on (1,3)-beta-D-glucan in the diagnosis of PCP in various populations (HIV-infected and HIV-uninfected) showed that the pooled sensitivity and specificity were 96% and 84%, respectively.[87]Onishi A, Sugiyama D, Kogata Y, et al. Diagnostic accuracy of serum 1,3-β-D-glucan for pneumocystis jiroveci pneumonia, invasive candidiasis, and invasive aspergillosis: systematic review and meta-analysis. J Clin Microbiol. 2012 Jan;50(1):7-15.
http://jcm.asm.org/content/50/1/7.long
http://www.ncbi.nlm.nih.gov/pubmed/22075593?tool=bestpractice.com
One more recent 2015 meta-analysis demonstrated similar sensitivity (92%) and specificity (78%) for HIV-infected patients; however, in HIV-uninfected patients, sensitivity and specificity were lower, at 85% and 73%, respectively.[88]Li WJ, Guo YL, Liu TJ, et al. Diagnosis of pneumocystis pneumonia using serum (1-3)-β-D-Glucan: a bivariate meta-analysis and systematic review. J Thorac Dis. 2015 Dec;7(12):2214-25.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4703639
http://www.ncbi.nlm.nih.gov/pubmed/26793343?tool=bestpractice.com
In one of the largest studies of HIV-infected participants (n=282) with 69% having PCP, the sensitivity and specificity were 92% and 65%, respectively.[89]Sax PE, Komarow L, Finkelman MA, et al. Blood (1->3)-beta-D-glucan as a diagnostic test for HIV-related Pneumocystis jirovecii pneumonia. Clin Infect Dis. 2011 Jul 15;53(2):197-202.
http://cid.oxfordjournals.org/content/53/2/197.long
http://www.ncbi.nlm.nih.gov/pubmed/21690628?tool=bestpractice.com
In a study of 159 AIDS patients with at least one respiratory symptom, 139 of whom had PCP, the sensitivity and specificity of (1,3)-beta-D-glucan were 92.8% and 75.0%, respectively.[90]Wood BR, Komarow L, Zolopa AR, et al. Test performance of blood beta-glucan for Pneumocystis jirovecii pneumonia in patients with AIDS and respiratory symptoms. AIDS. 2013 Mar 27;27(6):967-72.
http://www.ncbi.nlm.nih.gov/pubmed/23698062?tool=bestpractice.com
While the sensitivity may be helpful in ruling out PCP in settings where more sensitive tests are not available, the decreased specificity is due to detection of (1,3)-beta-D-glucan during other fungal infections, since (1,3)-beta-D-glucan is not a Pneumocystis-specific protein and may be less reliable in HIV-uninfected people.[Figure caption and citation for the preceding image starts]: Posteroanterior chest x-ray showing mild, reticular, bilateral pulmonary interstitial infiltratesFrom the collection of Matthew Gingo, UPMC [Citation ends]. [Figure caption and citation for the preceding image starts]: Posteroanterior chest x-ray showing severe, bilateral pulmonary interstitial infiltrates with pneumatocelesFrom the collection of Matthew Gingo, UPMC [Citation ends].
[Figure caption and citation for the preceding image starts]: Posteroanterior chest x-ray showing severe, bilateral pulmonary interstitial infiltrates with pneumatocelesFrom the collection of Matthew Gingo, UPMC [Citation ends]. [Figure caption and citation for the preceding image starts]: Computed tomography scan of the thorax showing bilateral pulmonary interstitial infiltrates and pneumatoceles (cysts), which are typical of Pneumocystis pneumonia (PCP)From the collection of Matthew Gingo, UPMC [Citation ends].
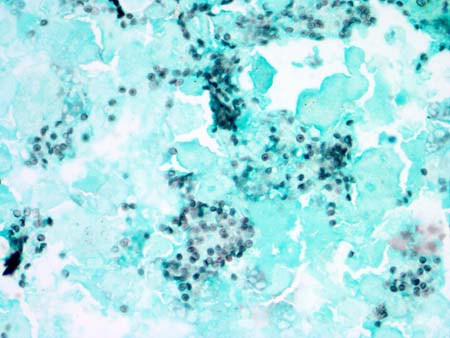
[Figure caption and citation for the preceding image starts]: Computed tomography scan of the thorax showing bilateral pulmonary interstitial infiltrates and pneumatoceles (cysts), which are typical of Pneumocystis pneumonia (PCP)From the collection of Matthew Gingo, UPMC [Citation ends].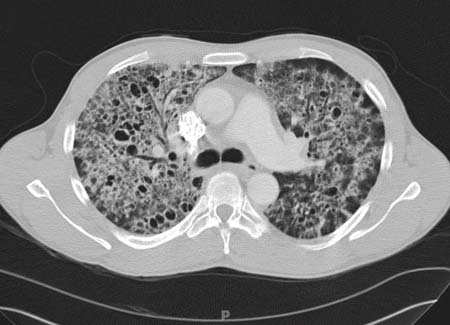 [Figure caption and citation for the preceding image starts]: Photomicrograph of bronchoalveolar lavage (BAL) fluid showing Pneumocystis cysts, stained black with Grocott-Gomori methenamine-silver stain (methyl green counterstain)From the collection of Matthew Gingo, UPMC [Citation ends].
[Figure caption and citation for the preceding image starts]: Photomicrograph of bronchoalveolar lavage (BAL) fluid showing Pneumocystis cysts, stained black with Grocott-Gomori methenamine-silver stain (methyl green counterstain)From the collection of Matthew Gingo, UPMC [Citation ends].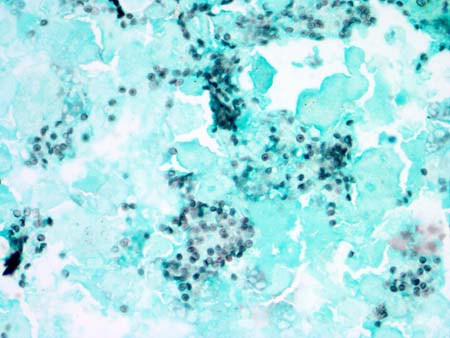
[Figure caption and citation for the preceding image starts]: Algorithm for the diagnosis of Pneumocystis pneumonia; bronchoalveolar lavage (BAL)Matthew Gingo, adapted from Singh, HIV Clinical Manual, 2003 [Citation ends].
 [Figure caption and citation for the preceding image starts]: Posteroanterior chest x-ray showing severe, bilateral pulmonary interstitial infiltrates with pneumatocelesFrom the collection of Matthew Gingo, UPMC [Citation ends].
[Figure caption and citation for the preceding image starts]: Posteroanterior chest x-ray showing severe, bilateral pulmonary interstitial infiltrates with pneumatocelesFrom the collection of Matthew Gingo, UPMC [Citation ends]. [Figure caption and citation for the preceding image starts]: Computed tomography scan of the thorax showing bilateral pulmonary interstitial infiltrates and pneumatoceles (cysts), which are typical of Pneumocystis pneumonia (PCP)From the collection of Matthew Gingo, UPMC [Citation ends].
[Figure caption and citation for the preceding image starts]: Computed tomography scan of the thorax showing bilateral pulmonary interstitial infiltrates and pneumatoceles (cysts), which are typical of Pneumocystis pneumonia (PCP)From the collection of Matthew Gingo, UPMC [Citation ends].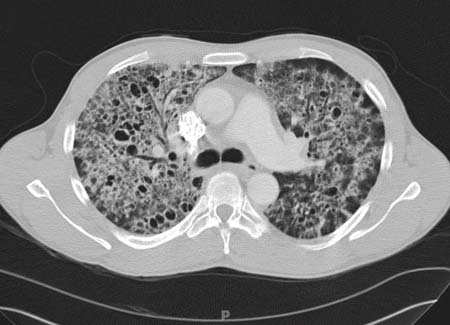 [Figure caption and citation for the preceding image starts]: Photomicrograph of bronchoalveolar lavage (BAL) fluid showing Pneumocystis cysts, stained black with Grocott-Gomori methenamine-silver stain (methyl green counterstain)From the collection of Matthew Gingo, UPMC [Citation ends].
[Figure caption and citation for the preceding image starts]: Photomicrograph of bronchoalveolar lavage (BAL) fluid showing Pneumocystis cysts, stained black with Grocott-Gomori methenamine-silver stain (methyl green counterstain)From the collection of Matthew Gingo, UPMC [Citation ends].