Ectopic pregnancy
- Overview
- Theory
- Diagnosis
- Management
- Follow up
- Resources
Treatment algorithm
Please note that formulations/routes and doses may differ between drug names and brands, drug formularies, or locations. Treatment recommendations are specific to patient groups: see disclaimer
tubal ectopic pregnancy: ruptured ectopic pregnancy or failed medical management
surgery
Preferred method is laparoscopy with either salpingostomy or salpingectomy, depending on the status of the contralateral tube and the desire for future fertility.[47]ACOG practice bulletin no. 193: tubal ectopic pregnancy. Obstet Gynecol. 2018 Mar;131(3):e91-103.
http://www.ncbi.nlm.nih.gov/pubmed/29470343?tool=bestpractice.com
[60]Elson CJ, Salim R, Potdar N, et al; Royal College of Obstetricians and Gynaecologists. Diagnosis and management of ectopic pregnancy: Green-top Guideline No. 21. BJOG. 2016 Dec;123(13):e15-55.
https://obgyn.onlinelibrary.wiley.com/doi/epdf/10.1111/1471-0528.14189
http://www.ncbi.nlm.nih.gov/pubmed/27813249?tool=bestpractice.com
[79]Gao M-XG. Laparoscopy versus laparotomy for ectopic pregnancy: a systematic review. Chin J Evid Based Med. 2008 Jul-Aug;14(4):309-19.[80]Mol F, Mol BW, Ankum WM, et al. Current evidence on surgery, systemic methotrexate and expectant management in the treatment of tubal ectopic pregnancy: a systematic review and meta-analysis. Hum Reprod Update. 2008 Jul-Aug;14(4):309-19.
http://humupd.oxfordjournals.org/content/14/4/309.full
http://www.ncbi.nlm.nih.gov/pubmed/18522946?tool=bestpractice.com
[81]Hajenius PJ, Mol BW, Mol BWJ, et al. Interventions for tubal ectopic pregnancy. Cochrane Database Syst Rev. 2007;(1):CD000324.
https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD000324/full
http://www.ncbi.nlm.nih.gov/pubmed/10796710?tool=bestpractice.com
[82]Mol F, van Mello NM, Strandell A, et al. Salpingotomy versus salpingectomy in women with tubal pregnancy (ESEP study): an open-label, multicentre, randomised controlled
trial. Lancet. 2014 Apr 26;383(9927):1483-9.
http://www.ncbi.nlm.nih.gov/pubmed/24499812?tool=bestpractice.com
[Figure caption and citation for the preceding image starts]: Surgical extraction of ectopic pregnancyFrom the collection of Dr Sina Haeri; used with permission [Citation ends].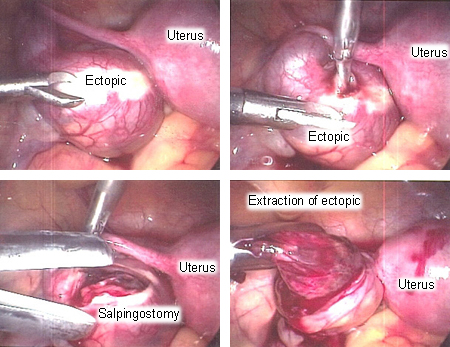 [Figure caption and citation for the preceding image starts]: Surgical extraction of ectopic pregnancyFrom the collection of Dr Sina Haeri; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Surgical extraction of ectopic pregnancyFrom the collection of Dr Sina Haeri; used with permission [Citation ends].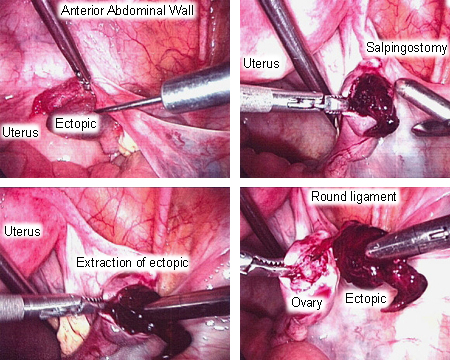
Salpingostomy should be considered for women with contralateral tube damage, as this is a risk factor for infertility.[63]National Institute for Health and Care Excellence. Ectopic pregnancy and miscarriage: diagnosis and initial management. Nov 2021 [internet publication]. https://www.nice.org.uk/guidance/ng126 [71]Po L, Thomas J, Mills K, et al. Guideline no. 414: management of pregnancy of unknown location and tubal and nontubal ectopic pregnancies. J Obstet Gynaecol Can. 2021 May;43(5):614-30.e1. http://www.ncbi.nlm.nih.gov/pubmed/33453378?tool=bestpractice.com There is no evidence to recommend salpingostomy over salpingectomy if the contralateral tube is normal.[71]Po L, Thomas J, Mills K, et al. Guideline no. 414: management of pregnancy of unknown location and tubal and nontubal ectopic pregnancies. J Obstet Gynaecol Can. 2021 May;43(5):614-30.e1. http://www.ncbi.nlm.nih.gov/pubmed/33453378?tool=bestpractice.com Future fertility and tubal patency rates in laparoscopically treated women is similar to that in the medically managed group.[47]ACOG practice bulletin no. 193: tubal ectopic pregnancy. Obstet Gynecol. 2018 Mar;131(3):e91-103. http://www.ncbi.nlm.nih.gov/pubmed/29470343?tool=bestpractice.com [57]Hendriks E, Rosenberg R, Prine L. Ectopic pregnancy: diagnosis and management. Am Fam Physician. 2020 May 15;101(10):599-606. https://www.aafp.org/afp/2020/0515/p599.html http://www.ncbi.nlm.nih.gov/pubmed/32412215?tool=bestpractice.com
Laparoscopic treatment of ectopic pregnancy in women with obesity (body mass index >30) is feasible and safe with proper patient selection and appropriate experience of the surgeon.[83]Yong PJ, Thurston J, Singh SS, et al. Guideline No. 386-Gynaecologic surgery in the obese patient. J Obstet Gynaecol Can. 2019 Sep;41(9):1356-70.e7. https://www.jogc.com/article/S1701-2163(18)31027-2/fulltext http://www.ncbi.nlm.nih.gov/pubmed/31443850?tool=bestpractice.com
Serial chorionic gonadotropin levels should be taken after salpingostomy until the levels are undetectable. A negative pregnancy test should be confirmed after salpingectomy.
post-surgical methotrexate
Treatment recommended for SOME patients in selected patient group
If serum chorionic gonadotropin levels do not return to undetectable after surgery, methotrexate is given.
Primary options
methotrexate: 50 mg/square meter of body surface area intramuscularly as a single dose
Rho(D) immune globulin
Treatment recommended for SOME patients in selected patient group
The American College of Emergency Physicians' Clinical Subcommittee review found insufficient evidence either for or against treatment with Rho(D) immune globulin in rhesus-negative women with ectopic pregnancy.[84]American College of Emergency Physicians Clinical Policies Subcommittee (Writing Committee) on Early Pregnancy: Hahn SA, Promes SB, Brown MD. Clinical policy: critical issues in the initial evaluation and management of patients presenting to the emergency department in early pregnancy. Ann Emerg Med. 2017 Feb;69(2):241-250.e20. http://www.annemergmed.com/article/S0196-0644(16)31344-0/fulltext http://www.ncbi.nlm.nih.gov/pubmed/28126120?tool=bestpractice.com However, the UK National Institute for Health and Care Excellence recommends Rho(D) immune globulin for all rhesus-negative women undergoing surgery for ectopic pregnancy, but not for those treated medically.[63]National Institute for Health and Care Excellence. Ectopic pregnancy and miscarriage: diagnosis and initial management. Nov 2021 [internet publication]. https://www.nice.org.uk/guidance/ng126
Primary options
Rho(D) immune globulin: 50 micrograms (250 international units) intramuscularly as a single dose as soon as possible or within 72 hours of the event
fluid resuscitation
Hemodynamic instability associated with a ruptured ectopic pregnancy results from severe hypovolemia secondary to blood loss.
Rapid volume repletion with isotonic solution and blood products is of paramount importance to avoid ischemic injury and multi-organ damage.
surgery
Treatment recommended for ALL patients in selected patient group
Type of surgery used depends on the experience and judgment of the surgeon and is decided on in consultation with the anesthetist.
Not unreasonable to undertake a laparotomy based on the availability of resources (including adequately trained personnel), with the specific procedure dependent on the location of the bleeding.
Rho(D) immune globulin
Treatment recommended for SOME patients in selected patient group
The American College of Emergency Physicians' Clinical Subcommittee review found insufficient evidence either for or against treatment with Rho(D) immune globulin in rhesus-negative women with ectopic pregnancy.[84]American College of Emergency Physicians Clinical Policies Subcommittee (Writing Committee) on Early Pregnancy: Hahn SA, Promes SB, Brown MD. Clinical policy: critical issues in the initial evaluation and management of patients presenting to the emergency department in early pregnancy. Ann Emerg Med. 2017 Feb;69(2):241-250.e20. http://www.annemergmed.com/article/S0196-0644(16)31344-0/fulltext http://www.ncbi.nlm.nih.gov/pubmed/28126120?tool=bestpractice.com However, the UK National Institute for Health and Care Excellence recommends Rho(D) immune globulin for all rhesus-negative women undergoing surgery for ectopic pregnancy, but not for those treated medically.[63]National Institute for Health and Care Excellence. Ectopic pregnancy and miscarriage: diagnosis and initial management. Nov 2021 [internet publication]. https://www.nice.org.uk/guidance/ng126
Primary options
Rho(D) immune globulin: 50 micrograms (250 international units) intramuscularly as a single dose as soon as possible or within 72 hours of the event
tubal ectopic pregnancy: moderate risk or failed expectant management
methotrexate
In women who are clinically stable with a nonruptured ectopic pregnancy, laparoscopic surgery and medical management are both reasonable management options and the decision should be guided by initial investigations and discussion with the woman.[47]ACOG practice bulletin no. 193: tubal ectopic pregnancy. Obstet Gynecol. 2018 Mar;131(3):e91-103. http://www.ncbi.nlm.nih.gov/pubmed/29470343?tool=bestpractice.com [63]National Institute for Health and Care Excellence. Ectopic pregnancy and miscarriage: diagnosis and initial management. Nov 2021 [internet publication]. https://www.nice.org.uk/guidance/ng126
Medical management is reserved for hemodynamically stable women who have a confirmed or high clinical suspicion of ectopic pregnancy, an unruptured mass, and no absolute contraindications to methotrexate.[47]ACOG practice bulletin no. 193: tubal ectopic pregnancy. Obstet Gynecol. 2018 Mar;131(3):e91-103. http://www.ncbi.nlm.nih.gov/pubmed/29470343?tool=bestpractice.com [71]Po L, Thomas J, Mills K, et al. Guideline no. 414: management of pregnancy of unknown location and tubal and nontubal ectopic pregnancies. J Obstet Gynaecol Can. 2021 May;43(5):614-30.e1. http://www.ncbi.nlm.nih.gov/pubmed/33453378?tool=bestpractice.com
It has been suggested that initial serum human chorionic gonadotropin (hCG) levels >5000 mIU/mL are predictive of an increased failure rate for medical management, particularly for single-dose regimens, and the American College of Obstetricians and Gynecologists states that high initial hCG concentration is a relative contraindication for methotrexate therapy.[47]ACOG practice bulletin no. 193: tubal ectopic pregnancy. Obstet Gynecol. 2018 Mar;131(3):e91-103. http://www.ncbi.nlm.nih.gov/pubmed/29470343?tool=bestpractice.com [74]Menon S, Colins J, Barnhart KT. Establishing a human chorionic gonadotropin cutoff to guide methotrexate treatment of ectopic pregnancy: a systematic review. Fertil Steril. 2007 Mar;87(3):481-4. http://www.ncbi.nlm.nih.gov/pubmed/17173905?tool=bestpractice.com
Ultrasound features that are suggestive of early gestational development or that indicate potential tubal rupture are also risk factors for treatment failure.[71]Po L, Thomas J, Mills K, et al. Guideline no. 414: management of pregnancy of unknown location and tubal and nontubal ectopic pregnancies. J Obstet Gynaecol Can. 2021 May;43(5):614-30.e1. http://www.ncbi.nlm.nih.gov/pubmed/33453378?tool=bestpractice.com These include visualized yolk sac or embryo, and significant pelvic free fluid.[71]Po L, Thomas J, Mills K, et al. Guideline no. 414: management of pregnancy of unknown location and tubal and nontubal ectopic pregnancies. J Obstet Gynaecol Can. 2021 May;43(5):614-30.e1. http://www.ncbi.nlm.nih.gov/pubmed/33453378?tool=bestpractice.com Ectopic pregnancy size >4 cm is considered a relative contraindication for medical management, but tubal rupture is unlikely if ectopic size is <2 cm and hCG level is <1855 mIU/mL.[47]ACOG practice bulletin no. 193: tubal ectopic pregnancy. Obstet Gynecol. 2018 Mar;131(3):e91-103. http://www.ncbi.nlm.nih.gov/pubmed/29470343?tool=bestpractice.com [75]Karadeniz RS, Tasci Y, Altay M, et al. Tubal rupture in ectopic pregnancy: is it predictable? Minerva Ginecol. 2015 Feb;67(1):13-9. http://www.ncbi.nlm.nih.gov/pubmed/25660430?tool=bestpractice.com
Other relative contraindications are embryonic cardiac activity on transvaginal ultrasound scan, high initial hCG concentration and refusal to accept blood transfusion.[47]ACOG practice bulletin no. 193: tubal ectopic pregnancy. Obstet Gynecol. 2018 Mar;131(3):e91-103. http://www.ncbi.nlm.nih.gov/pubmed/29470343?tool=bestpractice.com [60]Elson CJ, Salim R, Potdar N, et al; Royal College of Obstetricians and Gynaecologists. Diagnosis and management of ectopic pregnancy: Green-top Guideline No. 21. BJOG. 2016 Dec;123(13):e15-55. https://obgyn.onlinelibrary.wiley.com/doi/epdf/10.1111/1471-0528.14189 http://www.ncbi.nlm.nih.gov/pubmed/27813249?tool=bestpractice.com Most practitioners use the specific clinical scenario, in addition to ultrasound findings and hCG values, to determine whether medical management is an appropriate choice for an individual woman.
Certain conditions preclude a woman from undergoing treatment with methotrexate, including evidence of immunodeficiency, liver disease (with transaminases more than double normal), renal disease (creatinine >1.5 mg/dL), active peptic ulcer disease, significant pulmonary disease, or hematologic abnormalities (e.g., significant anemia, thrombocytopenia, or leukopenia).[47]ACOG practice bulletin no. 193: tubal ectopic pregnancy. Obstet Gynecol. 2018 Mar;131(3):e91-103. http://www.ncbi.nlm.nih.gov/pubmed/29470343?tool=bestpractice.com [57]Hendriks E, Rosenberg R, Prine L. Ectopic pregnancy: diagnosis and management. Am Fam Physician. 2020 May 15;101(10):599-606. https://www.aafp.org/afp/2020/0515/p599.html http://www.ncbi.nlm.nih.gov/pubmed/32412215?tool=bestpractice.com [71]Po L, Thomas J, Mills K, et al. Guideline no. 414: management of pregnancy of unknown location and tubal and nontubal ectopic pregnancies. J Obstet Gynaecol Can. 2021 May;43(5):614-30.e1. http://www.ncbi.nlm.nih.gov/pubmed/33453378?tool=bestpractice.com Other contraindications include intrauterine pregnancy, breast-feeding, sensitivity to methotrexate, and the inability to participate in follow-up.[47]ACOG practice bulletin no. 193: tubal ectopic pregnancy. Obstet Gynecol. 2018 Mar;131(3):e91-103. http://www.ncbi.nlm.nih.gov/pubmed/29470343?tool=bestpractice.com [60]Elson CJ, Salim R, Potdar N, et al; Royal College of Obstetricians and Gynaecologists. Diagnosis and management of ectopic pregnancy: Green-top Guideline No. 21. BJOG. 2016 Dec;123(13):e15-55. https://obgyn.onlinelibrary.wiley.com/doi/epdf/10.1111/1471-0528.14189 http://www.ncbi.nlm.nih.gov/pubmed/27813249?tool=bestpractice.com [63]National Institute for Health and Care Excellence. Ectopic pregnancy and miscarriage: diagnosis and initial management. Nov 2021 [internet publication]. https://www.nice.org.uk/guidance/ng126 [71]Po L, Thomas J, Mills K, et al. Guideline no. 414: management of pregnancy of unknown location and tubal and nontubal ectopic pregnancies. J Obstet Gynaecol Can. 2021 May;43(5):614-30.e1. http://www.ncbi.nlm.nih.gov/pubmed/33453378?tool=bestpractice.com
Once methotrexate has been administered, hCG levels should be serially monitored until they reach a nonpregnancy level.[47]ACOG practice bulletin no. 193: tubal ectopic pregnancy. Obstet Gynecol. 2018 Mar;131(3):e91-103. http://www.ncbi.nlm.nih.gov/pubmed/29470343?tool=bestpractice.com [63]National Institute for Health and Care Excellence. Ectopic pregnancy and miscarriage: diagnosis and initial management. Nov 2021 [internet publication]. https://www.nice.org.uk/guidance/ng126 This usually takes 2-4 weeks but can be up to 8 weeks.[76]Barnhart KT, Gosman G, Ashby R, et al. The medical management of ectopic pregnancy: a meta-analysis comparing "single dose" and "multidose" regimens. Obstet Gynecol. 2003 Apr;101(4):778-84. https://www.ncbi.nlm.nih.gov/pubmedhealth/PMH0020120 http://www.ncbi.nlm.nih.gov/pubmed/12681886?tool=bestpractice.com
During methotrexate treatment, vigorous activity and sexual intercourse should be avoided as this may potentially cause a rupture of ectopic pregnancy; pelvic and ultrasound scans should be limited; and women should avoid folic acid and nonsteroidal anti-inflammatory drugs as these reduce the efficacy of methotrexate. Gas-forming foods should also be avoided as they may produce pain that can be confused with symptoms of rupture. Sunlight exposure may risk methotrexate dermatitis.[47]ACOG practice bulletin no. 193: tubal ectopic pregnancy. Obstet Gynecol. 2018 Mar;131(3):e91-103. http://www.ncbi.nlm.nih.gov/pubmed/29470343?tool=bestpractice.com Once methotrexate treatment is complete, it may be advisable for women to delay attempts to conceive for 12 weeks or more to allow for maximum clearance.[71]Po L, Thomas J, Mills K, et al. Guideline no. 414: management of pregnancy of unknown location and tubal and nontubal ectopic pregnancies. J Obstet Gynaecol Can. 2021 May;43(5):614-30.e1. http://www.ncbi.nlm.nih.gov/pubmed/33453378?tool=bestpractice.com
At any given point in time, if a woman becomes clinically unstable, surgical intervention is indicated.[47]ACOG practice bulletin no. 193: tubal ectopic pregnancy. Obstet Gynecol. 2018 Mar;131(3):e91-103. http://www.ncbi.nlm.nih.gov/pubmed/29470343?tool=bestpractice.com Unsuccessful medical management is also managed surgically. However, a case-control series found that ultrasound-guided injection of methotrexate into the ectopic pregnancy, in addition to systemic methotrexate, may be a safe alternative to surgery in cases where there is a higher risk of treatment failure (e.g., higher hCG levels or fetal cardiac activity).[78]Wang M, Chen B, Wang J, et al. Nonsurgical management of live tubal ectopic pregnancy by ultrasound-guided local injection and systemic methotrexate. J Minim Invasive Gynecol. 2014 Jul-Aug;21(4):642-9. http://www.ncbi.nlm.nih.gov/pubmed/24462855?tool=bestpractice.com
Primary options
two-dose regimen
methotrexate: 50 mg/square meter of body surface area intramuscularly as a single dose on day 1 and day 4
More methotrexateMeasure hCG level on post-treatment day 4 and day 7, and if decrease is <15%, re-administer methotrexate on day 7 and check hCG level again on day 11. If the decrease between day 7 and day 11 is <15%, re-administer methotrexate on day 11 and check hCG level again on day 14. Consider surgical management if hCG is still not decreasing.[47]ACOG practice bulletin no. 193: tubal ectopic pregnancy. Obstet Gynecol. 2018 Mar;131(3):e91-103. http://www.ncbi.nlm.nih.gov/pubmed/29470343?tool=bestpractice.com
OR
single-dose regimen
methotrexate: 50 mg/square meter of body surface area intramuscularly as a single dose on day 1
More methotrexateMeasure hCG level on post-treatment day 4 and day 7, and if decrease is <15%, re-administer methotrexate and repeat hCG level. If hCG does not decrease after two doses, consider surgical management.[47]ACOG practice bulletin no. 193: tubal ectopic pregnancy. Obstet Gynecol. 2018 Mar;131(3):e91-103. http://www.ncbi.nlm.nih.gov/pubmed/29470343?tool=bestpractice.com
Secondary options
multiple-dose regimen
methotrexate: 1 mg/kg intramuscularly once daily on days 1, 3, 5, and 7
More methotrexateMeasure hCG level on days that dose is administered and continue until hCG level has decreased by 15% from its previous measurement (can discontinue methotrexate once hCG decrease is >15% between measurements). If no decrease after four doses, consider surgical management.[47]ACOG practice bulletin no. 193: tubal ectopic pregnancy. Obstet Gynecol. 2018 Mar;131(3):e91-103. http://www.ncbi.nlm.nih.gov/pubmed/29470343?tool=bestpractice.com
and
leucovorin: 0.1 mg/kg intramuscularly once daily on days 2, 4, 6, and 8
surgery
In women who are clinically stable with a nonruptured ectopic pregnancy, laparoscopic surgery and medical management are both reasonable management options and the choice should be guided by initial investigations and discussion with the individual woman.[47]ACOG practice bulletin no. 193: tubal ectopic pregnancy. Obstet Gynecol. 2018 Mar;131(3):e91-103. http://www.ncbi.nlm.nih.gov/pubmed/29470343?tool=bestpractice.com [63]National Institute for Health and Care Excellence. Ectopic pregnancy and miscarriage: diagnosis and initial management. Nov 2021 [internet publication]. https://www.nice.org.uk/guidance/ng126
If a woman shows signs of hemodynamic instability, symptoms of a ruptured ectopic mass, or signs of intraperitoneal bleeding then surgical intervention is required. It is also necessary if the woman has absolute contraindications to medical therapy.[47]ACOG practice bulletin no. 193: tubal ectopic pregnancy. Obstet Gynecol. 2018 Mar;131(3):e91-103. http://www.ncbi.nlm.nih.gov/pubmed/29470343?tool=bestpractice.com [63]National Institute for Health and Care Excellence. Ectopic pregnancy and miscarriage: diagnosis and initial management. Nov 2021 [internet publication]. https://www.nice.org.uk/guidance/ng126
The preferred method is laparoscopy with either salpingostomy or salpingectomy, depending on the status of the contralateral tube and the desire for future fertility.[47]ACOG practice bulletin no. 193: tubal ectopic pregnancy. Obstet Gynecol. 2018 Mar;131(3):e91-103. http://www.ncbi.nlm.nih.gov/pubmed/29470343?tool=bestpractice.com [60]Elson CJ, Salim R, Potdar N, et al; Royal College of Obstetricians and Gynaecologists. Diagnosis and management of ectopic pregnancy: Green-top Guideline No. 21. BJOG. 2016 Dec;123(13):e15-55. https://obgyn.onlinelibrary.wiley.com/doi/epdf/10.1111/1471-0528.14189 http://www.ncbi.nlm.nih.gov/pubmed/27813249?tool=bestpractice.com [79]Gao M-XG. Laparoscopy versus laparotomy for ectopic pregnancy: a systematic review. Chin J Evid Based Med. 2008 Jul-Aug;14(4):309-19.[80]Mol F, Mol BW, Ankum WM, et al. Current evidence on surgery, systemic methotrexate and expectant management in the treatment of tubal ectopic pregnancy: a systematic review and meta-analysis. Hum Reprod Update. 2008 Jul-Aug;14(4):309-19. http://humupd.oxfordjournals.org/content/14/4/309.full http://www.ncbi.nlm.nih.gov/pubmed/18522946?tool=bestpractice.com [81]Hajenius PJ, Mol BW, Mol BWJ, et al. Interventions for tubal ectopic pregnancy. Cochrane Database Syst Rev. 2007;(1):CD000324. https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD000324/full http://www.ncbi.nlm.nih.gov/pubmed/10796710?tool=bestpractice.com [82]Mol F, van Mello NM, Strandell A, et al. Salpingotomy versus salpingectomy in women with tubal pregnancy (ESEP study): an open-label, multicentre, randomised controlled trial. Lancet. 2014 Apr 26;383(9927):1483-9. http://www.ncbi.nlm.nih.gov/pubmed/24499812?tool=bestpractice.com Salpingostomy should be considered for women with contralateral tube damage, as this is a risk factor for infertility.[63]National Institute for Health and Care Excellence. Ectopic pregnancy and miscarriage: diagnosis and initial management. Nov 2021 [internet publication]. https://www.nice.org.uk/guidance/ng126 [71]Po L, Thomas J, Mills K, et al. Guideline no. 414: management of pregnancy of unknown location and tubal and nontubal ectopic pregnancies. J Obstet Gynaecol Can. 2021 May;43(5):614-30.e1. http://www.ncbi.nlm.nih.gov/pubmed/33453378?tool=bestpractice.com There is no evidence to recommend salpingostomy over salpingectomy if the contralateral tube is normal.[71]Po L, Thomas J, Mills K, et al. Guideline no. 414: management of pregnancy of unknown location and tubal and nontubal ectopic pregnancies. J Obstet Gynaecol Can. 2021 May;43(5):614-30.e1. http://www.ncbi.nlm.nih.gov/pubmed/33453378?tool=bestpractice.com
Laparoscopic treatment of ectopic pregnancy in women with obesity (body mass index >30) is feasible and safe with proper patient selection and appropriate experience of the surgeon.[83]Yong PJ, Thurston J, Singh SS, et al. Guideline No. 386-Gynaecologic surgery in the obese patient. J Obstet Gynaecol Can. 2019 Sep;41(9):1356-70.e7. https://www.jogc.com/article/S1701-2163(18)31027-2/fulltext http://www.ncbi.nlm.nih.gov/pubmed/31443850?tool=bestpractice.com
Serial chorionic gonadotropin levels should be taken after salpingostomy until the levels are undetectable. A negative pregnancy test should be confirmed after salpingectomy.
postsurgical methotrexate
Treatment recommended for SOME patients in selected patient group
If serum chorionic gonadotropin levels do not return to undetectable after surgery, methotrexate is given.
Primary options
methotrexate: 50 mg/square meter of body surface area intramuscularly as a single dose
Rho(D) immune globulin
Treatment recommended for SOME patients in selected patient group
The American College of Emergency Physicians' Clinical Subcommittee review found insufficient evidence either for or against treatment with Rho(D) immune globulin in rhesus-negative women with ectopic pregnancy.[84]American College of Emergency Physicians Clinical Policies Subcommittee (Writing Committee) on Early Pregnancy: Hahn SA, Promes SB, Brown MD. Clinical policy: critical issues in the initial evaluation and management of patients presenting to the emergency department in early pregnancy. Ann Emerg Med. 2017 Feb;69(2):241-250.e20. http://www.annemergmed.com/article/S0196-0644(16)31344-0/fulltext http://www.ncbi.nlm.nih.gov/pubmed/28126120?tool=bestpractice.com However, the UK National Institute for Health and Care Excellence recommends Rho(D) immune globulin for all rhesus-negative women undergoing surgery for ectopic pregnancy, but not for those treated medically.[63]National Institute for Health and Care Excellence. Ectopic pregnancy and miscarriage: diagnosis and initial management. Nov 2021 [internet publication]. https://www.nice.org.uk/guidance/ng126
Primary options
Rho(D) immune globulin: 50 micrograms (250 international units) intramuscularly as a single dose as soon as possible or within 72 hours of the event
tubal ectopic pregnancy: low risk
expectant management
Appropriate for low risk, hemodynamically stable, asymptomatic women (or with minimal pain) where there is objective evidence of resolution - usually demonstrated by a plateau or decrease in human chorionic gonadotropin (hCG) levels.[47]ACOG practice bulletin no. 193: tubal ectopic pregnancy. Obstet Gynecol. 2018 Mar;131(3):e91-103. http://www.ncbi.nlm.nih.gov/pubmed/29470343?tool=bestpractice.com [60]Elson CJ, Salim R, Potdar N, et al; Royal College of Obstetricians and Gynaecologists. Diagnosis and management of ectopic pregnancy: Green-top Guideline No. 21. BJOG. 2016 Dec;123(13):e15-55. https://obgyn.onlinelibrary.wiley.com/doi/epdf/10.1111/1471-0528.14189 http://www.ncbi.nlm.nih.gov/pubmed/27813249?tool=bestpractice.com [71]Po L, Thomas J, Mills K, et al. Guideline no. 414: management of pregnancy of unknown location and tubal and nontubal ectopic pregnancies. J Obstet Gynaecol Can. 2021 May;43(5):614-30.e1. http://www.ncbi.nlm.nih.gov/pubmed/33453378?tool=bestpractice.com In women with an initial hCG <200 mIU/mL, 88% will have spontaneous resolution, with a lower rate expected with higher hCG levels.[47]ACOG practice bulletin no. 193: tubal ectopic pregnancy. Obstet Gynecol. 2018 Mar;131(3):e91-103. http://www.ncbi.nlm.nih.gov/pubmed/29470343?tool=bestpractice.com [72]Korhonen J, Stenman UH, Ylöstalo P. Serum human chorionic gonadotropin dynamics during spontaneous resolution of ectopic pregnancy. Fertil Steril. 1994 Apr;61(4):632-6. http://www.ncbi.nlm.nih.gov/pubmed/8150103?tool=bestpractice.com The UK National Institute for Health and Care Excellence (NICE) has therefore made a strong recommendation for expectant management if serum hCG is ≤1000 IU/L but a conditional recommendation for expectant management if serum hCG is >1000 and <1500 IU/L.[63]National Institute for Health and Care Excellence. Ectopic pregnancy and miscarriage: diagnosis and initial management. Nov 2021 [internet publication]. https://www.nice.org.uk/guidance/ng126 [Evidence C]603bfbe3-6f6e-47d0-97db-e6de8339538dguidelineCWhat are the effects of expectant management versus medical management in women with tubal ectopic pregnancy?[63]National Institute for Health and Care Excellence. Ectopic pregnancy and miscarriage: diagnosis and initial management. Nov 2021 [internet publication]. https://www.nice.org.uk/guidance/ng126
One randomized controlled trial (RCT) of women with pregnancy of unknown location or ectopic pregnancy reported a success rate of 59% with expectant management compared with 76% following single-dose methotrexate.[73]van Mello NM, Mol F, Verhoeve HR, et al. Methotrexate or expectant management in women with an ectopic pregnancy or pregnancy of unknown location and low serum hCG concentrations? A randomized comparison. Hum Reprod. 2013 Jan;28(1):60-7. https://academic.oup.com/humrep/article/28/1/60/596638 http://www.ncbi.nlm.nih.gov/pubmed/23081873?tool=bestpractice.com A 2021 RCT of women with persisting pregnancy of unknown location reported a success rate of 51.5% with active management versus 36.0% with expectant management.[65]Barnhart KT, Hansen KR, Stephenson MD, et al. Effect of an active vs expectant management strategy on successful resolution of pregnancy among patients with a persisting pregnancy of unknown location: the ACT or NOT randomized clinical trial. JAMA. 2021 Aug 3;326(5):390-400. https://www.doi.org/10.1001/jama.2021.10767 http://www.ncbi.nlm.nih.gov/pubmed/34342619?tool=bestpractice.com
Serial hCG levels should be taken until levels are undetectable.
Failed expectant management is followed by medical treatment, if eligible, or surgical treatment. Expectant management should be ceased if a woman has increasing pain, hCG levels are not decreasing, or there are signs of tubal rupture.[47]ACOG practice bulletin no. 193: tubal ectopic pregnancy. Obstet Gynecol. 2018 Mar;131(3):e91-103. http://www.ncbi.nlm.nih.gov/pubmed/29470343?tool=bestpractice.com

Choose a patient group to see our recommendations
Please note that formulations/routes and doses may differ between drug names and brands, drug formularies, or locations. Treatment recommendations are specific to patient groups. See disclaimer
Use of this content is subject to our disclaimer