This section outlines the management of tubal ectopic pregnancy, which forms the majority of ectopic pregnancies. It should be noted that the most appropriate approach to management may differ for nontubal ectopic pregnancies.[68]Society for Maternal-Fetal Medicine. Miller R, Timor-Tritsch IE, et al. Society for Maternal-Fetal Medicine (SMFM) Consult Series #63: Cesarean scar ectopic pregnancy. Am J Obstet Gynecol. 2022 Jul;227(3):B9-B20.
https://www.ajog.org/article/S0002-9378(22)00478-1/fulltext
http://www.ncbi.nlm.nih.gov/pubmed/31972162?tool=bestpractice.com
[69]Long Y, Zhu H, Hu Y, et al. Interventions for non-tubal ectopic pregnancy. Cochrane Database Syst Rev. 2020 Jul 1;7:CD011174.
https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD011174.pub2/full
http://www.ncbi.nlm.nih.gov/pubmed/32609376?tool=bestpractice.com
The management of ectopic pregnancy depends on whether the woman is at low or medium risk of tubal rupture. In the presence of rupture, treatment depends on the hemodynamic stability of the woman.
Expectant management
Expectant management is appropriate for the low risk, hemodynamically stable, asymptomatic woman (or with minimal pain), where there is objective evidence of resolution - usually demonstrated by a plateau or decrease in human chorionic gonadotropin (hCG) levels.[47]ACOG practice bulletin no. 193: tubal ectopic pregnancy. Obstet Gynecol. 2018 Mar;131(3):e91-103.
http://www.ncbi.nlm.nih.gov/pubmed/29470343?tool=bestpractice.com
[63]National Institute for Health and Care Excellence. Ectopic pregnancy and miscarriage: diagnosis and initial management. Nov 2021 [internet publication].
https://www.nice.org.uk/guidance/ng126
[70]Elson CJ, Salim R, Potdar N, et al; Royal College of Obstetricians and Gynaecologists. Diagnosis and management of ectopic pregnancy: Green-top Guideline No. 21. BJOG. 2016 Dec;123(13):e15-e55.
https://obgyn.onlinelibrary.wiley.com/doi/epdf/10.1111/1471-0528.14189
http://www.ncbi.nlm.nih.gov/pubmed/27813249?tool=bestpractice.com
[71]Po L, Thomas J, Mills K, et al. Guideline no. 414: management of pregnancy of unknown location and tubal and nontubal ectopic pregnancies. J Obstet Gynaecol Can. 2021 May;43(5):614-30.e1.
http://www.ncbi.nlm.nih.gov/pubmed/33453378?tool=bestpractice.com
[Evidence C]603bfbe3-6f6e-47d0-97db-e6de8339538dguidelineCWhat are the effects of expectant management versus medical management in women with tubal ectopic pregnancy?[63]National Institute for Health and Care Excellence. Ectopic pregnancy and miscarriage: diagnosis and initial management. Nov 2021 [internet publication].
https://www.nice.org.uk/guidance/ng126
In women with an initial hCG <200 mIU/mL, 88% will have spontaneous resolution, with a lower rate expected with higher hCG levels.[47]ACOG practice bulletin no. 193: tubal ectopic pregnancy. Obstet Gynecol. 2018 Mar;131(3):e91-103.
http://www.ncbi.nlm.nih.gov/pubmed/29470343?tool=bestpractice.com
[72]Korhonen J, Stenman UH, Ylöstalo P. Serum human chorionic gonadotropin dynamics during spontaneous resolution of ectopic pregnancy. Fertil Steril. 1994 Apr;61(4):632-6.
http://www.ncbi.nlm.nih.gov/pubmed/8150103?tool=bestpractice.com
One randomized controlled trial (RCT) of women with pregnancy of unknown location or ectopic pregnancy reported a success rate of 59% with expectant management compared with 76% following single-dose methotrexate.[73]van Mello NM, Mol F, Verhoeve HR, et al. Methotrexate or expectant management in women with an ectopic pregnancy or pregnancy of unknown location and low serum hCG concentrations? A randomized comparison. Hum Reprod. 2013 Jan;28(1):60-7.
https://academic.oup.com/humrep/article/28/1/60/596638
http://www.ncbi.nlm.nih.gov/pubmed/23081873?tool=bestpractice.com
A 2021 RCT of women with persisting pregnancy of unknown location reported a success rate of 51.5% with active management versus 36.0% with expectant management.[65]Barnhart KT, Hansen KR, Stephenson MD, et al. Effect of an active vs expectant management strategy on successful resolution of pregnancy among patients with a persisting pregnancy of unknown location: the ACT or NOT randomized clinical trial. JAMA. 2021 Aug 3;326(5):390-400.
https://www.doi.org/10.1001/jama.2021.10767
http://www.ncbi.nlm.nih.gov/pubmed/34342619?tool=bestpractice.com
Failed expectant management is followed by medical or surgical treatment. Expectant management should be ceased if the woman has increasing pain, hCG levels are not decreasing, or there are signs of tubal rupture.[47]ACOG practice bulletin no. 193: tubal ectopic pregnancy. Obstet Gynecol. 2018 Mar;131(3):e91-103.
http://www.ncbi.nlm.nih.gov/pubmed/29470343?tool=bestpractice.com
Medical therapy
Methotrexate is a folic acid antagonist that disrupts rapidly dividing trophoblastic cells. Medical management with methotrexate is reserved for hemodynamically stable women who have a confirmed or high clinical suspicion of ectopic pregnancy, an unruptured mass, and no absolute contraindications to methotrexate.[47]ACOG practice bulletin no. 193: tubal ectopic pregnancy. Obstet Gynecol. 2018 Mar;131(3):e91-103.
http://www.ncbi.nlm.nih.gov/pubmed/29470343?tool=bestpractice.com
[71]Po L, Thomas J, Mills K, et al. Guideline no. 414: management of pregnancy of unknown location and tubal and nontubal ectopic pregnancies. J Obstet Gynaecol Can. 2021 May;43(5):614-30.e1.
http://www.ncbi.nlm.nih.gov/pubmed/33453378?tool=bestpractice.com
It has been suggested that initial serum hCG levels >5000 mIU/mL are predictive of an increased failure rate for medical management, particularly for single-dose regimens, and the American College of Obstetricians and Gynecologists states that high initial hCG concentration is a relative contraindication for methotrexate therapy.[47]ACOG practice bulletin no. 193: tubal ectopic pregnancy. Obstet Gynecol. 2018 Mar;131(3):e91-103.
http://www.ncbi.nlm.nih.gov/pubmed/29470343?tool=bestpractice.com
[74]Menon S, Colins J, Barnhart KT. Establishing a human chorionic gonadotropin cutoff to guide methotrexate treatment of ectopic pregnancy: a systematic review. Fertil Steril. 2007 Mar;87(3):481-4.
http://www.ncbi.nlm.nih.gov/pubmed/17173905?tool=bestpractice.com
Ultrasound features that are suggestive of early gestational development or that indicate potential tubal rupture are also risk factors for treatment failure.[71]Po L, Thomas J, Mills K, et al. Guideline no. 414: management of pregnancy of unknown location and tubal and nontubal ectopic pregnancies. J Obstet Gynaecol Can. 2021 May;43(5):614-30.e1.
http://www.ncbi.nlm.nih.gov/pubmed/33453378?tool=bestpractice.com
These include visualized yolk sac or embryo, and significant pelvic free fluid.[71]Po L, Thomas J, Mills K, et al. Guideline no. 414: management of pregnancy of unknown location and tubal and nontubal ectopic pregnancies. J Obstet Gynaecol Can. 2021 May;43(5):614-30.e1.
http://www.ncbi.nlm.nih.gov/pubmed/33453378?tool=bestpractice.com
Ectopic pregnancy size >4 cm is considered a relative contraindication for medical management, but tubal rupture is unlikely if ectopic size is <2 cm and hCG level is <1855 mIU/mL.[47]ACOG practice bulletin no. 193: tubal ectopic pregnancy. Obstet Gynecol. 2018 Mar;131(3):e91-103.
http://www.ncbi.nlm.nih.gov/pubmed/29470343?tool=bestpractice.com
[75]Karadeniz RS, Tasci Y, Altay M, et al. Tubal rupture in ectopic pregnancy: is it predictable? Minerva Ginecol. 2015 Feb;67(1):13-9.
http://www.ncbi.nlm.nih.gov/pubmed/25660430?tool=bestpractice.com
Other relative contraindications are embryonic cardiac activity on transvaginal ultrasound scan, high initial hCG concentration and refusal to accept blood transfusion.[47]ACOG practice bulletin no. 193: tubal ectopic pregnancy. Obstet Gynecol. 2018 Mar;131(3):e91-103.
http://www.ncbi.nlm.nih.gov/pubmed/29470343?tool=bestpractice.com
[70]Elson CJ, Salim R, Potdar N, et al; Royal College of Obstetricians and Gynaecologists. Diagnosis and management of ectopic pregnancy: Green-top Guideline No. 21. BJOG. 2016 Dec;123(13):e15-e55.
https://obgyn.onlinelibrary.wiley.com/doi/epdf/10.1111/1471-0528.14189
http://www.ncbi.nlm.nih.gov/pubmed/27813249?tool=bestpractice.com
Most practitioners use the specific clinical scenario, in addition to ultrasound findings and hCG values, to determine whether medical management is an appropriate choice for individual women.
Certain conditions preclude a woman from undergoing treatment with methotrexate, including evidence of immunodeficiency, liver disease (with transaminases more than double normal), renal disease (creatinine >1.5 mg/dL), active peptic ulcer disease, significant pulmonary disease, or hematologic abnormalities (e.g., significant anemia, thrombocytopenia, or leukopenia).[47]ACOG practice bulletin no. 193: tubal ectopic pregnancy. Obstet Gynecol. 2018 Mar;131(3):e91-103.
http://www.ncbi.nlm.nih.gov/pubmed/29470343?tool=bestpractice.com
[57]Hendriks E, Rosenberg R, Prine L. Ectopic pregnancy: diagnosis and management. Am Fam Physician. 2020 May 15;101(10):599-606.
https://www.aafp.org/afp/2020/0515/p599.html
http://www.ncbi.nlm.nih.gov/pubmed/32412215?tool=bestpractice.com
[71]Po L, Thomas J, Mills K, et al. Guideline no. 414: management of pregnancy of unknown location and tubal and nontubal ectopic pregnancies. J Obstet Gynaecol Can. 2021 May;43(5):614-30.e1.
http://www.ncbi.nlm.nih.gov/pubmed/33453378?tool=bestpractice.com
Other contraindications include intrauterine pregnancy, breast-feeding, sensitivity to methotrexate, and the inability to participate in follow-up.[47]ACOG practice bulletin no. 193: tubal ectopic pregnancy. Obstet Gynecol. 2018 Mar;131(3):e91-103.
http://www.ncbi.nlm.nih.gov/pubmed/29470343?tool=bestpractice.com
[63]National Institute for Health and Care Excellence. Ectopic pregnancy and miscarriage: diagnosis and initial management. Nov 2021 [internet publication].
https://www.nice.org.uk/guidance/ng126
[70]Elson CJ, Salim R, Potdar N, et al; Royal College of Obstetricians and Gynaecologists. Diagnosis and management of ectopic pregnancy: Green-top Guideline No. 21. BJOG. 2016 Dec;123(13):e15-e55.
https://obgyn.onlinelibrary.wiley.com/doi/epdf/10.1111/1471-0528.14189
http://www.ncbi.nlm.nih.gov/pubmed/27813249?tool=bestpractice.com
[71]Po L, Thomas J, Mills K, et al. Guideline no. 414: management of pregnancy of unknown location and tubal and nontubal ectopic pregnancies. J Obstet Gynaecol Can. 2021 May;43(5):614-30.e1.
http://www.ncbi.nlm.nih.gov/pubmed/33453378?tool=bestpractice.com
Protocols for methotrexate therapy include single-dose, two-dose, and fixed multiple-dose regimens.[47]ACOG practice bulletin no. 193: tubal ectopic pregnancy. Obstet Gynecol. 2018 Mar;131(3):e91-103.
http://www.ncbi.nlm.nih.gov/pubmed/29470343?tool=bestpractice.com
Although the regimens have not all been directly compared with each other, meta-analysis studies have shown the single-dose option to be slightly less effective (88%) than the multiple-dose option (93%), while causing fewer adverse effects.[47]ACOG practice bulletin no. 193: tubal ectopic pregnancy. Obstet Gynecol. 2018 Mar;131(3):e91-103.
http://www.ncbi.nlm.nih.gov/pubmed/29470343?tool=bestpractice.com
[71]Po L, Thomas J, Mills K, et al. Guideline no. 414: management of pregnancy of unknown location and tubal and nontubal ectopic pregnancies. J Obstet Gynaecol Can. 2021 May;43(5):614-30.e1.
http://www.ncbi.nlm.nih.gov/pubmed/33453378?tool=bestpractice.com
[76]Barnhart KT, Gosman G, Ashby R, et al. The medical management of ectopic pregnancy: a meta-analysis comparing "single dose" and "multidose" regimens. Obstet Gynecol. 2003 Apr;101(4):778-84.
https://www.ncbi.nlm.nih.gov/pubmedhealth/PMH0020120
http://www.ncbi.nlm.nih.gov/pubmed/12681886?tool=bestpractice.com
One meta-analysis demonstrated that the two-dose protocol was associated with higher treatment success than the single-dose protocol (odds ratio [OR] 1.84, 95% CI 1.13 to 3.00). The two-dose protocol was more successful in women with high hCG (OR 3.23, 95% CI 1.53 to 6.84) and in women with a large adnexal mass (OR 2.93, 95% CI 1.23 to 6.9). The length of follow-up was 7.9 days shorter for the two-dose protocol (95% CI -12.2 days to -3.5 days).[77]Alur-Gupta S, Cooney LG, Senapati S, et al. Two-dose versus single-dose methotrexate for treatment of ectopic pregnancy: a meta-analysis. Am J Obstet Gynecol. 2019 Aug;221(2):95-108.e2.
http://www.ncbi.nlm.nih.gov/pubmed/30629908?tool=bestpractice.com
The American College of Obstetricians and Gynecologists advise that the single-dose regimen may be an appropriate choice for women with low initial hCG or plateauing values, and the two-dose regimen an alternative which may be particularly suitable for women with an initial high hCG.[47]ACOG practice bulletin no. 193: tubal ectopic pregnancy. Obstet Gynecol. 2018 Mar;131(3):e91-103.
http://www.ncbi.nlm.nih.gov/pubmed/29470343?tool=bestpractice.com
A case-control series found that ultrasound-guided injection of methotrexate into the ectopic pregnancy, in addition to systemic methotrexate, may be a safe alternative to surgery in cases where there is a higher risk of treatment failure (e.g., higher hCG levels or fetal cardiac activity).[78]Wang M, Chen B, Wang J, et al. Nonsurgical management of live tubal ectopic pregnancy by ultrasound-guided local injection and systemic methotrexate. J Minim Invasive Gynecol. 2014 Jul-Aug;21(4):642-9.
http://www.ncbi.nlm.nih.gov/pubmed/24462855?tool=bestpractice.com
Once methotrexate has been administered, hCG levels should be serially monitored until they reach a nonpregnancy level.[47]ACOG practice bulletin no. 193: tubal ectopic pregnancy. Obstet Gynecol. 2018 Mar;131(3):e91-103.
http://www.ncbi.nlm.nih.gov/pubmed/29470343?tool=bestpractice.com
[63]National Institute for Health and Care Excellence. Ectopic pregnancy and miscarriage: diagnosis and initial management. Nov 2021 [internet publication].
https://www.nice.org.uk/guidance/ng126
This usually takes 2 to 4 weeks but can be up to 8 weeks.[76]Barnhart KT, Gosman G, Ashby R, et al. The medical management of ectopic pregnancy: a meta-analysis comparing "single dose" and "multidose" regimens. Obstet Gynecol. 2003 Apr;101(4):778-84.
https://www.ncbi.nlm.nih.gov/pubmedhealth/PMH0020120
http://www.ncbi.nlm.nih.gov/pubmed/12681886?tool=bestpractice.com
Further doses of methotrexate may be required depending on the regimen and response to treatment; hCG levels should be monitored to assess response. At any given point in time, if a woman becomes clinically unstable, surgical intervention is indicated.[47]ACOG practice bulletin no. 193: tubal ectopic pregnancy. Obstet Gynecol. 2018 Mar;131(3):e91-103.
http://www.ncbi.nlm.nih.gov/pubmed/29470343?tool=bestpractice.com
During methotrexate treatment, vigorous activity and sexual intercourse should be avoided as this may potentially cause a rupture of ectopic pregnancy; pelvic and ultrasound scans should be limited; and women should avoid folic acid and nonsteroidal anti-inflammatory drugs as these reduce the efficacy of methotrexate. Gas-forming foods should also be avoided as they may produce pain that can be confused with symptoms of rupture. Sunlight exposure may risk methotrexate dermatitis.[47]ACOG practice bulletin no. 193: tubal ectopic pregnancy. Obstet Gynecol. 2018 Mar;131(3):e91-103.
http://www.ncbi.nlm.nih.gov/pubmed/29470343?tool=bestpractice.com
Once methotrexate treatment is complete, it may be advisable for women to delay attempts to conceive for 12 weeks or more to allow for maximum clearance.[71]Po L, Thomas J, Mills K, et al. Guideline no. 414: management of pregnancy of unknown location and tubal and nontubal ectopic pregnancies. J Obstet Gynaecol Can. 2021 May;43(5):614-30.e1.
http://www.ncbi.nlm.nih.gov/pubmed/33453378?tool=bestpractice.com
Surgical therapy
In women who are clinically stable with a nonruptured ectopic pregnancy, laparoscopic surgery and medical management are both reasonable management options and the decision should be guided by initial investigations and discussion with the woman.[47]ACOG practice bulletin no. 193: tubal ectopic pregnancy. Obstet Gynecol. 2018 Mar;131(3):e91-103.
http://www.ncbi.nlm.nih.gov/pubmed/29470343?tool=bestpractice.com
[71]Po L, Thomas J, Mills K, et al. Guideline no. 414: management of pregnancy of unknown location and tubal and nontubal ectopic pregnancies. J Obstet Gynaecol Can. 2021 May;43(5):614-30.e1.
http://www.ncbi.nlm.nih.gov/pubmed/33453378?tool=bestpractice.com
If a woman shows signs of hemodynamic instability, symptoms of a ruptured ectopic mass, or signs of intraperitoneal bleeding then surgical intervention is required. It is also necessary if the woman has absolute contraindications to medical therapy.[47]ACOG practice bulletin no. 193: tubal ectopic pregnancy. Obstet Gynecol. 2018 Mar;131(3):e91-103.
http://www.ncbi.nlm.nih.gov/pubmed/29470343?tool=bestpractice.com
[71]Po L, Thomas J, Mills K, et al. Guideline no. 414: management of pregnancy of unknown location and tubal and nontubal ectopic pregnancies. J Obstet Gynaecol Can. 2021 May;43(5):614-30.e1.
http://www.ncbi.nlm.nih.gov/pubmed/33453378?tool=bestpractice.com
The preferred method is laparoscopy with either salpingostomy or salpingectomy, depending on the status of the contralateral tube and the desire for future fertility.[47]ACOG practice bulletin no. 193: tubal ectopic pregnancy. Obstet Gynecol. 2018 Mar;131(3):e91-103.
http://www.ncbi.nlm.nih.gov/pubmed/29470343?tool=bestpractice.com
[70]Elson CJ, Salim R, Potdar N, et al; Royal College of Obstetricians and Gynaecologists. Diagnosis and management of ectopic pregnancy: Green-top Guideline No. 21. BJOG. 2016 Dec;123(13):e15-e55.
https://obgyn.onlinelibrary.wiley.com/doi/epdf/10.1111/1471-0528.14189
http://www.ncbi.nlm.nih.gov/pubmed/27813249?tool=bestpractice.com
[79]Gao M-XG. Laparoscopy versus laparotomy for ectopic pregnancy: a systematic review. Chin J Evid Based Med. 2008 Jul-Aug;14(4):309-19.[80]Mol F, Mol BW, Ankum WM, et al. Current evidence on surgery, systemic methotrexate and expectant management in the treatment of tubal ectopic pregnancy: a systematic review and meta-analysis. Hum Reprod Update. 2008 Jul-Aug;14(4):309-19.
http://humupd.oxfordjournals.org/content/14/4/309.full
http://www.ncbi.nlm.nih.gov/pubmed/18522946?tool=bestpractice.com
[81]Hajenius PJ, Mol BW, Mol BWJ, et al. Interventions for tubal ectopic pregnancy. Cochrane Database Syst Rev. 2007;(1):CD000324.
https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD000324/full
http://www.ncbi.nlm.nih.gov/pubmed/10796710?tool=bestpractice.com
[82]Mol F, van Mello NM, Strandell A, et al. Salpingotomy versus salpingectomy in women with tubal pregnancy (ESEP study): an open-label, multicentre, randomised controlled
trial. Lancet. 2014 Apr 26;383(9927):1483-9.
http://www.ncbi.nlm.nih.gov/pubmed/24499812?tool=bestpractice.com
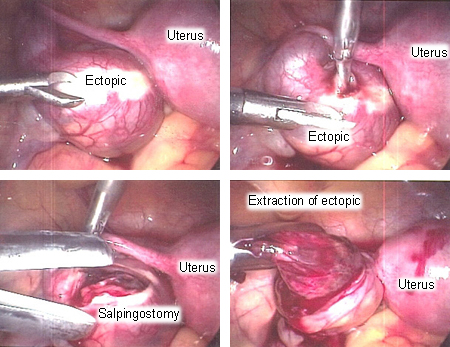
[Figure caption and citation for the preceding image starts]: Surgical extraction of ectopic pregnancyFrom the collection of Dr Sina Haeri; used with permission [Citation ends].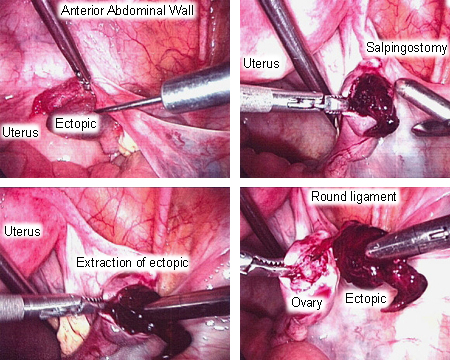 [Figure caption and citation for the preceding image starts]: Surgical extraction of ectopic pregnancyFrom the collection of Dr Sina Haeri; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Surgical extraction of ectopic pregnancyFrom the collection of Dr Sina Haeri; used with permission [Citation ends].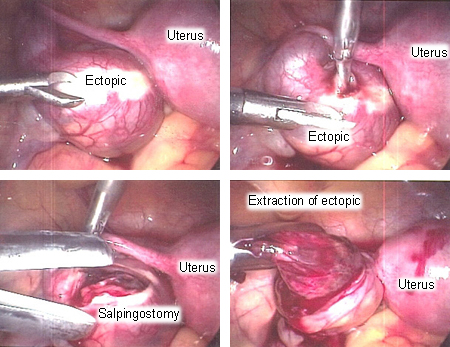
Salpingostomy should be considered for women with contralateral tube damage, as this is a risk factor for infertility.[63]National Institute for Health and Care Excellence. Ectopic pregnancy and miscarriage: diagnosis and initial management. Nov 2021 [internet publication].
https://www.nice.org.uk/guidance/ng126
[71]Po L, Thomas J, Mills K, et al. Guideline no. 414: management of pregnancy of unknown location and tubal and nontubal ectopic pregnancies. J Obstet Gynaecol Can. 2021 May;43(5):614-30.e1.
http://www.ncbi.nlm.nih.gov/pubmed/33453378?tool=bestpractice.com
There is no evidence to recommend salpingostomy over salpingectomy if the contralateral tube is normal.[71]Po L, Thomas J, Mills K, et al. Guideline no. 414: management of pregnancy of unknown location and tubal and nontubal ectopic pregnancies. J Obstet Gynaecol Can. 2021 May;43(5):614-30.e1.
http://www.ncbi.nlm.nih.gov/pubmed/33453378?tool=bestpractice.com
The future fertility and tubal patency rates in laparoscopically treated women are similar to those of the medically managed group.[47]ACOG practice bulletin no. 193: tubal ectopic pregnancy. Obstet Gynecol. 2018 Mar;131(3):e91-103.
http://www.ncbi.nlm.nih.gov/pubmed/29470343?tool=bestpractice.com
[57]Hendriks E, Rosenberg R, Prine L. Ectopic pregnancy: diagnosis and management. Am Fam Physician. 2020 May 15;101(10):599-606.
https://www.aafp.org/afp/2020/0515/p599.html
http://www.ncbi.nlm.nih.gov/pubmed/32412215?tool=bestpractice.com
Serial hCG measurements are required after salpingostomy to detect any persistent trophoblastic tissue, with consideration of methotrexate administration if levels plateau or rise.[47]ACOG practice bulletin no. 193: tubal ectopic pregnancy. Obstet Gynecol. 2018 Mar;131(3):e91-103.
http://www.ncbi.nlm.nih.gov/pubmed/29470343?tool=bestpractice.com
[70]Elson CJ, Salim R, Potdar N, et al; Royal College of Obstetricians and Gynaecologists. Diagnosis and management of ectopic pregnancy: Green-top Guideline No. 21. BJOG. 2016 Dec;123(13):e15-e55.
https://obgyn.onlinelibrary.wiley.com/doi/epdf/10.1111/1471-0528.14189
http://www.ncbi.nlm.nih.gov/pubmed/27813249?tool=bestpractice.com
Hemodynamic instability associated with a ruptured ectopic pregnancy results from severe hypovolemia secondary to blood loss. As such, the management of these women involves stabilization with emergency fluid resuscitation and immediate transfer to the operating suite. Rapid volume repletion with isotonic solution and blood products is of paramount importance to avoid ischemic injury and multiorgan damage.
Although laparoscopy is the standard surgical approach for the treatment of an ectopic pregnancy in a hemodynamically stable woman (even in the presence of hemoperitoneum), in hemodynamically unstable women the type of surgery used depends on the experience and judgment of the surgeon and is decided on in consultation with the anesthesiologist. Laparoscopic treatment of ectopic pregnancy in women with obesity (body mass index >30) is feasible and safe with proper patient selection and appropriate experience of the surgeon.[83]Yong PJ, Thurston J, Singh SS, et al. Guideline No. 386-Gynaecologic surgery in the obese patient. J Obstet Gynaecol Can. 2019 Sep;41(9):1356-70.e7.
https://www.jogc.com/article/S1701-2163(18)31027-2/fulltext
http://www.ncbi.nlm.nih.gov/pubmed/31443850?tool=bestpractice.com
It is not unreasonable to undertake a laparotomy based on the availability of resources (including adequately trained personnel), with the specific procedure dependent on the location of the bleeding.[71]Po L, Thomas J, Mills K, et al. Guideline no. 414: management of pregnancy of unknown location and tubal and nontubal ectopic pregnancies. J Obstet Gynaecol Can. 2021 May;43(5):614-30.e1.
http://www.ncbi.nlm.nih.gov/pubmed/33453378?tool=bestpractice.com
Rhesus-negative women
The American College of Emergency Physicians' Clinical Subcommittee review found insufficient evidence either for or against treatment with Rho(D) immune globulin in rhesus-negative women with ectopic pregnancy.[84]American College of Emergency Physicians Clinical Policies Subcommittee (Writing Committee) on Early Pregnancy: Hahn SA, Promes SB, Brown MD. Clinical policy: critical issues in the initial evaluation and management of patients presenting to the emergency department in early pregnancy. Ann Emerg Med. 2017 Feb;69(2):241-250.e20.
http://www.annemergmed.com/article/S0196-0644(16)31344-0/fulltext
http://www.ncbi.nlm.nih.gov/pubmed/28126120?tool=bestpractice.com
However, NICE recommends Rho(D) immune globulin for all rhesus-negative women undergoing surgery for ectopic pregnancy, but not for those treated medically.[63]National Institute for Health and Care Excellence. Ectopic pregnancy and miscarriage: diagnosis and initial management. Nov 2021 [internet publication].
https://www.nice.org.uk/guidance/ng126
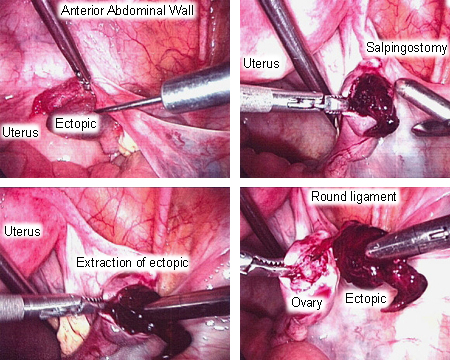 [Figure caption and citation for the preceding image starts]: Surgical extraction of ectopic pregnancyFrom the collection of Dr Sina Haeri; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Surgical extraction of ectopic pregnancyFrom the collection of Dr Sina Haeri; used with permission [Citation ends].