Approach
Pregnancy must be confirmed by either urine or serum human chorionic gonadotropin (hCG) testing.[40] A few cases have been reported of ruptured ectopic pregnancy with a negative urine pregnancy test, but this is very rare.[41] A serum hCG should be obtained if clinical suspicion is high. Classic symptoms and signs are pain, vaginal bleeding, and amenorrhea. Hemodynamic instability and cervical motion tenderness may indicate rupture or imminent rupture. Transvaginal ultrasound (TVUS) may confirm the diagnosis. If there is no positive identification of an ectopic pregnancy on ultrasound but clinical suspicion remains, then serial quantitative hCG, and TVUS, may aid clinical decision-making.
History
Key risk factors include prior ectopic pregnancy, prior tubal sterilization surgery, in utero diethylstilbestrol exposure of the mother, multiple sexual partners, prior pelvic inflammatory disease or infections (e.g., chlamydia), salpingitis, IUD use at the point of conception, subfertility and IVF treatment, and smoking.
Symptoms generally appear 6 to 8 weeks after the last normal menstrual period, but they can occur much later in cases of nontubal ectopic pregnancy.
Usual symptoms include abdominal pain, amenorrhea, and vaginal bleeding, but these may also be associated with early pregnancy loss, and further investigation is needed to distinguish the two entities. In one study evaluating a standard questionnaire, vomiting during pain, diffuse abdominal pain, acute pain for longer than 30 minutes, and flashing pain contributed independently to the diagnosis of ruptured ectopic pregnancy.[11][42]
There are a number of atypical presentations in cases of ruptured ectopic pregnancy. Leakage of blood from the implantation site may provide irritation to the diaphragm, leading to referred shoulder pain. Collection of blood in the posterior cul-de-sac can manifest as a continuous urge to defecate. Symptoms of shock, including lightheadedness, may indicate severe hemorrhage and tubal rupture. Other atypical presentations include right upper quadrant pain and seizures.
There have been numerous case reports of ectopic pregnancies following both total and supracervical hysterectomies. Although this condition is extremely rare, clinicians should be aware of the possibility of its occurrence. Provided that at least one ovary has been retained, a pregnancy test should be performed for a woman of reproductive age who has previously had a hysterectomy and presents with abdominal pain of unknown origin.[9]
Physical exam
Often unremarkable in cases of unruptured ectopic pregnancy, although the pelvic exam is an important part of the evaluation.[43][44] Some women may present with cervical motion tenderness, adnexal mass, or tenderness.[45] If the uterine cervix is found to be dilated during the exam, this may suggest a miscarriage.
Red flags suggesting possible rupture include unstable vital signs (orthostatic changes), blood in the vaginal vault, or signs of intraperitoneal bleeding (e.g., acute abdomen, shoulder pain, cervical motion tenderness).
If hemodynamic instability is present and rupture is suspected, subsequent diagnostic steps may be expedited or bypassed in favor of urgent fluid resuscitation and surgical intervention.
Key tests
Once pregnancy is confirmed by either urine or serum hCG testing, high-resolution TVUS exam is used to determine the location of the pregnancy.[40] Transabdominal ultrasound may also be used; however, it is less sensitive and specific than TVUS.[46] If an intrauterine gestation is visualized, which can be either viable or nonviable, the likelihood of having an ectopic pregnancy is extremely low, with the exception of heterotopic pregnancy (particularly after IVF treatment).[45]
An ectopic pregnancy can be definitively diagnosed via ultrasound when a gestational sac with a yolk sac, or embryo, or both, is noted in the adnexa.[47] Not all ectopic pregnancies can be visualized on ultrasound; however, with increasingly high-resolution ultrasound and expert sonography, studies have shown that TVUS is both highly sensitive and specific in the diagnosis of ectopic pregnancy. However, there remains a significant proportion of cases (between 5% and 42%) where neither an intrauterine nor an ectopic pregnancy can be visualized on ultrasound. In these cases, the descriptive term pregnancy of unknown location (PUL) is used.[48][49][Figure caption and citation for the preceding image starts]: Ultrasound image of ectopic pregnancyFrom the collection of Dr Melissa Fries; used with permission [Citation ends].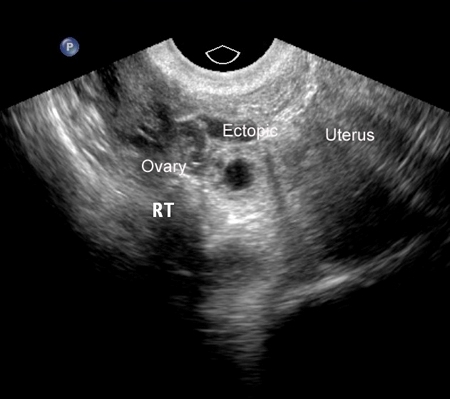 [Figure caption and citation for the preceding image starts]: Ultrasound image of ectopic pregnancyFrom the collection of Dr Melissa Fries; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Ultrasound image of ectopic pregnancyFrom the collection of Dr Melissa Fries; used with permission [Citation ends].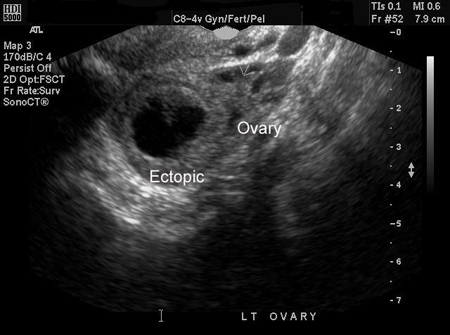 [Figure caption and citation for the preceding image starts]: Ultrasound image of ectopic pregnancyFrom the collection of Dr Melissa Fries; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Ultrasound image of ectopic pregnancyFrom the collection of Dr Melissa Fries; used with permission [Citation ends].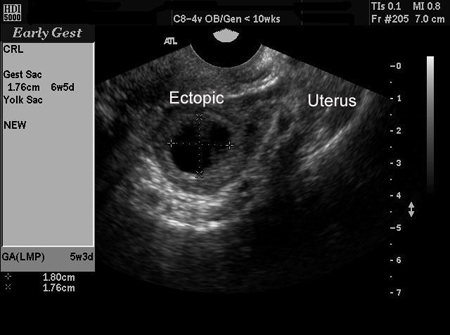
The serum concentration of hCG when a pregnancy is expected to be visible on an ultrasound scan is known as the "discriminatory hCG level." When a gestational sac is absent on ultrasound and serum hCG is above this level, this strongly suggests either an early pregnancy loss or ectopic pregnancy.[47] High-resolution transvaginal scanning makes it potentially possible to detect an ectopic pregnancy with hCG values well below the traditional thresholds.[50][51] However, there have also been reports of an intrauterine gestational sac being detected on a follow-up scan when previously no sac was visible with serum hCG levels above the discriminatory level.[47] In the case of a woman with multiple gestation, there will also be higher hCG levels compared to a single gestation. In view of this, it is recommended that if discriminatory levels are used to diagnose ectopic pregnancy a conservatively high value, such as 3500 mIU/mL, should be used to reduce the risk of misdiagnosis.[47] A single hCG cannot differentiate intrauterine and ectopic pregnancy.[52] All pregnancies should be considered potentially viable until they are diagnosed as not.
The expected rise in serum hCG in a normal pregnancy can depend on the initial values. If the initial hCG level is <1500 mIU/mL, then an increase of 49% or higher would be expected over 2 days; whereas, with an initial level of >3000 mIU/mL, the expected increase would be ≥33% over 2 days.[53] In 99% of viable intrauterine pregnancies, there will be a greater rise in hCG levels over a 48-hour period than these minimum thresholds; a lower rate of increase should raise suspicion of an ectopic pregnancy or early pregnancy loss. However, this level should not be considered a threshold for the diagnosis of a nonviable pregnancy.[53][54] It is important to also remember that, when there is an expected rise in serum hCG or falling levels, this does not rule out the possibility of ectopic pregnancy.[55] Caution is advised when interpreting the result, as one study revealed that up to 27% of women diagnosed with an ectopic pregnancy had hCG curves resembling a normal pregnancy.[53][56][57]
In regard to PUL, at the conclusion of the index pregnancy, the final diagnosis should be classified as follows:[49]
Visualized ectopic pregnancy on either ultrasound or during surgery
Visualized intrauterine pregnancy, regardless of viability
Spontaneously resolved PUL.
For persisting PUL, the final outcome of this category should be classified based on clinical management:
Nonvisualized ectopic pregnancy: based on persistent or rising hCG levels after uterine evacuation and no evidence of trophoblastic tissue
Treated persistent PUL: describes women who receive methotrexate without confirming the location of the ultrasound, histology, or surgery
Resolved persistent PUL: describes women whose serum hCG levels normalize with expectant management
Histologic intrauterine pregnancy: based on dilation and curettage results.
A steady decrease in hCG values (i.e., a decrease of 50% in 48 hours) suggests a failing pregnancy (miscarriage). This could be intrauterine, but may also represent a spontaneously resolving ectopic pregnancy.[47][58] On the other hand, a suboptimal increase (i.e., <49% rise in 48 hours if the initial hCG level is <1500 mIU/mL, <40% rise in 48 hours for an initial hCG level of between 1500 and 3000 mIU/mL or <33% rise in 48 hours if the initial hCG is >3000 mIU/mL) or plateauing of hCG values may suggest an ectopic pregnancy or pregnancy loss.[47][59]
Ancillary testing
Progesterone has been used in many studies as an adjunct to diagnosis for ectopic pregnancy. However, the UK Royal College of Obstetricians and Gynaecologists advises that a serum progesterone level is not useful in identifying ectopic pregnancy and it is not listed as a recommended investigation for tubal ectopic pregnancy by the American College of Obstetricians and Gynecologists.[47][60]
Progesterone levels can be useful in indicating the viability of the pregnancy. However, they are a poor predictor of the location of the pregnancy. Levels <6.3 nanograms/mL have a high positive predictive value for failing pregnancies.[48]
Although still at the experimental and research stage, attempts are underway to develop a validated mathematical model employing several maternal serum biomarkers such as progesterone, inhibin A , activin A, vascular endothelial growth factor, and pregnancy-associated plasma protein A to accurately predict the possibility of ectopic pregnancy.[61]
Commercially available urine tests that assess the ratio of intact hCG, beta core fragments, nicked beta fragments, and beta-hCG isoforms were not found to be useful in confirming an abnormal first trimester pregnancy in an emergency room setting.[62]
Use of this content is subject to our disclaimer