Tests
1st tests to order
chest x-ray
Test
First-line test.
Is almost always abnormal in immunocompetent individuals. Typically presents as fibronodular opacities in upper lobes with or without cavitation. Atypical pattern includes opacities in middle or lower lobes, hilar or paratracheal lymphadenopathy, and/or pleural effusion.[Figure caption and citation for the preceding image starts]: Pulmonary TB with cavitationFrom the personal collection of David Horne and Masahiro Narita; used with permission [Citation ends].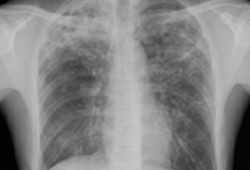 [Figure caption and citation for the preceding image starts]: Opacities in right lower lobe in a patient with pulmonary TB and diabetesFrom the personal collection of David Horne and Masahiro Narita; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Opacities in right lower lobe in a patient with pulmonary TB and diabetesFrom the personal collection of David Horne and Masahiro Narita; used with permission [Citation ends]. [Figure caption and citation for the preceding image starts]: Right hilar adenopathy in a childFrom the personal collection of David Horne and Masahiro Narita; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Right hilar adenopathy in a childFrom the personal collection of David Horne and Masahiro Narita; used with permission [Citation ends]. [Figure caption and citation for the preceding image starts]: Right-sided pleural effusionFrom the personal collection of David Horne and Masahiro Narita; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Right-sided pleural effusionFrom the personal collection of David Horne and Masahiro Narita; used with permission [Citation ends].
Studies indicate that an atypical chest radiograph is a reflection of immunosuppression, rather than primary TB.[50]
HIV status is associated with lymphadenopathy, effusion, lower lung zone involvement, and miliary pattern; cavitary lesions are less often seen. Patients with advanced HIV may have a normal chest x-ray.[50][51]
Result
abnormal typical for TB; abnormal atypical for TB; or normal
sputum acid-fast bacilli smear
Test
Sputum may be spontaneously expectorated or induced (with appropriate precautions to prevent transmission), and three specimens should be collected (minimum 8 hours apart, including an early morning specimen, which is the best to detect Mycobacterium tuberculosis).[12]
The examiner looks for acid-fast bacilli (AFB) (the stained dye remains even after exposure to acidic media) consistent with M tuberculosis. Other organisms, especially nontuberculous mycobacteria (e.g., Mycobacterium kansasii and Mycobacterium avium), are positive on AFB stain. Thus, a positive AFB smear is not specific in populations with low TB prevalence.
If sputum is positive for AFB, the results will be graded from 1+ to 3+ or 4+ depending on number of organisms seen and grading scale. Smear positivity and its grading may help estimate the degree of infectiousness and burden of TB. In the US, sensitivity is 50% to 60%.[52]
Result
positive for AFB
sputum culture
Test
The most sensitive and specific test. Should always be performed as it is required for precise identification and for drug susceptibility testing.
Growth on solid media may take 4 to 8 weeks; growth in liquid media may be detected in 1 to 3 weeks. Growth on solid media if positive is reported on quantitation scale (1+ to 4+).
While on treatment, the patient should have sputum cultures performed at least monthly until two consecutive cultures are negative.[9]
Result
positive; no growth; or other mycobacteria
CBC (complete blood count)
Test
Leukocytosis (without left shift) and anemia each seen in 10%.[53] Other abnormalities include elevated monocyte and eosinophil counts. Pancytopenia may be seen in disseminated disease.
Result
elevated WBC; low Hb
nucleic acid amplification tests (NAAT)
Test
NAAT should be performed on at least one respiratory specimen when a diagnosis of TB is being considered. NAAT may speed the diagnosis in smear-negative cases and may be helpful to differentiate nontuberculous mycobacteria when sputum is AFB smear positive but NAAT negative.[31] Genotyping might be considered useful in outbreaks of TB to identify transmission of TB, especially when contact had not been appreciated in the course of epidemiologic investigations. Several rapid NAATs are available and some are also able to detect genes encoding resistance to TB drugs.[32][33][34]
Result
positive forM tuberculosis
Tests to consider
gastric aspirate
Test
Used in patients unable to produce sputum (e.g., young children). Based on overnight collection of bronchial secretions in the stomach. In early morning after 8 to 10 hours of fasting, 10 to 20 mL of sterile water infused into stomach through nasogastric tube and 50 mL aspirated. After neutralization, the aspirate is sent for culture.[12]
Result
positive for acid-fast bacilli
bronchoscopy and bronchoalveolar lavage
Test
Many studies demonstrate that sputum induction has better sensitivity for TB diagnosis than bronchoscopy and bronchoalveolar lavage (BAL).[12] BAL may be indicated in patients in whom sputum induction is unsuccessful or in whom smear and nucleic acid amplification tests are negative. Bronchoscopy is useful when other diagnoses strongly considered or in patients in whom pulmonary TB is still suspected after other methods proved nondiagnostic.
Highest yield sputum collection is first expectorated sputum following bronchoscopy.
Transbronchial lung biopsies are useful in the diagnosis of miliary disease as granulomas may be seen and/or Mycobacterium tuberculosis may be cultured.
Result
positive for acid-fast bacilli
stool testing
Test
While not routinely used in the US, use of stool samples is an alternative to respiratory specimens in the diagnosis of pulmonary TB (sputum is swallowed and M tuberculosis may pass through the gastrointestinal tract). One systematic review evaluating AFB-smear, culture, and NAAT (polymerase chain reaction [PCR]) testing of stool in pulmonary TB found a pooled sensitivity of one or more of the three tests was 79.1% (95% CI 61.5 to 92.5).[41] The sensitivity of stool microscopy, PCR, and culture was 41.1% (95% CI 24.9 to 58.2), 89.7% (95% CI 81.4 to 95.9), and 38.0% (95% CI 26.2 to 50.6) respectively.[41]
Result
positive for acid-fast bacilli and/or M tuberculosis
empiric treatment
Test
Diagnosis of active TB may be made based on clinical history including risk factors and radiographic findings.
Other diagnoses and evaluation with bronchoscopy and bronchoscopy and bronchoalveolar lavage should be considered if the suspicion for TB is not high enough or differential diagnoses, including concurrent pathology, affect clinical management.
When clinical suspicion of pulmonary TB is high, empiric TB treatment with standard regimen (isoniazid, rifampin, pyrazinamide, ethambutol) is generally initiated after collecting optimal sputum samples.
For culture-negative cases who are placed on empiric TB treatment, a clinical and radiographic response should be re-evaluated at 2 months of treatment, and isoniazid and rifampin continued for at least 2 more months (4 months of treatment in total) if there is a clinical and radiographic response. If there was not a response at 2 months of treatment, TB medications should be stopped and another diagnosis looked for.[9]
Result
clinical response
drug susceptibility testing
Test
Perform on initial isolates.
Result
drug sensitivities
genotyping
Test
Useful in the investigation of outbreaks, contacts, and laboratory cross-contamination, as well as epidemiologic studies. There is evidence that some strain "families" of TB may have increased virulence.
Currently, the US Centers for Disease Control and Prevention and other laboratories use spoligotyping (a polymerase chain reaction method for simultaneous detection and typing of strains ofMycobacterium tuberculosis) and/or a technique called mycobacterial interspersed repetitive units-variable number tandem repeats (MIRU-VNTR) as initial genotyping techniques.
Result
genotype of infective agent
HIV test
Test
It is recommended that all patients with TB have an HIV test within 2 months of diagnosis of TB.[9] In the setting of HIV infection, pulmonary TB is an AIDS-defining diagnosis.
HIV infection may alter the treatment of TB and treatment of HIV infection may lead to more rapid resolution of TB.[9]
Result
positive or negative
lateral flow urine lipoarabinomannan (LF-LAM) assay
Test
Lateral flow tests that detect lipoarabinomannan (LAM) antigen in urine have emerged as potential point-of-care tests. One Cochrane review found the lateral flow urine lipoarabinomannan (LF-LAM) assay to have a sensitivity of 42% in diagnosing TB in HIV-positive individuals with TB symptoms, and 35% in HIV-positive individuals not assessed for TB symptoms.[39]
[  ]
[
]
[  ]
The World Health Organization (WHO) recommends that LF-LAM can be used to assist in the diagnosis of active TB in HIV-positive adults, adolescents, and children.[32] This approach is supported by another Cochrane review, which found reductions in mortality and an increase in treatment initiation with use of LF-LAM in inpatient and outpatient settings.[40]
]
The World Health Organization (WHO) recommends that LF-LAM can be used to assist in the diagnosis of active TB in HIV-positive adults, adolescents, and children.[32] This approach is supported by another Cochrane review, which found reductions in mortality and an increase in treatment initiation with use of LF-LAM in inpatient and outpatient settings.[40]
Culture would still be required for drug susceptibility testing.
Result
positive
CT of chest
Test
Not part of the standard evaluation but may assist in assessing for other diagnoses. May show same patterns of disease as seen with chest x-ray. In addition, there may be a tree-in-bud pattern. Cavities that are seen on CT, but are not noted on chest x-ray, do not place the patient in the category of cavitary disease.
Result
abnormal
tuberculin skin testing
Test
Used for investigation for latent TB infection. A negative tuberculin skin test (TST) does not rule out active TB as false-negative results occur in 20% to 25% of patients with active pulmonary TB.[43] The sensitivity of TST in diagnosing active TB is around 75% to 80% and its inability to distinguish between latent infection and active disease limits its usefulness.
The TST uses purified protein derivative to evaluate for delayed hypersensitivity response in order to diagnose prior exposure to TB. Different cutoffs in size of induration are used to define a positive test depending on the patient's risk factors.
There is diminished immune response in patients with active TB, especially with increased age, poor nutrition, and advanced disease.[54]
Result
millimeters of induration; 0-4 mm generally considered negative and no treatment indicated, though may be considered positive in child under 5 years of age at high risk of TB infection; ≥5 mm considered positive in situation of HIV infection, contact with infectious TB case within past 2 years, fibrotic opacities on chest x-ray consistent with untreated but healed TB, severely immunosuppressed patients (e.g., organ transplant, tumor necrosis factor-alpha-blocker, prednisone ≥15 mg/day for 1 month or longer); ≥10 mm considered positive in situation of TST conversion within 2 years, medical or social conditions associated with increased risk of progression to active TB (e.g., diabetes, malnutrition, cigarette smoking, alcohol consumption >3 drinks/day, intravenous drug users, leukemia, lymphoma, head and neck cancer, lung cancer, chronic renal failure), recent immigrants from countries with high prevalence of TB, residents and employees of high-risk congregate settings (e.g., nursing homes, prisons), TB laboratory personnel; ≥15 mm considered positive in people with no risk factors for TB
interferon-gamma release assays
Test
Measure the response of T cells to TB antigens in order to diagnose prior exposure. Used for investigation for latent TB infection.
Interferon-gamma release assays, similar to tuberculin skin testing, have low sensitivity in diagnosing active TB, with a false-negative rate of 20% to 25% in patients with active pulmonary TB.[43] They do not distinguish between latent infection and active disease, which limits their usefulness in the diagnosis of active TB. Sensitivity of QuantiFERON®-TB Gold for active TB is 75%.[54][55]
Result
positive
TB antigen-based skin tests (TBSTs)
Test
TBSTs are a new class of tests that have been developed to measure the cell-mediated immunologic response to M tuberculosis specific antigens. The WHO recommends that TBSTs may be used to test for latent TB infection, reporting that the diagnostic accuracy of TBSTs is similar to that of interferon gamma release assays and greater than that of the TST.[48]
Result
positive
Use of this content is subject to our disclaimer