Tests
1st tests to order
ECG
Test
A 12-lead ECG should be performed and interpreted within 10 minutes of the patient's arrival in the emergency facility.[56] Classic ECG findings of ischemia in NSTEMI include horizontal or downsloping ST depression >1.0 mm and/or symmetrically inverted T waves (Wellens waves).[Figure caption and citation for the preceding image starts]: ECG showing ST depressionFrom the personal collection of Dr Syed W. Yusuf and Dr Iyad N. Daher, Department of Cardiology, University of Texas, Houston; used with permission [Citation ends].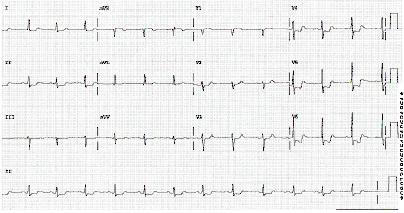 [Figure caption and citation for the preceding image starts]: ECG showing ST depressionFrom the personal collection of Dr Syed W. Yusuf and Dr Iyad N. Daher, Department of Cardiology, University of Texas, Houston; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: ECG showing ST depressionFrom the personal collection of Dr Syed W. Yusuf and Dr Iyad N. Daher, Department of Cardiology, University of Texas, Houston; used with permission [Citation ends].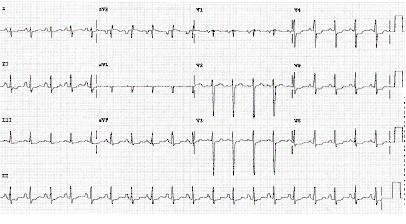
In many patients the ECG may be normal and in some patients there may be transient ST elevation.
Serial ECGs, initially at 15- to 30-minute intervals, then per provider discretion, should be taken in patients with chest pain, to detect development of ST-elevation myocardial infarction (MI), or to help guide reperfusion strategies.[2]
Continuous 12-lead ECG monitoring is a reasonable alternative to serial 12-lead recordings in patients whose initial ECG is nondiagnostic.[2]
Supplemental ECG leads V7 through V9 may be useful in patients with nondiagnostic initial ECGs to rule out MI due to left circumflex occlusion, and V3R and V4R may be useful to detect right ventricular MI.[5]
Result
nonspecific ST-T wave changes or ischemic changes
cardiac biomarkers
Test
Troponin levels confirm the diagnosis of infarction.[56] Test is the best marker for musculoskeletal injury, small myocardial infarction (MI), or late (>2-3 days) MI.
The 99th percentile is the cutoff value used to determine acute MI.
The 0 hour/1 hour algorithm (where a high-sensitive cardiac troponin measurement is made at presentation [0 hours] and at 1 hour after presentation) is recommended, or the 0 hour/2 hour algorithm may be used as a second-best option when using high-sensitivity assays. As an alternative, the 0 hour/ 3 hour algorithm may be considered. Additional testing after 3 hours is recommended if the first two cardiac troponin measurements of the 0 hour/1 hour algorithm are not conclusive and the clinical condition is still suggestive of ACS.[5] This test is readily available at most institutions. Cardiac troponins are more sensitive and specific markers of cardiomyocyte damage than creatine kinase (CK), its myocardial band isoenzyme (CK-MB), and myoglobin. In patients with MI, troponin levels rise rapidly (usually within 1 hour from symptom onset if using high-sensitivity assays) and remain elevated for several days. Therefore, with the advent of high-sensitive troponin assays (hs-cTn), other biomarkers (e.g., CK, CK-MB, and myoglobin) are no longer needed for diagnostic purposes. Similarly, for initial diagnostic purposes, routine measurement of additional biomarkers (e.g., heart-type fatty acid-binding protein [h-FABP] or copeptin) is not recommended in addition to hs-cTn.[5]
Other conditions that may cause elevated cardiac biomarkers include trauma, renal failure, congestive heart failure, surgery, inflammatory states, pulmonary embolism, sepsis, burns, rhabdomyolysis, and drug toxicity.[71]
Result
>99th percentile of normal
echocardiography
Test
Cardiac ultrasound may be useful for early triage of patients with suspected myocardial infarction.[4] An urgent echocardiogram should always be performed in hemodynamically unstable patients.[5][58] It can also be performed initially when a strong clinical suspicion of acute coronary syndrome is present and ECG is normal or inconclusive, to evaluate ischemic complications and other causes of chest pain (i.e., pulmonary embolism, pericardial effusion/tamponade, or acute valvular pathology).[4]
Result
regional wall motion abnormality, depressed left ventricular function, or decreased ejection fraction
CBC
Test
Hemoglobin and hematocrit measurements may help to evaluate a secondary cause of NSTEMI (e.g., acute blood loss, anemia) and to evaluate thrombocytopenia to estimate risk of bleeding.
Result
normal, anemia, thrombocytopenia
BUN and serum creatinine
electrolytes
Test
Electrolyte derangements may predispose to cardiac arrhythmias.
Result
normal or deranged
LFTs
Test
Useful if considering treatment with drugs that undergo hepatic metabolism.
Impaired LFTs may also suggest hepatic congestion in patients with concomitant heart failure.
Result
normal
blood glucose
Tests to consider
lipids
Test
Lipid management should include assessment of a fasting lipid profile for all patients, within 24 hours of admission to the hospital. Frequently, in the acute phase of an acute coronary syndrome, lipid values may be lower than normal for that patient.
Result
elevated, normal, or optimal
brain natriuretic peptide (BNP) or N-terminal pro-BNP (NT-pro-BNP)
Test
Measurement of BNP or NT-pro-BNP may be considered to supplement assessment of global risk in patients with suspected acute coronary syndrome.[2]
Result
>99th percentile of normal
angiography/cardiac catheterization
Test
Urgent and immediate angiography (without noninvasive risk stratification) with intensive medical treatment is warranted.[2][64][Figure caption and citation for the preceding image starts]: 64-slice CT angiography of a patient with stable angina showing 3D reconstruction (A), curved reformatted images (B) and confirmation of a high-grade lesion on conventional angiography (C). The arrowheads show calcified plaques. Dx= diagnosisFrom: Schussler JM and Grayburn PA. Heart. 2007 Mar;93(3):290-7 [Citation ends].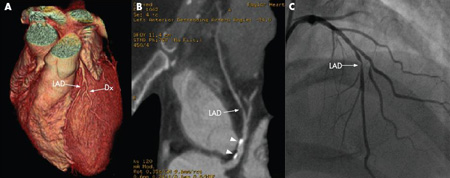 [Figure caption and citation for the preceding image starts]: 64-slice CT angiography (A) and conventional angiography (B) showing a high-grade lesion in the mid-right coronary artery, indicated by the arrows. The arrowheads show artifacts that may be mistaken for lesionsFrom: Schussler JM and Grayburn PA. Heart. 2007 Mar;93(3):290-7 [Citation ends].
[Figure caption and citation for the preceding image starts]: 64-slice CT angiography (A) and conventional angiography (B) showing a high-grade lesion in the mid-right coronary artery, indicated by the arrows. The arrowheads show artifacts that may be mistaken for lesionsFrom: Schussler JM and Grayburn PA. Heart. 2007 Mar;93(3):290-7 [Citation ends].
Indications include recurrent symptoms (refractory angina), ischemia despite adequate medical treatment, high risk (e.g., congestive heart failure, malignant ventricular arrhythmias), or noninvasive test findings (significant left ventricular dysfunction, ejection fraction <0.35, large anterior or multiple perfusion defects).[2]
Renal failure is a relative contraindication and patients with contrast allergy must be premedicated prior to angiography.
Result
severe stenosis or thrombosis
stress testing
Test
Stress testing, including treadmill exercise testing, may be useful and is recommended in patients with low and intermediate pretest probability with a normal ECG and normal high sensitivity biomarkers to assist with assessing need for an invasive strategy.[2][65][66]
The sensitivity and specificity of these tests increase when combined with either nuclear imaging to look for myocardial perfusion defects or echocardiography to assess wall motion abnormalities.
The key positive finding on nuclear imaging stress tests is the presence of a reversible defect. This is an area of myocardium that becomes deprived of perfusion during increased myocardial demand and reperfuses on stopping the activity. This signifies stenosis within the coronary circulation that may be treated with percutaneous coronary intervention or coronary artery bypass graft.
Submaximal exercise testing can be performed at 4-7 days after myocardial infarction, while symptom limited testing can be performed at 14-21 days post-myocardial infarction, when the patient has been free of active ischemic or heart failure symptoms.[67]
Result
ECG: ST-segment depression >1mm (0.1 mV); nuclear imaging: reversible or fixed perfusion defect
coronary CT angiography (CCTA)
Test
May provide noninvasive evaluation of coronary anatomy and atherosclerosis. Renal failure is a relative contraindication. Patients with a contrast allergy should be premedicated prior to angiography.[68][Figure caption and citation for the preceding image starts]: 64-slice CT angiography (A) and conventional angiography (B) showing a high-grade lesion in the mid-right coronary artery, indicated by the arrows. The arrowheads show artifacts that may be mistaken for lesionsFrom: Schussler JM and Grayburn PA. Heart. 2007 Mar;93(3):290-7 [Citation ends]. [Figure caption and citation for the preceding image starts]: 64-slice CT angiography of a patient with stable angina showing 3D reconstruction (A), curved reformatted images (B) and confirmation of a high-grade lesion on conventional angiography (C). The arrowheads show calcified plaques. Dx= diagnosisFrom: Schussler JM and Grayburn PA. Heart. 2007 Mar;93(3):290-7 [Citation ends].
[Figure caption and citation for the preceding image starts]: 64-slice CT angiography of a patient with stable angina showing 3D reconstruction (A), curved reformatted images (B) and confirmation of a high-grade lesion on conventional angiography (C). The arrowheads show calcified plaques. Dx= diagnosisFrom: Schussler JM and Grayburn PA. Heart. 2007 Mar;93(3):290-7 [Citation ends].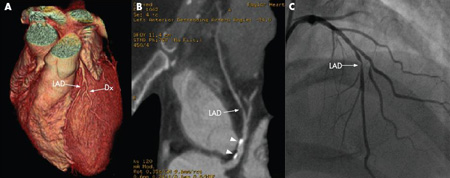
Due to the high negative predictive value of CCTA, evidence suggests that CCTA is useful in patients with low to moderate risk of NSTEMI. When compared with the standard care of low-risk patients (observation, serial enzymes followed by stress testing) CCTA reduced time to diagnosis, reduced length of emergency department stay, and had similar safety.[69] CCTA is not indicated for patients with high-risk features (i.e., ischemic ECG changes, positive cardiac markers).[70]
Result
occlusion or near-occlusion
Use of this content is subject to our disclaimer