Patients with suspected acute coronary syndrome (ACS) require urgent evaluation. It is essential to establish whether the symptoms are a manifestation of an ACS and, if so, how likely it is for an adverse clinical event to occur.[2]Amsterdam EA, Wenger NK, Brindis RG, et al. 2014 AHA/ACC guideline for the management of patients with non-ST-elevation acute coronary syndromes: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2014 Dec 23;64(24):e139-228.
http://www.onlinejacc.org/content/64/24/e139
http://www.ncbi.nlm.nih.gov/pubmed/25260718?tool=bestpractice.com
Physicians need to first establish the patient's risk and follow current guidelines according to the initial risk assessment to choose an appropriate management strategy. The initial risk assessment includes the history, examination, ECG, and cardiac biomarkers.[2]Amsterdam EA, Wenger NK, Brindis RG, et al. 2014 AHA/ACC guideline for the management of patients with non-ST-elevation acute coronary syndromes: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2014 Dec 23;64(24):e139-228.
http://www.onlinejacc.org/content/64/24/e139
http://www.ncbi.nlm.nih.gov/pubmed/25260718?tool=bestpractice.com
[5]Collet JP, Thiele H, Barbato E, et al. 2020 ESC guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation. Eur Heart J. 2021 Apr 7;42(14):1289-367.
https://academic.oup.com/eurheartj/article/42/14/1289/5898842
http://www.ncbi.nlm.nih.gov/pubmed/32860058?tool=bestpractice.com
[55]National Institute for Health and Care Excellence. Recent-onset chest pain of suspected cardiac origin: assessment and diagnosis. November 2016 [internet publication].
https://www.nice.org.uk/guidance/CG95
ECG
ECG is indicated as the first-line investigation in all patients. A 12-lead ECG should be performed and interpreted within 10 minutes of the patient arriving at the emergency facility.[56]Writing Committee, Kontos MC, de Lemos JA, et al. 2022 ACC Expert Consensus Decision Pathway on the evaluation and disposition of acute chest pain in the emergency department: A report of the American College of Cardiology Solution Set Oversight Committee. J Am Coll Cardiol. 2022 Nov 15;80(20):1925-60.
https://www.sciencedirect.com/science/article/pii/S0735109722066189?via%3Dihub
http://www.ncbi.nlm.nih.gov/pubmed/36241466?tool=bestpractice.com
It is critical to immediate management to exclude ST-elevation myocardial infarction (STEMI). NSTEMI is indistinguishable from other types of ACS (STEMI or unstable angina) until ECG and biomarkers become available, because their pathophysiology and presentation are similar.[2]Amsterdam EA, Wenger NK, Brindis RG, et al. 2014 AHA/ACC guideline for the management of patients with non-ST-elevation acute coronary syndromes: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2014 Dec 23;64(24):e139-228.
http://www.onlinejacc.org/content/64/24/e139
http://www.ncbi.nlm.nih.gov/pubmed/25260718?tool=bestpractice.com
Typical ECG findings may be present, but many patients have a normal ECG at presentation and therefore serial ECGs, initially at 15- to 30-minute intervals, should be performed to detect the potential for development of ST-segment elevation or depression. Where present, ECG findings in NSTEMI may be highly variable. Typically >1 mm of ST depression is present in 2 or more contiguous leads. Other potential findings include dramatic new T-wave inversions (Wellens waves) or transient ST elevation. ECG changes of ST elevation or new left bundle branch block should be evaluated as STEMI.[Figure caption and citation for the preceding image starts]: ECG showing ST depressionFrom the personal collection of Dr Syed W. Yusuf and Dr Iyad N. Daher, Department of Cardiology, University of Texas, Houston; used with permission [Citation ends].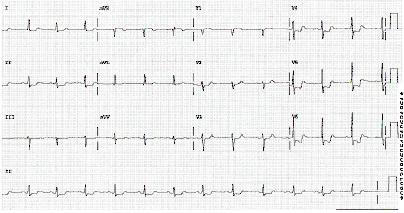 [Figure caption and citation for the preceding image starts]: ECG showing ST depressionFrom the personal collection of Dr Syed W. Yusuf and Dr Iyad N. Daher, Department of Cardiology, University of Texas, Houston; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: ECG showing ST depressionFrom the personal collection of Dr Syed W. Yusuf and Dr Iyad N. Daher, Department of Cardiology, University of Texas, Houston; used with permission [Citation ends].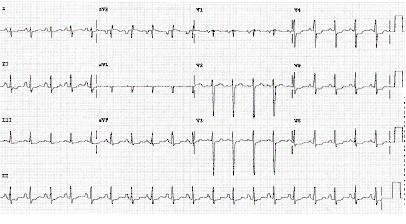
Continuous 12-lead ECG monitoring is a reasonable alternative to serial 12-lead recordings in patients whose initial ECG is nondiagnostic.[2]Amsterdam EA, Wenger NK, Brindis RG, et al. 2014 AHA/ACC guideline for the management of patients with non-ST-elevation acute coronary syndromes: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2014 Dec 23;64(24):e139-228.
http://www.onlinejacc.org/content/64/24/e139
http://www.ncbi.nlm.nih.gov/pubmed/25260718?tool=bestpractice.com
Supplemental ECG leads V7 through V9 may be useful in patients with nondiagnostic initial ECGs to rule out myocardial infarction (MI) due to left circumflex occlusion, and V3R and V4R may be useful to detect right ventricular MI.[5]Collet JP, Thiele H, Barbato E, et al. 2020 ESC guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation. Eur Heart J. 2021 Apr 7;42(14):1289-367.
https://academic.oup.com/eurheartj/article/42/14/1289/5898842
http://www.ncbi.nlm.nih.gov/pubmed/32860058?tool=bestpractice.com
Less commonly, the ECG may reveal a tachyarrhythmia or bradyarrhythmia precipitated by the MI.
History and examination
Patients presenting with chest pain or discomfort need immediate assessment for current or past history of coronary artery disease (CAD) and traditional risk factors (e.g., age, sex, diabetes, hypertension, cocaine use) to triage them as high priority.[2]Amsterdam EA, Wenger NK, Brindis RG, et al. 2014 AHA/ACC guideline for the management of patients with non-ST-elevation acute coronary syndromes: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2014 Dec 23;64(24):e139-228.
http://www.onlinejacc.org/content/64/24/e139
http://www.ncbi.nlm.nih.gov/pubmed/25260718?tool=bestpractice.com
ACS is highly likely if there is a history of chest or left arm pain similar to previously documented angina pain, and a history of CAD (including MI). Angina pain is typically deep, poorly localized chest or arm pain described as a sensation of tightness, heaviness, aching, burning, pressure, or squeezing. The pain is most often retrosternal and can often radiate to the left arm, but may also radiate to the lower jaw, neck, both arms, back, and epigastrium, where it may mimic heartburn. It is associated with exertion or emotional stress (or less commonly with cold exposure) and relieved by rest.[2]Amsterdam EA, Wenger NK, Brindis RG, et al. 2014 AHA/ACC guideline for the management of patients with non-ST-elevation acute coronary syndromes: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2014 Dec 23;64(24):e139-228.
http://www.onlinejacc.org/content/64/24/e139
http://www.ncbi.nlm.nih.gov/pubmed/25260718?tool=bestpractice.com
[57]Writing Committee Members; Gulati M, Levy PD, Mukherjee D, et al. 2021 AHA/ACC/ASE/CHEST/SAEM/SCCT/SCMR guideline for the evaluation and diagnosis of chest pain: a report of the American College of Cardiology/American Heart Association Joint Committee On Clinical Practice Guidelines. J Am Coll Cardiol. 2021 Nov 30;78(22):e187-285.
https://www.sciencedirect.com/science/article/pii/S0735109721057958
http://www.ncbi.nlm.nih.gov/pubmed/34756653?tool=bestpractice.com
Diaphoresis is a common associated symptom. Shortness of breath is also common and is probably secondary to diminished cardiac output, but may also be due to underlying pulmonary congestion. Patients may express anxiety or appear anxious. They may also report a feeling of impending doom. Classically, events peak in the early morning hours, presumably due to hemodynamic stress caused by increased serum cortisol, adrenergic hormones, and platelet aggregation.
Patients may present with a range of nonclassic symptoms, any of which may be the sole presenting symptom. These include weakness, nausea, vomiting, abdominal pain, and syncope. These are more common in women, older people, and those with diabetes or chronic kidney disease. Examination findings are usually nonspecific but may reveal hypertension or hypotension, the presence of third and fourth heart sounds, and paradoxical splitting of the second heart sound. Signs of heart failure (raised jugular venous pressure, bilateral crepitations on auscultation of the lungs) or cardiogenic shock may also be present, and these signify a worse prognosis.
Relief of chest pain with sublingual nitroglycerin is not necessarily diagnostic of myocardial ischemia and should not be used as a diagnostic criterion; other entities (e.g., esophageal spasm) may demonstrate a comparable response.[57]Writing Committee Members; Gulati M, Levy PD, Mukherjee D, et al. 2021 AHA/ACC/ASE/CHEST/SAEM/SCCT/SCMR guideline for the evaluation and diagnosis of chest pain: a report of the American College of Cardiology/American Heart Association Joint Committee On Clinical Practice Guidelines. J Am Coll Cardiol. 2021 Nov 30;78(22):e187-285.
https://www.sciencedirect.com/science/article/pii/S0735109721057958
http://www.ncbi.nlm.nih.gov/pubmed/34756653?tool=bestpractice.com
Pain described as sharp, fleeting (few seconds duration), or related to inspiration (pleuritic) or position, or which is shifting in location, suggests a lower likelihood of ischemia.[57]Writing Committee Members; Gulati M, Levy PD, Mukherjee D, et al. 2021 AHA/ACC/ASE/CHEST/SAEM/SCCT/SCMR guideline for the evaluation and diagnosis of chest pain: a report of the American College of Cardiology/American Heart Association Joint Committee On Clinical Practice Guidelines. J Am Coll Cardiol. 2021 Nov 30;78(22):e187-285.
https://www.sciencedirect.com/science/article/pii/S0735109721057958
http://www.ncbi.nlm.nih.gov/pubmed/34756653?tool=bestpractice.com
Initial tests (non-ECG)
In addition to the ECG, the following tests must also be performed in all patients.
Cardiac troponins: a rise in the levels of cardiac troponins (>99th percentile of normal) are diagnostic for the condition and the use of high-sensitivity cardiac troponin assays have shortened the assessment time interval.[56]Writing Committee, Kontos MC, de Lemos JA, et al. 2022 ACC Expert Consensus Decision Pathway on the evaluation and disposition of acute chest pain in the emergency department: A report of the American College of Cardiology Solution Set Oversight Committee. J Am Coll Cardiol. 2022 Nov 15;80(20):1925-60.
https://www.sciencedirect.com/science/article/pii/S0735109722066189?via%3Dihub
http://www.ncbi.nlm.nih.gov/pubmed/36241466?tool=bestpractice.com
The 0 hour/1 hour algorithm (where a high-sensitive cardiac troponin measurement is made at presentation [0 hours] and at 1 hour after presentation) is recommended, or the 0 hour/2 hour algorithm may be used as a second-best option when using high-sensitivity assays. As an alternative, the 0 hour/ 3 hour algorithm may be considered. Additional testing after 3 hours is recommended if the first two cardiac troponin measurements of the 0 hour/1 hour algorithm are not conclusive and the clinical condition is still suggestive of ACS.[5]Collet JP, Thiele H, Barbato E, et al. 2020 ESC guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation. Eur Heart J. 2021 Apr 7;42(14):1289-367.
https://academic.oup.com/eurheartj/article/42/14/1289/5898842
http://www.ncbi.nlm.nih.gov/pubmed/32860058?tool=bestpractice.com
This test is readily available at most institutions. Cardiac troponins are more sensitive and specific markers of cardiomyocyte damage than creatine kinase (CK), its myocardial band isoenzyme (CK-MB), and myoglobin. In patients with MI, troponin levels rise rapidly (usually within 1 hour from symptom onset if using high-sensitivity assays) and remain elevated for several days. Therefore, with the advent of high-sensitive troponin assays (hs-cTn), other biomarkers (e.g., CK, CK-MB, and myoglobin) are no longer needed for diagnostic purposes. Similarly, for initial diagnostic purposes, routine measurement of additional biomarkers (e.g., heart-type fatty acid-binding protein [h-FABP] or copeptin) is not recommended in addition to hs-cTn.[5]Collet JP, Thiele H, Barbato E, et al. 2020 ESC guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation. Eur Heart J. 2021 Apr 7;42(14):1289-367.
https://academic.oup.com/eurheartj/article/42/14/1289/5898842
http://www.ncbi.nlm.nih.gov/pubmed/32860058?tool=bestpractice.com
Echocardiography: cardiac ultrasound may be useful for early triage of patients with suspected MI.[4]Thygesen K, Alpert JS, Jaffe AS, et al; Executive Group on behalf of the Joint European Society of Cardiology (ESC)/American College of Cardiology (ACC)/American Heart Association (AHA)/World Heart Federation (WHF) Task Force for the Universal Definition of Myocardial Infarction. Fourth universal definition of myocardial infarction (2018). J Am Coll Cardiol. 2018 Oct 30;72(18):2231-64.
http://www.onlinejacc.org/content/early/2018/08/27/j.jacc.2018.08.1038
http://www.ncbi.nlm.nih.gov/pubmed/30153967?tool=bestpractice.com
An urgent echocardiogram should always be performed in hemodynamically unstable patients.[5]Collet JP, Thiele H, Barbato E, et al. 2020 ESC guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation. Eur Heart J. 2021 Apr 7;42(14):1289-367.
https://academic.oup.com/eurheartj/article/42/14/1289/5898842
http://www.ncbi.nlm.nih.gov/pubmed/32860058?tool=bestpractice.com
[58]Edvardsen T, Asch FM, Davidson B, et al. Non-invasive imaging in coronary syndromes: recommendations of the European Association of Cardiovascular Imaging and the American Society of Echocardiography, in collaboration with the American Society of Nuclear Cardiology, Society of Cardiovascular Computed Tomography, and Society for Cardiovascular Magnetic Resonance. Eur Heart J Cardiovasc Imaging. 2022 Jan 24;23(2):e6-33.
https://academic.oup.com/ehjcimaging/article/23/2/e6/6423983
http://www.ncbi.nlm.nih.gov/pubmed/34751391?tool=bestpractice.com
It can also be performed initially when a strong clinical suspicion of acute coronary syndrome is present and ECG is normal or inconclusive, to evaluate ischemic complications and other causes of chest pain (i.e., pulmonary embolism, pericardial effusion/tamponade, or acute valvular pathology).[4]Thygesen K, Alpert JS, Jaffe AS, et al; Executive Group on behalf of the Joint European Society of Cardiology (ESC)/American College of Cardiology (ACC)/American Heart Association (AHA)/World Heart Federation (WHF) Task Force for the Universal Definition of Myocardial Infarction. Fourth universal definition of myocardial infarction (2018). J Am Coll Cardiol. 2018 Oct 30;72(18):2231-64.
http://www.onlinejacc.org/content/early/2018/08/27/j.jacc.2018.08.1038
http://www.ncbi.nlm.nih.gov/pubmed/30153967?tool=bestpractice.com
Patients with a high index of suspicion who have negative serial ECGs and cardiac enzymes should be closely monitored in a telemetry or chest pain unit, as it may take time for cardiac markers to rise.[2]Amsterdam EA, Wenger NK, Brindis RG, et al. 2014 AHA/ACC guideline for the management of patients with non-ST-elevation acute coronary syndromes: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2014 Dec 23;64(24):e139-228.
http://www.onlinejacc.org/content/64/24/e139
http://www.ncbi.nlm.nih.gov/pubmed/25260718?tool=bestpractice.com
Chest x-ray: indicated to determine whether congestive heart failure (CHF) is present and to exclude noncardiac causes for chest pain.[56]Writing Committee, Kontos MC, de Lemos JA, et al. 2022 ACC Expert Consensus Decision Pathway on the evaluation and disposition of acute chest pain in the emergency department: A report of the American College of Cardiology Solution Set Oversight Committee. J Am Coll Cardiol. 2022 Nov 15;80(20):1925-60.
https://www.sciencedirect.com/science/article/pii/S0735109722066189?via%3Dihub
http://www.ncbi.nlm.nih.gov/pubmed/36241466?tool=bestpractice.com
CBC: hemoglobin and hematocrit measurements may help to evaluate a secondary cause of NSTEMI (e.g., acute blood loss, anemia) and to evaluate thrombocytopenia to estimate risk of bleeding.
BUN and serum creatinine: creatinine clearance should be estimated in NSTEMI patients and the doses of renally cleared drugs should be adjusted appropriately. In chronic kidney disease patients undergoing angiography, iso-osmolar contrast agents may be preferred.[2]Amsterdam EA, Wenger NK, Brindis RG, et al. 2014 AHA/ACC guideline for the management of patients with non-ST-elevation acute coronary syndromes: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2014 Dec 23;64(24):e139-228.
http://www.onlinejacc.org/content/64/24/e139
http://www.ncbi.nlm.nih.gov/pubmed/25260718?tool=bestpractice.com
[59]Neumann FJ, Sousa-Uva M, Ahlsson A, et al; ESC Scientific Document Group. 2018 ESC/EACTS guidelines on myocardial revascularization. Eur Heart J. 2019 Jan 7;40(2):87-165.
https://academic.oup.com/eurheartj/advance-article/doi/10.1093/eurheartj/ehy394/5079120
http://www.ncbi.nlm.nih.gov/pubmed/30165437?tool=bestpractice.com
Serum electrolytes: electrolyte derangements may predispose to cardiac arrhythmias.
Liver function tests: useful if treatment with drugs that undergo hepatic metabolism is considered. Impaired liver function tests may also suggest hepatic congestion in patients with concomitant heart failure.
Blood glucose levels: hyperglycemia is common in the setting of acute MI, with or without a history of diabetes.[60]Gholap NN, Mehta RL, Ng L, et al. Is admission blood glucose concentration a more powerful predictor of mortality after myocardial infarction than diabetes diagnosis? A retrospective cohort study. BMJ Open. 2012 Sep 25;2(5):e001596.
https://bmjopen.bmj.com/content/2/5/e001596.long
http://www.ncbi.nlm.nih.gov/pubmed/23015602?tool=bestpractice.com
There is controversy over whether tight glucose control may reduce risk of death and morbidity.[61]de Mulder M, Umans VA, Cornel JH, et al. Intensive glucose regulation in hyperglycemic acute coronary syndrome: results of the randomized BIOMarker study to identify the acute risk of a coronary syndrome-2 (BIOMArCS-2) glucose trial. JAMA Intern Med. 2013 Nov 11;173(20):1896-904.
https://jamanetwork.com/journals/jamainternalmedicine/fullarticle/1735896
http://www.ncbi.nlm.nih.gov/pubmed/24018647?tool=bestpractice.com
Risk stratification
ACS management requires continuous risk stratification for death or recurrent MI. The American College of Cardiology/American Heart Association recommend that patients with suspected ACS are risk stratified based on the likelihood of ACS and adverse outcome(s) to further triage and assist in the selection of treatment options, particularly in settings where high-sensitivity cardiac troponin assays are not available.[2]Amsterdam EA, Wenger NK, Brindis RG, et al. 2014 AHA/ACC guideline for the management of patients with non-ST-elevation acute coronary syndromes: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2014 Dec 23;64(24):e139-228.
http://www.onlinejacc.org/content/64/24/e139
http://www.ncbi.nlm.nih.gov/pubmed/25260718?tool=bestpractice.com
[57]Writing Committee Members; Gulati M, Levy PD, Mukherjee D, et al. 2021 AHA/ACC/ASE/CHEST/SAEM/SCCT/SCMR guideline for the evaluation and diagnosis of chest pain: a report of the American College of Cardiology/American Heart Association Joint Committee On Clinical Practice Guidelines. J Am Coll Cardiol. 2021 Nov 30;78(22):e187-285.
https://www.sciencedirect.com/science/article/pii/S0735109721057958
http://www.ncbi.nlm.nih.gov/pubmed/34756653?tool=bestpractice.com
Several risk scores exist that incorporate a number of variables such as clinical history, angina symptoms and equivalents, physical exam, ECG, renal function, and troponin levels. These variables can be used to estimate the risk of death and nonfatal cardiac ischemic events: for example, using the TIMI risk score or the Global Registry of Acute Coronary Events (GRACE) risk model.[2]Amsterdam EA, Wenger NK, Brindis RG, et al. 2014 AHA/ACC guideline for the management of patients with non-ST-elevation acute coronary syndromes: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2014 Dec 23;64(24):e139-228.
http://www.onlinejacc.org/content/64/24/e139
http://www.ncbi.nlm.nih.gov/pubmed/25260718?tool=bestpractice.com
[62]Antman EM, Cohen M, Bernink PJ, et al. The TIMI risk score for unstable angina/non-ST elevation MI: a method for prognostication and therapeutic decision making. JAMA. 2000 Aug 16;284(7):835-42.
https://jamanetwork.com/journals/jama/fullarticle/192996
http://www.ncbi.nlm.nih.gov/pubmed/10938172?tool=bestpractice.com
[
Thrombolysis in Myocardial Infarction (TIMI) Score for Unstable Angina Non ST Elevation Myocardial Infarction
Opens in new window
]
[
GRACE Score for Acute Coronary Syndrome Prognosis
Opens in new window
]
The TIMI risk score is composed of 7 risk indicators rated on presentation. One point is awarded for the presence of each of the following criteria:
Age >65 years
Presence of ≥3 CAD risk factors
Prior coronary stenosis >50%
ST-segment deviation on ECG
Elevated serum cardiac biomarkers
At least 2 anginal episodes in the past 24 hours
Use of aspirin in the past 7 days.
Patients with a TIMI score of 0 to 2 are low risk, 3 to 4 are intermediate risk, and 5 to 7 are high risk. All-cause mortality, rate of MI, and rate of urgent revascularization at 14 days increase in proportion to the number of risk factors present on the TIMI score.
The GRACE risk model is a web-based tool that can be used to predict in-hospital and post-discharge mortality or MI in patients following an initial ACS.
The Killip classification is another tool that can be used for risk stratification. This classification system risk stratifies patients with acute MI based on clinical evidence of left ventricular failure:
Class I: no evidence of CHF
Class II: presence of a third heart sound gallop, basilar rales, or elevated jugular venous pressure
Class III: presence of pulmonary edema
Class IV: cardiogenic shock.
The HEART Score incorporates elements of the patient’s history, ECG, age, risk factors, and troponin and is used for patients in the emergency room setting to assess risk of acute MI, percutaneous coronary intervention, coronary artery bypass graft (CABG), and death within 6 weeks of initial presentation.[63]Backus BE, Six AJ, Kelder JC, et al. A prospective validation of the HEART score for chest pain patients at the emergency department. Int J Cardiol. 2013 Oct 3;168(3):2153-8.
https://www.internationaljournalofcardiology.com/article/S0167-5273(13)00315-X/fulltext
http://www.ncbi.nlm.nih.gov/pubmed/23465250?tool=bestpractice.com
[
HEART Score
Opens in new window
]
Subsequent tests
Following initial workup and risk stratification, a range of additional investigations may be considered.
Brain natriuretic peptide (BNP) and N-terminal pro-BNP (NT-pro-BNP): measurement of BNP or NT-pro-BNP may be considered to supplement assessment of global risk in patients with suspected ACS, particularly cardiogenic shock associated with MI type 1.[2]Amsterdam EA, Wenger NK, Brindis RG, et al. 2014 AHA/ACC guideline for the management of patients with non-ST-elevation acute coronary syndromes: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2014 Dec 23;64(24):e139-228.
http://www.onlinejacc.org/content/64/24/e139
http://www.ncbi.nlm.nih.gov/pubmed/25260718?tool=bestpractice.com
[5]Collet JP, Thiele H, Barbato E, et al. 2020 ESC guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation. Eur Heart J. 2021 Apr 7;42(14):1289-367.
https://academic.oup.com/eurheartj/article/42/14/1289/5898842
http://www.ncbi.nlm.nih.gov/pubmed/32860058?tool=bestpractice.com
Lipid profile: this test is indicated in the first 24 hours of admission to the hospital to assess for lipid abnormalities and therefore the need for any lipid-lowering therapy.
Angiography: urgent and immediate angiography is indicated if patients do not stabilize with intensive medical treatment.[2]Amsterdam EA, Wenger NK, Brindis RG, et al. 2014 AHA/ACC guideline for the management of patients with non-ST-elevation acute coronary syndromes: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2014 Dec 23;64(24):e139-228.
http://www.onlinejacc.org/content/64/24/e139
http://www.ncbi.nlm.nih.gov/pubmed/25260718?tool=bestpractice.com
[64]Lawton JS, Tamis-Holland JE, Bangalore S, et al. 2021 ACC/AHA/SCAI guideline for coronary artery revascularization: a report of the American College of Cardiology/American Heart Association Joint Committee On Clinical Practice Guidelines. Circulation. 2022 Jan 18;145(3):e18-114.
https://www.ahajournals.org/doi/full/10.1161/CIR.0000000000001038
http://www.ncbi.nlm.nih.gov/pubmed/34882435?tool=bestpractice.com
Indications include recurrent symptoms (refractory angina), ischemia despite adequate medical treatment, high risk (e.g., CHF, malignant ventricular arrhythmias), or noninvasive test findings (significant left ventricular dysfunction, ejection fraction <0.35, large anterior or multiple perfusion defects). Patients with a history of anaphylaxis or allergy to contrast must be premedicated prior to angiography.[Figure caption and citation for the preceding image starts]: 64-slice CT angiography (A) and conventional angiography (B) showing a high-grade lesion in the mid-right coronary artery, indicated by the arrows. The arrowheads show artifacts that may be mistaken for lesionsFrom: Schussler JM and Grayburn PA. Heart. 2007 Mar;93(3):290-7 [Citation ends]. [Figure caption and citation for the preceding image starts]: 64-slice CT angiography of a patient with stable angina showing 3D reconstruction (A), curved reformatted images (B) and confirmation of a high-grade lesion on conventional angiography (C). The arrowheads show calcified plaques. Dx= diagnosisFrom: Schussler JM and Grayburn PA. Heart. 2007 Mar;93(3):290-7 [Citation ends].
[Figure caption and citation for the preceding image starts]: 64-slice CT angiography of a patient with stable angina showing 3D reconstruction (A), curved reformatted images (B) and confirmation of a high-grade lesion on conventional angiography (C). The arrowheads show calcified plaques. Dx= diagnosisFrom: Schussler JM and Grayburn PA. Heart. 2007 Mar;93(3):290-7 [Citation ends].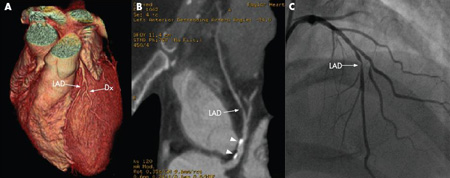
Stress testing: stress testing, including treadmill exercise testing, may be useful and is recommended in low and intermediate pretest probability with a normal ECG and normal high sensitivity biomarkers to assist with guiding the need for an invasive strategy.[2]Amsterdam EA, Wenger NK, Brindis RG, et al. 2014 AHA/ACC guideline for the management of patients with non-ST-elevation acute coronary syndromes: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2014 Dec 23;64(24):e139-228.
http://www.onlinejacc.org/content/64/24/e139
http://www.ncbi.nlm.nih.gov/pubmed/25260718?tool=bestpractice.com
[65]Lindahl B, Andrén B, Ohlsson J, et al. Risk stratification in unstable coronary artery disease. Additive value of troponin T determinations and pre-discharge exercise tests. Eur Heart J. 1997 May;18(5):762-70.
http://www.ncbi.nlm.nih.gov/pubmed/9152646?tool=bestpractice.com
[66]Nyman I, Larsson H, Areskog M, et al. The predictive value of silent ischemia at an exercise test before discharge after an episode of unstable coronary artery disease. Am Heart J. 1992 Feb;123(2):324-31.
http://www.ncbi.nlm.nih.gov/pubmed/1736566?tool=bestpractice.com
The sensitivity and specificity of these tests increase when combined with either nuclear imaging to look for myocardial perfusion defects or echocardiography to assess wall motion abnormalities. The key positive finding on nuclear imaging stress tests is the presence of a reversible defect. This is an area of myocardium that becomes deprived of perfusion during increased myocardial demand and reperfuses on stopping the activity. This signifies stenosis within the coronary circulation that may be treated with percutaneous coronary intervention or CABG. Submaximal exercise testing can be performed at 4 to 7 days after myocardial infarction, while symptom limited testing can be performed at 14 to 21 days post-myocardial infarction, when the patient has been free of active ischemic or heart failure symptoms.[67]Fletcher GF, Ades PA, Kligfield P, et al. Exercise standards for testing and training: a scientific statement from the American Heart Association. Circulation. 2013 Aug 20;128(8):873-934.
https://www.ahajournals.org/doi/full/10.1161/cir.0b013e31829b5b44
http://www.ncbi.nlm.nih.gov/pubmed/23877260?tool=bestpractice.com
Coronary CT angiography (CCTA): this may provide noninvasive evaluation of coronary anatomy and atherosclerosis. Renal failure is a relative contraindication. Patients with contrast allergy may be premedicated prior to angiography.[68]Raff GL, Gallagher MJ, O'Neill WW, et al. Diagnostic accuracy of noninvasive coronary angiography using 64-slice spiral computed tomography. J Am Coll Cardiol. 2005 Aug 2;46(3):552-7.
http://www.onlinejacc.org/content/46/3/552
http://www.ncbi.nlm.nih.gov/pubmed/16053973?tool=bestpractice.com
Due to the high negative predictive value of CCTA, evidence suggests that CCTA is useful in patients with low to moderate risk of NSTEMI. When compared with the standard care of low-risk patients (observation, serial enzymes followed by stress testing) CCTA reduced time to diagnosis, reduced length of emergency department stay, and had similar safety.[69]Hoffmann U, Truong QA, Schoenfeld DA, et al; ROMICAT-II Investigators. Coronary CT angiography versus standard evaluation in acute chest pain. N Engl J Med. 2012 Jul 26;367(4):299-308.
https://www.nejm.org/doi/10.1056/NEJMoa1201161
http://www.ncbi.nlm.nih.gov/pubmed/22830462?tool=bestpractice.com
CCTA is not indicated for patients with high-risk features (i.e., ischemic ECG changes, positive cardiac markers).[70]Hendel RC, Patel MR, Kramer CM, et al; American College of Cardiology Foundation Quality Strategic Directions Committee Appropriateness Criteria Working Group; American College of Radiology; Society of Cardiovascular Computed Tomography; Society for Cardiovascular Magnetic Resonance; American Society of Nuclear Cardiology; North American Society for Cardiac Imaging; Society for Cardiovascular Angiography and Interventions; Society of Interventional Radiology. ACCF/ACR/SCCT/SCMR/ASNC/NASCI/SCAI/SIR 2006 appropriateness criteria for cardiac computed tomography and cardiac magnetic resonance imaging. J Am Coll Cardiol. 2006 Oct 3;48(7):1475-97.
http://www.onlinejacc.org/content/48/7/1475
http://www.ncbi.nlm.nih.gov/pubmed/17010819?tool=bestpractice.com
[Figure caption and citation for the preceding image starts]: 64-slice CT angiography of a patient with stable angina showing 3D reconstruction (A), curved reformatted images (B) and confirmation of a high-grade lesion on conventional angiography (C). The arrowheads show calcified plaques. Dx= diagnosisFrom: Schussler JM and Grayburn PA. Heart. 2007 Mar;93(3):290-7 [Citation ends].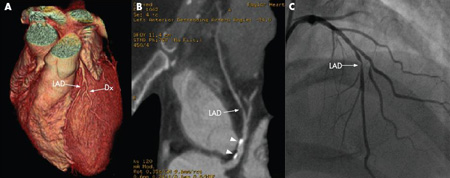 [Figure caption and citation for the preceding image starts]: 64-slice CT angiography (A) and conventional angiography (B) showing a high-grade lesion in the mid-right coronary artery, indicated by the arrows. The arrowheads show artifacts that may be mistaken for lesionsFrom: Schussler JM and Grayburn PA. Heart. 2007 Mar;93(3):290-7 [Citation ends].
[Figure caption and citation for the preceding image starts]: 64-slice CT angiography (A) and conventional angiography (B) showing a high-grade lesion in the mid-right coronary artery, indicated by the arrows. The arrowheads show artifacts that may be mistaken for lesionsFrom: Schussler JM and Grayburn PA. Heart. 2007 Mar;93(3):290-7 [Citation ends].
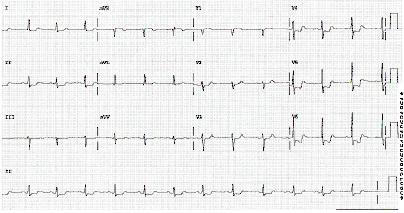 [Figure caption and citation for the preceding image starts]: ECG showing ST depressionFrom the personal collection of Dr Syed W. Yusuf and Dr Iyad N. Daher, Department of Cardiology, University of Texas, Houston; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: ECG showing ST depressionFrom the personal collection of Dr Syed W. Yusuf and Dr Iyad N. Daher, Department of Cardiology, University of Texas, Houston; used with permission [Citation ends].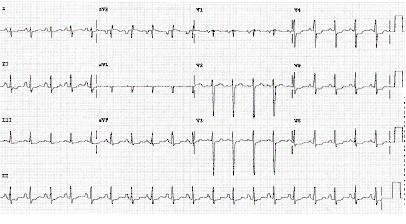
 [Figure caption and citation for the preceding image starts]: 64-slice CT angiography of a patient with stable angina showing 3D reconstruction (A), curved reformatted images (B) and confirmation of a high-grade lesion on conventional angiography (C). The arrowheads show calcified plaques. Dx= diagnosisFrom: Schussler JM and Grayburn PA. Heart. 2007 Mar;93(3):290-7 [Citation ends].
[Figure caption and citation for the preceding image starts]: 64-slice CT angiography of a patient with stable angina showing 3D reconstruction (A), curved reformatted images (B) and confirmation of a high-grade lesion on conventional angiography (C). The arrowheads show calcified plaques. Dx= diagnosisFrom: Schussler JM and Grayburn PA. Heart. 2007 Mar;93(3):290-7 [Citation ends].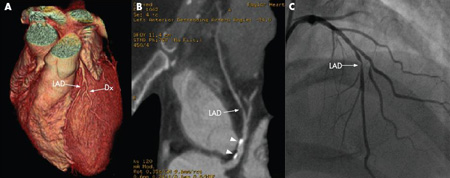
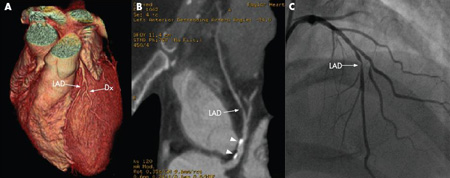 [Figure caption and citation for the preceding image starts]: 64-slice CT angiography (A) and conventional angiography (B) showing a high-grade lesion in the mid-right coronary artery, indicated by the arrows. The arrowheads show artifacts that may be mistaken for lesionsFrom: Schussler JM and Grayburn PA. Heart. 2007 Mar;93(3):290-7 [Citation ends].
[Figure caption and citation for the preceding image starts]: 64-slice CT angiography (A) and conventional angiography (B) showing a high-grade lesion in the mid-right coronary artery, indicated by the arrows. The arrowheads show artifacts that may be mistaken for lesionsFrom: Schussler JM and Grayburn PA. Heart. 2007 Mar;93(3):290-7 [Citation ends].