Tests
1st tests to order
ECG
Test
Should be obtained and interpreted by a qualified physician within the first 10 minutes after a patient presents with chest pain.[1][77][81][Figure caption and citation for the preceding image starts]: ECG showing ST depressionFrom the personal collection of Dr Syed Wamique Yusuf [Citation ends]. [Figure caption and citation for the preceding image starts]: ECG showing ST depressionFrom the personal collection of Dr Syed Wamique Yusuf [Citation ends].
[Figure caption and citation for the preceding image starts]: ECG showing ST depressionFrom the personal collection of Dr Syed Wamique Yusuf [Citation ends].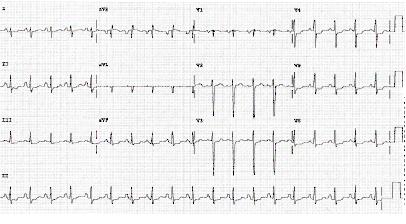
Additional ECG leads (V3R, V4R, V7-V9) are recommended if ongoing ischemia is suspected when standard leads are inconclusive.[1]
In patients with recurrent symptoms or in case of diagnostic uncertainty, additional 12-lead ECG should be obtained.[1]
If the initial ECG is not diagnostic but the patient remains symptomatic and there is a high clinical suspicion for acute coronary syndrome (ACS), serial ECGs should be performed to detect ischemic changes.[2][77]
The timing for repeat ECGs should be guided by symptoms, especially if chest pain recurs or a change in clinical condition develops.[77] In clinical practice a repeat ECG is usually performed at 6 and 24 hours (more frequently if clinical status changes).
Result
may be normal or have ST-segment depression, T-wave inversion, or transient ST-segment elevation
cardiac biomarkers
Test
High-sensitivity cardiac troponin assays allow rapid exclusion of myocardial necrosis.[1][77][81] The 0 hour/1 hour algorithm (where a high-sensitivity cardiac troponin measurement is made at presentation [0 hours] and at 1 hour after presentation) is recommended to rule out non-ST-elevation acute coronary syndromes (NSTE-ACS) when using high-sensitivity assays, or the 0 hour/2 hour algorithm may be used as a second-best option. Additional testing after 3 hours is recommended if the first two cardiac troponin measurements of the 0 hour/1 hour algorithm are not conclusive and the clinical condition is still suggestive of acute coronary syndrome.[1] In clinical practice, diagnostic algorithms for NSTE-ACS should be used in conjunction with all available clinical information and ECG. Additional serial cardiac troponin testing should be pursued if clinical suspicion remains high, or whenever the patient develops recurrent chest pain.[1][77]
When a previous-generation troponin assay is used, cardiac-specific troponin (troponin I or T) levels should be measured at presentation and 3 to 6 hours after symptom onset in all patients who present with symptoms consistent with acute coronary syndromes.[2] Additional troponin levels should be obtained beyond 6 hours after symptom onset in patients with normal troponins on serial examination when, based on clinical presentation and/or ECG changes, there is an intermediate or high index of suspicion for acute coronary syndrome.[2] In low-to-intermediate risk patients with suspected ACS, undetectable high-sensitivity troponin T values at admission are associated with very low risk of death or myocardial infarction (MI) within 90 days.[84]
Troponin remains elevated up to 10-14 days after release. Thus, in a patient who had an acute MI several days earlier presenting with chest discomfort, a single, slightly elevated troponin level may represent old ischemia.
In patients in whom a re-infarction is suspected, a troponin re-elevation of 20% or more has been advocated as a marker.[85]
Among patients presenting to the emergency department with chest pain, even slightly elevated blood levels of high-sensitivity cardiac troponin T are associated with adverse clinical outcomes, with a strong and graded association between all detectable levels of high-sensitivity cardiac troponin T and risk for myocardial infarction, heart failure, and cardiovascular and noncardiovascular mortality. The yearly rate of death was 0.5% among patients with high-sensitivity cardiac troponin T levels <0.005 micrograms/L, and this rate increased in a graded manner with increasing levels to 33% among patients with high-sensitivity cardiac troponin T levels ≥0.05 micrograms/L.[86]
Cardiac troponins are more sensitive and specific markers of cardiomyocyte damage than creatine kinase (CK), its myocardial band isoenzyme (CK-MB), and myoglobin. In patients with myocardial infarction, troponin levels rise rapidly (usually within 1 hour from symptom onset if using high-sensitivity assays) and remain elevated for several days. Hence, with the advent of high-sensitivity cardiac troponin assays (hs-cTn), do not use other biomarkers such as CK, CK-MB, and myoglobin in diagnosis.[1][2][77][87] If there is no evidence of myocardial injury or necrosis, the patient with history and ECG changes suggestive of non-ST-elevation MI (NSTEMI) is considered to have UA.[2]
Result
not elevated
CXR
Test
A CXR should be ordered to look for other causes of chest pain, such as a wide mediastinum in case of aortic dissection, hyperlucent lung field in pulmonary embolism, wedge-shaped infarct in pulmonary infarction, consolidation in pneumonia, collapsed lung in pneumothorax, or gas under the diaphragm in perforated viscus.[81]
Result
in patients with heart failure, will show pulmonary edema; excludes alternative diagnoses or triggers of chest pain
CBC
Test
CBC should be checked to look for anemia as it is a precipitating factor for angina, and thrombocytopenia to estimate risk of bleeding; unstable angina (UA) treatment increases the risk of bleeding. Thrombocytopenia is an independent predictor of poor outcomes, including death, major bleeds, and life-threatening prothrombotic events in UA.[1] Significant thrombocytopenia is defined as a platelet count <100,000/microliter or a relative drop of 50% from baseline.[1]
Also performed to detect possible secondary causes of UA (i.e., secondary blood loss, anemia). Anemia is common in UA and persistent or worsening anemia in ACS is associated with increased mortality and major bleeding.[1]
Result
normal, thrombocytopenia, anemia
electrolytes and renal function
Test
Recommended baseline test in patients with acute coronary syndrome for risk stratification (including as part of the Global Registry of Acute Coronary Events [GRACE] risk score), to determine the choice/dose of anticoagulant, and to help prevent contrast-induced nephropathy if an invasive strategy is planned in a patient with chronic kidney disease (CKD).[1]
It is important to remember that a patient with CKD may have a chronically elevated troponin.[2] Patients with CKD may also have electrolyte abnormalities that can cause ECG abnormalities. Impaired renal function is an independent predictor for mortality.[2]
Result
baseline levels
LFTs
Test
Measure liver function to include in the assessment of bleeding risk before starting anticoagulation.
Result
baseline levels
blood sugar
Test
Recommended for risk stratification.
If elevated, needs assessment for diabetes.
Result
normal; elevated in the presence of diabetes
CRP
Test
CRP is commonly ordered to rule out other causes of acute chest pain (e.g., pneumonia).
Result
elevated if infection present
lipid profile
Test
Recommended for risk stratification.
Target LDL <55 mg/dL (<1.4 mmol/L) if coronary artery disease present.[1]
Result
normal or increased total cholesterol and LDL
coagulation profile
Test
Recommended at baseline, as treatment options affect coagulation.
Result
normal
Investigations to avoid
Tests to consider
echocardiogram
Test
An emergent echocardiogram should always be performed in patients with cardiogenic shock or hemodynamic instability.[1][89] Point-of-care transthoracic echocardiogram can also be used to look for regional wall motion abnormalities of the left ventricle in patients with an atypical presentation or equivocal ECG, look for mechanical complications of acute MI (such as left ventricular function, right ventricular function, ventricular septal rupture, left ventricular free wall rupture, acute mitral regurgitation, pericardial effusion, cardiac tamponade) and for evidence to suggest alternative etiologies associated with chest pain (e.g., acute aortic disease, pulmonary embolism).[1][2][89][90][91]
A predischarge echocardiogram is indicated for all patients post-acute MI to assess left ventricular function after coronary reperfusion therapy and to guide prognostication.[92] Used to assist diagnosis in the acute stage if ECG is inconclusive.
May also provide information about precipitating causes such as aortic stenosis, hypertrophic cardiomyopathy, or pericardial effusion.
Result
transient regional wall motion abnormalities
coronary angiography
Test
Coronary angiography (with or without revascularization) should be considered for a patient with suspected unstable angina (with a negative troponin testing result) based on the risk assessment and clinical presentation, and is the investigation of choice for assessing the presence and severity of coronary artery disease, and allows concurrent treatment with angioplasty and stenting.[79][93]
Result
flow-limiting stenosis
functional (stress) testing
Test
Functional (stress) testing (e.g., stress echocardiography, perfusion/stress cardiac magnetic resonance [CMR] imaging, myocardial perfusion scan) may be considered by the cardiology team as part of the initial workup in patients with suspected ACS but nonelevated (or inconclusive) hs-cTn, no ECG changes, and no recurrence of pain.[1] They can also be performed following stabilization, to identify the extent of myocardial ischemia and direct patients for possible invasive management.[77]
However, do not perform stress CMR in patients with acute chest pain and high probability of coronary artery disease. Stress testing can increase risk and delay treatment for patients with acute chest pain and markers of high risk: for example, ST-segment elevation or positive cardiac biomarkers.[95]
Result
stress echocardiography: reversible regional wall motion abnormalities; perfusion/stress CMR: reversible (ischemic) defect; myocardial perfusion imaging: perfusion defect between stress and rest scan (reversible defects = ischemia, fixed defects = scar)
coronary CT angiography
Test
In patients with normal ECG and normal cardiac troponins, CT angiography to assess coronary artery anatomy, or rest myocardial perfusion imaging to exclude myocardial ischemia, may reasonably be performed.[2][77] Coronary CT angiography has been accepted in the acute setting to identify significant proximal coronary artery stenosis when ECG is not helpful and an intermediate clinical suspicion of acute coronary syndrome exists, as indicated by mild angina, prior MI, compensated or prior heart failure, diabetes, or renal insufficiency.[96][97]
However, do not use coronary CT angiography in high-risk emergency department patients presenting with acute chest pain as it is not indicated for patients with high-risk features: for example, ischemic ECG changes or positive cardiac markers.[1][95]
Result
flow-limiting stenosis
CT chest or MRI
Test
May be indicated for further evaluation and in particular for exclusion of conditions such as pulmonary embolism and aortic dissection.
Result
alternative diagnosis
Use of this content is subject to our disclaimer