Hyponatraemia
- Overview
- Theory
- Diagnosis
- Management
- Follow up
- Resources
Treatment algorithm
Please note that formulations/routes and doses may differ between drug names and brands, drug formularies, or locations. Treatment recommendations are specific to patient groups: see disclaimer
acute onset (<48 hours) and/or symptomatic
hypertonic (3%) saline infusion
Cerebral oedema occurs more frequently when hyponatraemia develops acutely (i.e., <48 hours). In patients with cerebral oedema, symptoms are usually severe (e.g., nausea/vomiting, altered mental status, somnolence, seizures, coma).[2]Spasovski G, Vanholder R, Allolio B, et al; Hyponatraemia Guideline Development Group. Clinical practice guideline on diagnosis and treatment of hyponatraemia. Eur J Endocrinol. 2014 Feb 25;170(3):G1-47. http://www.eje-online.org/content/170/3/G1.long http://www.ncbi.nlm.nih.gov/pubmed/24569125?tool=bestpractice.com
All patients with acute onset of hyponatraemia and/or symptoms should be treated promptly with hypertonic 3% saline.[2]Spasovski G, Vanholder R, Allolio B, et al; Hyponatraemia Guideline Development Group. Clinical practice guideline on diagnosis and treatment of hyponatraemia. Eur J Endocrinol. 2014 Feb 25;170(3):G1-47. http://www.eje-online.org/content/170/3/G1.long http://www.ncbi.nlm.nih.gov/pubmed/24569125?tool=bestpractice.com [3]Adrogué HJ, Tucker BM, Madias NE. Diagnosis and management of hyponatremia: a review. JAMA. 2022 Jul 19;328(3):280-91. http://www.ncbi.nlm.nih.gov/pubmed/35852524?tool=bestpractice.com [5]Ball S, Barth J, Levy M, et al. Society for Endocrinology endocrine emergency guidance: emergency management of severe symptomatic hyponatraemia in adult patients. Endocr Connect. 2016 Sep;5(5):G4-6. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5314809 http://www.ncbi.nlm.nih.gov/pubmed/27935814?tool=bestpractice.com
Usual regimen is 100-300 mL of hypertonic 3% saline (or 2-4 mL/kg) given in 100 mL increments over 10-20 minutes (usually as a bolus infusion) until symptom improvement occurs.[3]Adrogué HJ, Tucker BM, Madias NE. Diagnosis and management of hyponatremia: a review. JAMA. 2022 Jul 19;328(3):280-91. http://www.ncbi.nlm.nih.gov/pubmed/35852524?tool=bestpractice.com [5]Ball S, Barth J, Levy M, et al. Society for Endocrinology endocrine emergency guidance: emergency management of severe symptomatic hyponatraemia in adult patients. Endocr Connect. 2016 Sep;5(5):G4-6. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5314809 http://www.ncbi.nlm.nih.gov/pubmed/27935814?tool=bestpractice.com Evidence suggests that a ‘rapid intermittent bolus’ regime of fluid administration may be more effective at achieving the desired hourly reduction in sodium levels than a slow continuous infusion.[48]Baek SH, Jo YH, Ahn S, et al. Risk of overcorrection in rapid intermittent bolus vs slow continuous infusion therapies of hypertonic saline for patients with symptomatic hyponatremia: the SALSA randomized clinical trial. JAMA Intern Med. 2021 Jan 1;181(1):81-92. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7589081 http://www.ncbi.nlm.nih.gov/pubmed/33104189?tool=bestpractice.com
Recommendations regarding the rate of serum sodium correction vary, with some sources recommending a rate of 3-6 mmol/L/day, while others recommend a more aggressive rate of 8-12 mmol/L/day (in the first 24 hours).[2]Spasovski G, Vanholder R, Allolio B, et al; Hyponatraemia Guideline Development Group. Clinical practice guideline on diagnosis and treatment of hyponatraemia. Eur J Endocrinol. 2014 Feb 25;170(3):G1-47.
http://www.eje-online.org/content/170/3/G1.long
http://www.ncbi.nlm.nih.gov/pubmed/24569125?tool=bestpractice.com
[49]Sterns RH. Disorders of plasma sodium - causes, consequences, and correction. N Engl J Med. 2015 Jan 1;372(1):55-65.
http://www.ncbi.nlm.nih.gov/pubmed/25551526?tool=bestpractice.com
[50]Nagler EV, Vanmassenhove J, van der Veer SN, et al. Diagnosis and treatment of hyponatremia: a systematic review of clinical practice guidelines and consensus statements. BMC Med. 2014 Dec 11;12:1.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4276109
http://www.ncbi.nlm.nih.gov/pubmed/25539784?tool=bestpractice.com
A rate of 1-2 mmol/L/hour can be used for several hours if symptoms are severe.[24]Adrogué HJ, Madias NE. Hyponatremia. N Engl J Med. 2000 May 25;342(21):1581-9.
http://www.ncbi.nlm.nih.gov/pubmed/10824078?tool=bestpractice.com
A rate of <8 mmol/L/day is recommended to prevent myelinolysis.[24]Adrogué HJ, Madias NE. Hyponatremia. N Engl J Med. 2000 May 25;342(21):1581-9.
http://www.ncbi.nlm.nih.gov/pubmed/10824078?tool=bestpractice.com
[Figure caption and citation for the preceding image starts]: Brain magnetic resonance imaging of a patient with central pontine myelinolysis showing hypointensity within the basis pontisBMJ Case Reports 2013; doi:10.1136/bcr-2013-009970 [Citation ends].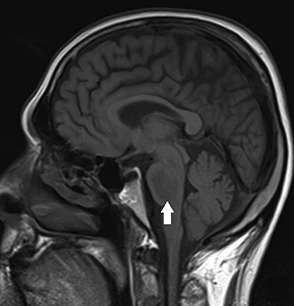 A more conservative approach to sodium correction is recommended in patients who have mild symptoms or who are asymptomatic.
A more conservative approach to sodium correction is recommended in patients who have mild symptoms or who are asymptomatic.
Avoid giving hypotonic fluids as this can worsen cerebral oedema.
Once desired serum sodium concentration is achieved, hypertonic 3% saline can be stopped and fluid repletion continued with a suitable fluid according to clinical conditions and to correct any ongoing losses.[5]Ball S, Barth J, Levy M, et al. Society for Endocrinology endocrine emergency guidance: emergency management of severe symptomatic hyponatraemia in adult patients. Endocr Connect. 2016 Sep;5(5):G4-6. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5314809 http://www.ncbi.nlm.nih.gov/pubmed/27935814?tool=bestpractice.com
supportive care
Treatment recommended for ALL patients in selected patient group
Supportive care (e.g., establishing intravenous access, giving supplemental oxygen, seizure control, intubation) should be initiated depending on the presentation.[3]Adrogué HJ, Tucker BM, Madias NE. Diagnosis and management of hyponatremia: a review. JAMA. 2022 Jul 19;328(3):280-91. http://www.ncbi.nlm.nih.gov/pubmed/35852524?tool=bestpractice.com
Serum sodium concentration should be tested every 2 hours to guide therapy until stabilisation occurs and hypertonic saline is no longer required. It should then be tested every 4-6 hours for 24 hours, and every 24 hours thereafter to monitor the ongoing rate of correction.[3]Adrogué HJ, Tucker BM, Madias NE. Diagnosis and management of hyponatremia: a review. JAMA. 2022 Jul 19;328(3):280-91. http://www.ncbi.nlm.nih.gov/pubmed/35852524?tool=bestpractice.com
Urine output should also be monitored as spontaneous diuresis can occur, which may lead to overcorrection of the serum sodium concentration. If urine output changes abruptly, serum sodium levels should be reassessed. A urine output of <2400 mL/24 hours (or 100 mL/hour) has been proposed as a safe upper limit during hyponatraemia correction, but this has yet to be validated.[51]Buchkremer F, Segerer S, Bock A. Monitoring urine flow to prevent overcorrection of hyponatremia: derivation of a safe upper limit based on the Edelman equation. Am J Kidney Dis. 2019 Jan;73(1):143-5. http://www.ncbi.nlm.nih.gov/pubmed/30122547?tool=bestpractice.com Urine studies should be obtained as early as possible as they may be affected by the administration of intravenous fluids.
treat underlying cause
Treatment recommended for ALL patients in selected patient group
Once the patient is stabilised, the underlying cause should be addressed.
Patients who do not improve may require further diagnostic assessment.
chronic onset (≥48 hours) or asymptomatic
isotonic fluid infusion
Isotonic intravenous fluids (e.g., normal saline 0.9% or a balanced solution such as lactated Ringer's solution) should be administered in 250-1000 mL boluses to maintain blood pressure. Boluses can be repeated as necessary, and then followed by an infusion of 0.5 to 1 mL/kg/hour to replete intravascular volume until signs and symptoms are no longer present.[2]Spasovski G, Vanholder R, Allolio B, et al; Hyponatraemia Guideline Development Group. Clinical practice guideline on diagnosis and treatment of hyponatraemia. Eur J Endocrinol. 2014 Feb 25;170(3):G1-47. http://www.eje-online.org/content/170/3/G1.long http://www.ncbi.nlm.nih.gov/pubmed/24569125?tool=bestpractice.com It is important that hypotonic fluids be avoided in these patients.
Recommendations regarding the rate of serum sodium correction vary. In patients with mild symptoms, or who are asymptomatic, 3-6 mmol/L/day may be appropriate. A rate of <8 mmol/L/day is recommended to prevent myelinolysis.[24]Adrogué HJ, Madias NE. Hyponatremia. N Engl J Med. 2000 May 25;342(21):1581-9. http://www.ncbi.nlm.nih.gov/pubmed/10824078?tool=bestpractice.com
Serum sodium concentration should be tested every 8-12 hours for 24 hours, and every 24 hours thereafter. It should be reassessed after repletion of volume as a concomitant disorder that is causing hyponatraemia may be present.
treat underlying cause
Treatment recommended for ALL patients in selected patient group
Underlying cause should be treated (e.g., treating severe nausea/vomiting, stopping diuretics if possible, treating mineralocorticoid deficiency).
fluid restriction
All patients should be placed on fluid restriction (including all oral and intravenous fluids) of 1 L/day.[2]Spasovski G, Vanholder R, Allolio B, et al; Hyponatraemia Guideline Development Group. Clinical practice guideline on diagnosis and treatment of hyponatraemia. Eur J Endocrinol. 2014 Feb 25;170(3):G1-47. http://www.eje-online.org/content/170/3/G1.long http://www.ncbi.nlm.nih.gov/pubmed/24569125?tool=bestpractice.com [3]Adrogué HJ, Tucker BM, Madias NE. Diagnosis and management of hyponatremia: a review. JAMA. 2022 Jul 19;328(3):280-91. http://www.ncbi.nlm.nih.gov/pubmed/35852524?tool=bestpractice.com This should be adjusted based on measured urine output and set at 500 mL less than daily urine volume (e.g., a patient producing 1200 mL/day of urine should be placed on 700 mL/day fluid restriction). This conservative approach should increase the serum sodium concentration gradually (i.e., <8 mmol/L/day) and helps to prevent myelinolysis, which can occur if sodium levels are corrected too quickly.
Electrolyte-free water excretion may be calculated. It is particularly useful in patients who are not responding to the general fluid restriction measures, and helps to determine the amount of free water restriction required to correct the serum sodium concentration.
Electrolyte-free water excretion = V × [1 - (UNa + UK)/(PNa)], where V is the urine flow rate, UNa is the urine concentration of sodium (mmol/L), UK is the urine concentration of potassium (mmol/L), and PNa is the plasma concentration of sodium (mmol/L).
If the value is positive, free water intake should be restricted to less than the electrolyte-free water excretion value, if feasible, in order to induce a negative free water balance. If the value is very low, this may be difficult to achieve. If the value is negative, free water restriction will not be effective and alternative treatment options (e.g., vaptans) should be considered.[43]Nguyen MK, Kurtz I. Derivation of a new formula for calculating urinary electrolyte-free water clearance based on the Edelman equation. Am J Physiol Renal Physiol. 2005 Jan;288(1):F1-7. https://journals.physiology.org/doi/full/10.1152/ajprenal.00259.2004 http://www.ncbi.nlm.nih.gov/pubmed/15383402?tool=bestpractice.com [44]Lindner G, Schwarz C. Electrolyte-free water clearance versus modified electrolyte-free water clearance: do the results justify the effort? Nephron Physiol. 2012;120(1):p1-5. http://www.ncbi.nlm.nih.gov/pubmed/22398459?tool=bestpractice.com
Serum sodium concentration should be tested every 8-12 hours for 24 hours, and every 24 hours thereafter.
treat underlying cause
Treatment recommended for ALL patients in selected patient group
Underlying cause should be treated. For patients with hypervolaemic hyponatraemia, causes include acute kidney injury/chronic kidney disease, congestive heart failure, cirrhosis, and nephrotic syndrome.
loop diuretic or spironolactone
Additional treatment recommended for SOME patients in selected patient group
A diuretic can be added if hypervolaemia is present and the underlying condition warrants it.[3]Adrogué HJ, Tucker BM, Madias NE. Diagnosis and management of hyponatremia: a review. JAMA. 2022 Jul 19;328(3):280-91. http://www.ncbi.nlm.nih.gov/pubmed/35852524?tool=bestpractice.com
Choice of agent depends on the underlying condition. Loop diuretics are recommended in patients with congestive heart failure or nephrotic syndrome, while spironolactone (an aldosterone receptor antagonist) is recommended in patients with cirrhosis and ascites. Thiazide diuretics should be avoided as they tend to worsen hyponatraemia.
The rate of correction of serum sodium should be closely monitored when using these agents and kept to <8 mmol/L/day to prevent myelinolysis.
Primary options
furosemide: 20-80 mg orally every 6-8 hours, increase dose gradually according to response, usual dose 40-120 mg/day, maximum 600 mg/day; 20-40 mg intravenously initially, increase dose by 20-40 mg every 2 hours as needed to achieve clinical response
OR
spironolactone: 25 mg/day orally initially given as a single dose or in 2 divided doses, increase gradually according to response, maximum 200 mg/day
vasopressin receptor antagonist + discontinue fluid restriction
If fluid restriction fails, a vasopressin receptor antagonist (also known as a vaptan) should be considered.[3]Adrogué HJ, Tucker BM, Madias NE. Diagnosis and management of hyponatremia: a review. JAMA. 2022 Jul 19;328(3):280-91. http://www.ncbi.nlm.nih.gov/pubmed/35852524?tool=bestpractice.com
Vaptans directly block the action of vasopressin on the kidneys, thereby reducing water retention.[3]Adrogué HJ, Tucker BM, Madias NE. Diagnosis and management of hyponatremia: a review. JAMA. 2022 Jul 19;328(3):280-91.
http://www.ncbi.nlm.nih.gov/pubmed/35852524?tool=bestpractice.com
[17]Grant P, Ayuk J, Bouloux PM, et al. The diagnosis and management of inpatient hyponatraemia and SIADH. Eur J Clin Invest. 2015 Aug;45(8):888-94.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4744950
http://www.ncbi.nlm.nih.gov/pubmed/25995119?tool=bestpractice.com
They have been shown to be safe and effective at slowly correcting serum sodium levels; however, they have not been shown to be associated with mortality benefits when used for the long-term treatment of congestive heart failure or hypervolaemic hyponatraemia.[52]Dixon MB, Lien YH. Tolvaptan and its potential in the treatment of hyponatremia. Ther Clin Risk Manag. 2008 Dec;4(6):1149-55.
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2643096
http://www.ncbi.nlm.nih.gov/pubmed/19337422?tool=bestpractice.com
[53]Nagler EV, Haller MC, Van Biesen W, et al. Interventions for chronic non-hypovolaemic hypotonic hyponatraemia. Cochrane Database Syst Rev. 2018 Jun 28;(6):CD010965.
https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD010965.pub2/full
http://www.ncbi.nlm.nih.gov/pubmed/29953167?tool=bestpractice.com
[  ]
What are the effects of vasopressin receptor antagonists (VRAs) for people with chronic non‐hypovolemic hypotonic hyponatremia?/cca.html?targetUrl=https://www.cochranelibrary.com/cca/doi/10.1002/cca.2244/fullShow me the answer There are also concerns that these drugs are associated with liver dysfunction.
]
What are the effects of vasopressin receptor antagonists (VRAs) for people with chronic non‐hypovolemic hypotonic hyponatremia?/cca.html?targetUrl=https://www.cochranelibrary.com/cca/doi/10.1002/cca.2244/fullShow me the answer There are also concerns that these drugs are associated with liver dysfunction.
Once a vaptan is started, fluid restriction is lifted in order to prevent overcorrection.[3]Adrogué HJ, Tucker BM, Madias NE. Diagnosis and management of hyponatremia: a review. JAMA. 2022 Jul 19;328(3):280-91. http://www.ncbi.nlm.nih.gov/pubmed/35852524?tool=bestpractice.com [54]Zhou Y, Yang W, Liu G, et al. Risks of vaptans in hypernatremia and serum sodium overcorrection: a systematic review and meta-analysis of randomised controlled trials. Int J Clin Pract. 2021 Jun;75(6):e13939. http://www.ncbi.nlm.nih.gov/pubmed/33336480?tool=bestpractice.com One systematic review found that treatment with a vaptan increased the risk of overcorrection by approximately 3% compared with placebo.[53]Nagler EV, Haller MC, Van Biesen W, et al. Interventions for chronic non-hypovolaemic hypotonic hyponatraemia. Cochrane Database Syst Rev. 2018 Jun 28;(6):CD010965. https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD010965.pub2/full http://www.ncbi.nlm.nih.gov/pubmed/29953167?tool=bestpractice.com
Primary options
tolvaptan: 15 mg orally once daily initially, increase gradually according to response, maximum 60 mg/day for up to 30 days
urea
Oral urea is supported as an alternative to vaptans in European and US hyponatraemia guidelines, although evidence from large multicentre randomised trials is lacking. The treatment is generally well tolerated and may be used in outpatient settings.[2]Spasovski G, Vanholder R, Allolio B, et al; Hyponatraemia Guideline Development Group. Clinical practice guideline on diagnosis and treatment of hyponatraemia. Eur J Endocrinol. 2014 Feb 25;170(3):G1-47. http://www.eje-online.org/content/170/3/G1.long http://www.ncbi.nlm.nih.gov/pubmed/24569125?tool=bestpractice.com [9]Verbalis JG, Grossman A, Höybye C, et al. Review and analysis of differing regulatory indications and expert panel guidelines for the treatment of hyponatremia. Curr Med Res Opin. 2014 Jul;30(7):1201-7. http://www.ncbi.nlm.nih.gov/pubmed/24809970?tool=bestpractice.com [55]Rondon-Berrios H, Tandukar S, Mor MK, et al. Urea for the treatment of hyponatremia. Clin J Am Soc Nephrol. 2018 Nov 7;13(11):1627-32. http://www.ncbi.nlm.nih.gov/pubmed/30181129?tool=bestpractice.com [56]Sterns RH, Silver SM, Hix JK. Urea for hyponatremia? Kidney Int. 2015 Feb;87(2):268-70. https://www.doi.org/10.1038/ki.2014.320 http://www.ncbi.nlm.nih.gov/pubmed/25635717?tool=bestpractice.com [57]Hoorn EJ, Zietse R. Diagnosis and treatment of hyponatremia: compilation of the guidelines. J Am Soc Nephrol. 2017 May;28(5):1340-9. https://journals.lww.com/jasn/fulltext/2017/05000/diagnosis_and_treatment_of_hyponatremia_.7.aspx http://www.ncbi.nlm.nih.gov/pubmed/28174217?tool=bestpractice.com
Primary options
urea: 15-60 g/day orally given in 1-4 divided doses, titrate according to serum sodium level, maximum 180 g/day
fluid restriction
All patients should be placed on fluid restriction (including all oral and intravenous fluids) of 1 L/day.[2]Spasovski G, Vanholder R, Allolio B, et al; Hyponatraemia Guideline Development Group. Clinical practice guideline on diagnosis and treatment of hyponatraemia. Eur J Endocrinol. 2014 Feb 25;170(3):G1-47. http://www.eje-online.org/content/170/3/G1.long http://www.ncbi.nlm.nih.gov/pubmed/24569125?tool=bestpractice.com [3]Adrogué HJ, Tucker BM, Madias NE. Diagnosis and management of hyponatremia: a review. JAMA. 2022 Jul 19;328(3):280-91. http://www.ncbi.nlm.nih.gov/pubmed/35852524?tool=bestpractice.com This should be adjusted based on measured urine output and set at 500 mL less than daily urine volume (e.g., a patient producing 1200 mL/day of urine should be placed on 700 mL/day fluid restriction). This conservative approach should increase the serum sodium concentration gradually (i.e., <8 mmol/L/day) and helps to prevent myelinolysis, which can occur if sodium levels are corrected too quickly.
Electrolyte-free water excretion may be calculated. It is particularly useful in patients who are not responding to the general fluid restriction measures, and helps to determine the amount of free water restriction required to correct the serum sodium concentration.
Electrolyte-free water excretion = V × [1 - (UNa + UK)/(PNa)], where V is the urine flow rate, UNa is the urine concentration of sodium (mmol/L), UK is the urine concentration of potassium (mmol/L), and PNa is the plasma concentration of sodium (mmol/L).
If the value is positive, free water intake should be restricted to less than the electrolyte-free water excretion value, if feasible, in order to induce a negative free water balance. If the value is very low, this may be difficult to achieve. If the value is negative, free water restriction will not be effective and alternative treatment options (e.g., vaptans) should be considered.[43]Nguyen MK, Kurtz I. Derivation of a new formula for calculating urinary electrolyte-free water clearance based on the Edelman equation. Am J Physiol Renal Physiol. 2005 Jan;288(1):F1-7. https://journals.physiology.org/doi/full/10.1152/ajprenal.00259.2004 http://www.ncbi.nlm.nih.gov/pubmed/15383402?tool=bestpractice.com [44]Lindner G, Schwarz C. Electrolyte-free water clearance versus modified electrolyte-free water clearance: do the results justify the effort? Nephron Physiol. 2012;120(1):p1-5. http://www.ncbi.nlm.nih.gov/pubmed/22398459?tool=bestpractice.com
Serum sodium concentration should be tested every 8-12 hours for 24 hours, and every 24 hours thereafter.
treat underlying cause
Treatment recommended for ALL patients in selected patient group
Underlying cause should be treated. For patients with euvolaemic hyponatraemia causes include causative medications and excess fluid intake (e.g., exercise, surgery, primary polydipsia, potomania). The syndrome of inappropriate antidiuretic hormone (SIADH) is characterised by hypotonic hyponatraemia, concentrated urine, and a euvolaemic state. See Syndrome of inappropriate antidiuretic hormone (Treatment algorithm).
vasopressin receptor antagonist + discontinue fluid restriction
If fluid restriction fails, a vasopressin receptor antagonist (also known as a vaptan) should be considered.[3]Adrogué HJ, Tucker BM, Madias NE. Diagnosis and management of hyponatremia: a review. JAMA. 2022 Jul 19;328(3):280-91. http://www.ncbi.nlm.nih.gov/pubmed/35852524?tool=bestpractice.com
Vaptans directly block the action of vasopressin on the kidneys, thereby reducing water retention.[3]Adrogué HJ, Tucker BM, Madias NE. Diagnosis and management of hyponatremia: a review. JAMA. 2022 Jul 19;328(3):280-91.
http://www.ncbi.nlm.nih.gov/pubmed/35852524?tool=bestpractice.com
[17]Grant P, Ayuk J, Bouloux PM, et al. The diagnosis and management of inpatient hyponatraemia and SIADH. Eur J Clin Invest. 2015 Aug;45(8):888-94.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4744950
http://www.ncbi.nlm.nih.gov/pubmed/25995119?tool=bestpractice.com
They have been shown to be safe and effective at slowly correcting serum sodium levels; however, they have not been shown to be associated with mortality benefits when used for the long-term treatment of euvolaemic hyponatraemia.[52]Dixon MB, Lien YH. Tolvaptan and its potential in the treatment of hyponatremia. Ther Clin Risk Manag. 2008 Dec;4(6):1149-55.
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2643096
http://www.ncbi.nlm.nih.gov/pubmed/19337422?tool=bestpractice.com
[53]Nagler EV, Haller MC, Van Biesen W, et al. Interventions for chronic non-hypovolaemic hypotonic hyponatraemia. Cochrane Database Syst Rev. 2018 Jun 28;(6):CD010965.
https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD010965.pub2/full
http://www.ncbi.nlm.nih.gov/pubmed/29953167?tool=bestpractice.com
[  ]
What are the effects of vasopressin receptor antagonists (VRAs) for people with chronic non‐hypovolemic hypotonic hyponatremia?/cca.html?targetUrl=https://www.cochranelibrary.com/cca/doi/10.1002/cca.2244/fullShow me the answer There are also concerns that these drugs are associated with liver dysfunction.
]
What are the effects of vasopressin receptor antagonists (VRAs) for people with chronic non‐hypovolemic hypotonic hyponatremia?/cca.html?targetUrl=https://www.cochranelibrary.com/cca/doi/10.1002/cca.2244/fullShow me the answer There are also concerns that these drugs are associated with liver dysfunction.
Once a vaptan is started, fluid restriction is lifted in order to prevent overcorrection.[3]Adrogué HJ, Tucker BM, Madias NE. Diagnosis and management of hyponatremia: a review. JAMA. 2022 Jul 19;328(3):280-91. http://www.ncbi.nlm.nih.gov/pubmed/35852524?tool=bestpractice.com [54]Zhou Y, Yang W, Liu G, et al. Risks of vaptans in hypernatremia and serum sodium overcorrection: a systematic review and meta-analysis of randomised controlled trials. Int J Clin Pract. 2021 Jun;75(6):e13939. http://www.ncbi.nlm.nih.gov/pubmed/33336480?tool=bestpractice.com One systematic review found that treatment with a vaptan increased the risk of overcorrection by approximately 3% compared with placebo.[53]Nagler EV, Haller MC, Van Biesen W, et al. Interventions for chronic non-hypovolaemic hypotonic hyponatraemia. Cochrane Database Syst Rev. 2018 Jun 28;(6):CD010965. https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD010965.pub2/full http://www.ncbi.nlm.nih.gov/pubmed/29953167?tool=bestpractice.com
Primary options
tolvaptan: 15 mg orally once daily initially, increase gradually according to response, maximum 60 mg/day for up to 30 days
urea
Oral urea is supported as an alternative to vaptans in European and US hyponatraemia guidelines, although evidence from large multicentre randomised trials is lacking. The treatment is generally well tolerated and may be used in outpatient settings.[2]Spasovski G, Vanholder R, Allolio B, et al; Hyponatraemia Guideline Development Group. Clinical practice guideline on diagnosis and treatment of hyponatraemia. Eur J Endocrinol. 2014 Feb 25;170(3):G1-47. http://www.eje-online.org/content/170/3/G1.long http://www.ncbi.nlm.nih.gov/pubmed/24569125?tool=bestpractice.com [9]Verbalis JG, Grossman A, Höybye C, et al. Review and analysis of differing regulatory indications and expert panel guidelines for the treatment of hyponatremia. Curr Med Res Opin. 2014 Jul;30(7):1201-7. http://www.ncbi.nlm.nih.gov/pubmed/24809970?tool=bestpractice.com [55]Rondon-Berrios H, Tandukar S, Mor MK, et al. Urea for the treatment of hyponatremia. Clin J Am Soc Nephrol. 2018 Nov 7;13(11):1627-32. http://www.ncbi.nlm.nih.gov/pubmed/30181129?tool=bestpractice.com [56]Sterns RH, Silver SM, Hix JK. Urea for hyponatremia? Kidney Int. 2015 Feb;87(2):268-70. https://www.doi.org/10.1038/ki.2014.320 http://www.ncbi.nlm.nih.gov/pubmed/25635717?tool=bestpractice.com [57]Hoorn EJ, Zietse R. Diagnosis and treatment of hyponatremia: compilation of the guidelines. J Am Soc Nephrol. 2017 May;28(5):1340-9. https://journals.lww.com/jasn/fulltext/2017/05000/diagnosis_and_treatment_of_hyponatremia_.7.aspx http://www.ncbi.nlm.nih.gov/pubmed/28174217?tool=bestpractice.com
Primary options
urea: 15-60 g/day orally given in 1-4 divided doses, titrate according to serum sodium level, maximum 180 g/day
overcorrection of serum sodium concentration
stop active treatment + initiate free water intake and/or desmopressin
If an overcorrection of more than 8-12 mmol/L/day of serum sodium concentration occurs, then prompt intervention is required to lower the serum sodium concentration.[2]Spasovski G, Vanholder R, Allolio B, et al; Hyponatraemia Guideline Development Group. Clinical practice guideline on diagnosis and treatment of hyponatraemia. Eur J Endocrinol. 2014 Feb 25;170(3):G1-47. http://www.eje-online.org/content/170/3/G1.long http://www.ncbi.nlm.nih.gov/pubmed/24569125?tool=bestpractice.com
All active treatment should be stopped and treatment with free water intake and/or desmopressin should be initiated.
The Adrogue-Madias formula can be used to determine the sodium-lowering effect of 1 litre of fluid (e.g., dextrose 5% in water): change in serum sodium concentration (per 1 litre) = (infusate sodium concentration - serum sodium concentration)/(total body water + 1); where serum sodium concentration is in mmol/L and total body water is in litres. Total body water in the equation can be estimated by using the following simple calculations: 0.5 × body weight in kilograms (for women and elderly men); 0.6 × body weight in kilograms (for younger men or children). Sodium concentration of common fluids (per litre): normal saline (0.9%): 154 mmol/L; lactated Ringer's solution: 130 mmol/L; dextrose 5% in water: 0 mmol/L; enteral water: 0 mmol/L. The sodium concentration of the infusate fluid must be known in order to use this formula, and the equation fails to take the ongoing water and electrolyte losses through urine and stool into account.[2]Spasovski G, Vanholder R, Allolio B, et al; Hyponatraemia Guideline Development Group. Clinical practice guideline on diagnosis and treatment of hyponatraemia. Eur J Endocrinol. 2014 Feb 25;170(3):G1-47. http://www.eje-online.org/content/170/3/G1.long http://www.ncbi.nlm.nih.gov/pubmed/24569125?tool=bestpractice.com [24]Adrogué HJ, Madias NE. Hyponatremia. N Engl J Med. 2000 May 25;342(21):1581-9. http://www.ncbi.nlm.nih.gov/pubmed/10824078?tool=bestpractice.com
The formula may be inadequate at predicting serum sodium levels in individual patients. For this reason, some physicians recommend paying careful attention to the initial changes in the serum sodium level and starting with 50% to 75% of the calculated infusion rate, and then adjusting the rate according to the serum sodium level.
Primary options
desmopressin: 1-2 micrograms intravenously twice daily

Choose a patient group to see our recommendations
Please note that formulations/routes and doses may differ between drug names and brands, drug formularies, or locations. Treatment recommendations are specific to patient groups. See disclaimer
Use of this content is subject to our disclaimer