Tests
1st tests to order
duplex ultrasonography
Test
In many centers, duplex ultrasonography is the first test ordered when carotid stenosis is suspected in an asymptomatic or symptomatic patient.[Figure caption and citation for the preceding image starts]: Echolucent internal carotid artery atheroma (yellow arrow) causing 70% stenosis (North American Symptomatic Carotid Endarterectomy Trial criteria). CCA = common carotid artery, ECA = external carotid artery, ICA = internal carotid artery, STA = superior thyroid arteryUsed with permission from BMJ 2013;346:f2420 [Citation ends].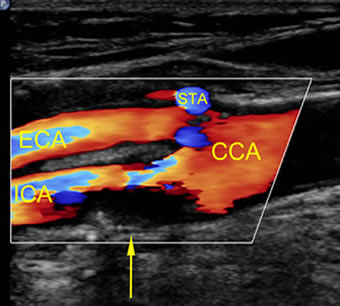
The most frequent reason for suspecting the diagnosis in an asymptomatic patient is the presence of atherosclerotic high-risk factors. (i.e., patients with peripheral arterial occlusive disease, coronary artery occlusive disease, hypertension, diabetes, hypercholesterolemia, or ages ≥55 years with active smoking).[11]
One study found that duplex ultrasonography will identify ≥70% stenosis with a sensitivity of 99%, specificity of 86%, and an overall accuracy of 95%.[21] One Cochrane review evaluating duplex ultrasound for diagnosis of symptomatic carotid stenosis found that it was accurate at discriminating between the presence or absence of significant carotid artery stenosis (<50% or 50% to 99%).[23]
Quantification is generally performed using the North American Symptomatic Carotid Endarterectomy Trial (NASCET) criteria, whereby the diameter of the arterial lumen at the tightest region of stenosis is compared with the region of the distal internal carotid artery that is free of disease and has nontapering walls.[24] These criteria have become accepted worldwide and other criteria are rarely used.
The formula used to calculate the degree of stenosis is:
Percentage stenosis = [1 - (minimum diameter/distal diameter)] × 100
Ultrasonography also identifies the anatomy, status of the contralateral carotid, collateral flow, and possible differential diagnoses.[25]
Result
elevated blood flow velocities along with visualization of details of the plaque within the carotid arteries; the velocities are translated into ranges of stenosis, generally categorized as mild (<50%), moderate (50% to 69%), high-grade (70% to 99%), and near-occlusion (a very tight and long stenosis from the carotid bifurcation to the base of the skull in the range of >95%, with collapse of the internal carotid artery is sometimes called a string sign or pseudo-occlusion)
computed tomography angiography (CTA) of head, neck, and chest
Test
CTA is the first line test for investigation of carotid stenosis in some centers and should also be ordered when results of duplex ultrasonography are equivocal, or fall in the moderate (50% to 69% diameter reduction) stenosis range, which is at the threshold where carotid artery revascularization may be necessary.
Should also be ordered when there is a need to evaluate the arterial anatomy proximal and distal to the cervical carotid artery, or to view the aortic arch before carotid stenting.
The best modality to determine the degree and length of stenosis. This is important when determining whether the patient is a candidate for carotid artery stenting or carotid endarterectomy.
The sensitivity and specificity for the diagnosis of a ≥70% stenosis are 85% and 93%, respectively.[26]
Noninvasive, less susceptible than magnetic resonance angiography (MRA) to overestimate the stenosis, and faster and less expensive than MRA.
Requires exposure to ionizing radiation, and the iodinated contrast is a hazard in patients with renal insufficiency.
Result
visualization of the narrowed carotid artery lumen; expressed as a specific percent stenosis; may also visualize the atherosclerotic plaque within the arterial wall; will demonstrate the arterial anatomy proximal and distal to the cervical carotid artery
Tests to consider
magnetic resonance angiography (MRA) of head, neck, and chest
Test
Less commonly performed than CTA, but preferred in some institutions with specialized capability for MRA. It is usually performed after injection of a contrast agent (contrast-enhanced MRA).
Should be ordered when results of duplex ultrasonography are equivocal, or fall in the moderate (50% to 69% diameter reduction) stenosis range, which is at the threshold where carotid artery revascularization may be necessary.
Should also be ordered when there is a need to evaluate the arterial anatomy proximal and distal to the cervical carotid artery, or to view the aortic arch before carotid stenting.
Noninvasive and does not require ionizing radiation.
Cannot be used in patients with ferromagnetic implants. Gadolinium-based contrast agents may not be used in renal insufficiency.
MRA has a tendency to overestimate stenosis severity. T2-weighted protocol will visualize and differentiate calcification (seen as black).
The sensitivity and specificity for the diagnosis of a ≥70% stenosis are 88% and 84%, respectively.[27]
Result
visualization of the narrowed carotid artery lumen; expressed as a specific percent stenosis; will also visualize details of the atherosclerotic plaque within the arterial wall; will demonstrate the arterial anatomy proximal and distal to the cervical carotid artery
CT brain
Test
In symptomatic patients, appropriate assessment of ischemic brain injury with CT is recommended when MRI is unavailable or contraindicated. All patients with transient ischemic attack or possible ischemic stroke should initially undergo a CT scan of the brain to rule out intracranial hemorrhage if an MRI has not been done and also to exclude stroke mimics.
Result
hypo-attenuation (darkness) of the brain parenchyma; loss of gray matter-white matter differentiation, and sulcal effacement
MRI brain
Test
In symptomatic patients, appropriate assessment of ischemic brain injury with MRI is recommended. It provides more accurate information about the stroke lesion compared with CT and can also identify intracranial hemorrhage. It is more sensitive to recent ischemia and previous hemorrhage than CT. In patients with recent stroke, special protocols can visualize changes as early as a few minutes after the event.
Result
acute ischemic infarct appears bright on diffusion-weighted imaging; at later stages, T2 images may also show increased signal in the ischemic territory; gradient echo or susceptibility weighted sequences are sensitive to previous hemorrhage
Use of this content is subject to our disclaimer