Etiology
The most common cause of carotid artery stenosis is atherosclerotic plaque in the cervical carotid artery. The unique hemodynamics at the carotid bifurcation predisposes this area to atherosclerosis. A small percentage of plaques may rupture and embolize to occlude intracranial arteries (causing a transient ischemic attack or stroke) or occlude retinal arteries (to cause transient monocular blindness or retinal strokes). Other less common causes include radiation arteritis, spontaneous or traumatic dissection, fibromuscular dysplasia, and restenosis after prior carotid artery revascularization.
Pathophysiology
Histologic evaluation of atherosclerotic plaques has demonstrated that they originate from fatty streaks that, over time, accumulate into a lipid core. The fatty streak becomes a fibroatheroma as fibrous tissue accumulates over the core and forms a fibrous cap. Through unknown mechanisms, some plaques become unstable resulting in an enlarging lipid core, intraplaque hemorrhage, plaque enlargement, thinning of the fibrous cap, fibrous cap rupture, ulceration, and luminal thrombosis.[9] These histomorphologic features have been associated with the production of atheroemboli and neurologic symptoms. These features have frequently been observed in explanted plaque specimens obtained from symptomatic patients.[Figure caption and citation for the preceding image starts]: Ruptured plaque with intraplaque hemorrhage explanted from a patient with carotid stenosis and a recent atheroembolic strokeFrom the personal collection of Brajesh K. Lal, MD [Citation ends].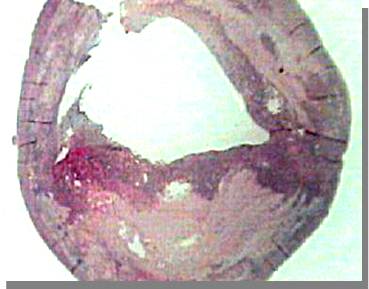 Conversely, small lipid cores located deep within the plaque with a thick fibrous cap have been observed in plaque specimens from patients with asymptomatic carotid stenosis.[Figure caption and citation for the preceding image starts]: Stable plaque with a small deep-seated lipid core explanted from a patient with a high-grade carotid stenosis without neurologic symptomsFrom the personal collection of Brajesh K. Lal, MD [Citation ends].
Conversely, small lipid cores located deep within the plaque with a thick fibrous cap have been observed in plaque specimens from patients with asymptomatic carotid stenosis.[Figure caption and citation for the preceding image starts]: Stable plaque with a small deep-seated lipid core explanted from a patient with a high-grade carotid stenosis without neurologic symptomsFrom the personal collection of Brajesh K. Lal, MD [Citation ends]. Duplex ultrasound and recent advances in computed tomography angiography (CTA) and magnetic resonance imaging allow more detailed characterization of plaques. This has the potential for defining high-risk lesions in the future.
Duplex ultrasound and recent advances in computed tomography angiography (CTA) and magnetic resonance imaging allow more detailed characterization of plaques. This has the potential for defining high-risk lesions in the future.
The unique hemodynamics at the carotid bifurcation predispose this area to atherosclerosis. Along the inner wall of the carotid bulb, blood flow remains laminar, with high velocity and high shear stress. Conversely, along the outer wall there are areas of flow separation, stasis, turbulent flow, and a complex oscillating shear stress pattern that predispose to atherosclerotic plaque deposition.[10]
Although rare neurologic events have been attributed to progressive stenosis and decreased blood flow from enlarging atherosclerotic plaques, most such events are secondary to plaque rupture with superimposed thrombosis and then embolization of thrombus from the lesion. Localized thrombosis can also lead to occlusion of the artery. Disruption of the fibrous cap with exposure of atherosclerotic debris to the flow lumen and embolization of cholesterol laden debris appears to be responsible for some embolic symptoms. Additional factors such as low cerebral perfusion pressure and poor collateralization, plaque ulceration or hemorrhage, hypotension, or a low cardiac output may also play a contributory role.
Classification
Based on symptomatic status[1][2]
Symptomatic: associated with atheroembolic focal neurologic symptoms such as stroke, transient ischemic attack, or amaurosis fugax within the last 6 months
Asymptomatic: not associated with focal neurologic symptoms within the last 6 months.
Based on etiology[1]
Atherosclerosis
Restenosis from neointimal hyperplasia after revascularization
Radiation-induced
Dissection
Fibromuscular dysplasia; carotid web (intimal variant of fibromuscular dysplasia).
Based on degree of stenosis[1]
Mild stenosis (<50% diameter reduction)
Moderate stenosis (50% to 69% diameter reduction)
Hemodynamically significant or high-grade stenosis (70% to 99% diameter reduction)
Near-occlusion; a very tight and often long stenosis from the carotid bifurcation to the base of the skull in the range of >95% with collapse of the internal carotid artery is sometimes called a string sign or pseudo-occlusion
Occlusion.
Use of this content is subject to our disclaimer