History and exam
Key diagnostic factors
common
history of malignancy
Hypercalcemia occurs in 20% to 30% of patients with cancer.[21][22] Cancer represents the most common etiology of hypercalcemia in the inpatient setting.[3] It can result from: humoral hypercalcemia of malignancy (characterized by tumor secretion of parathyroid hormone-related peptide [PTHrP]); local osteolytic hypercalcemia (characterized by local release of factors, including PTHrP, by bony metastases that promote osteoclast differentiation and function); calcitriol (1,25-dihydroxyvitamin D)-mediated hypercalcemia (characterized by autonomous production of calcitriol [(1,25-dihydroxyvitamin D)] by lymphoma cells); and ectopic hyperparathyroidism (characterized by tumor production of parathyroid hormone), which is very rare.[21][5]
Other diagnostic factors
common
normal physical exam
Hypercalcemia may not be associated with any specific physical examination findings.
poor skin turgor and/or dry mucous membranes
Signs of dehydration may be apparent on physical exam.
confusion
Hypercalcemia may be associated with neuropsychiatric symptoms.
fatigue
Hypercalcemia may be associated with neuropsychiatric symptoms.
constipation
Hypercalcemia is associated with gastrointestinal symptoms.
loss of appetite
Hypercalcemia is associated with gastrointestinal symptoms.
nausea
Hypercalcemia is associated with gastrointestinal symptoms.
polyuria
Hypercalcemia is associated with increased urinary excretion and dehydration by inducing nephrogenic diabetes insipidus.
polydipsia
Hypercalcemia is associated with increased urinary excretion and dehydration.
bone pain
Hypercalcemia is associated with bone pain.
Bone pain may be a feature of metastatic skeletal involvement.
uncommon
stupor
Hypercalcemia may be associated with neuropsychiatric symptoms. Stupor is a nonspecific symptom that may result from hypercalcemia, but has numerous toxic/metabolic and neurologic etiologies that need to be considered.
coma
Hypercalcemia may be associated with neuropsychiatric symptoms. Coma is a nonspecific symptom that may result from hypercalcemia, but has numerous toxic/metabolic and neurologic etiologies that need to be considered.
Risk factors
strong
nonmetastatic malignancy
metastatic skeletal involvement
Local osteolytic hypercalcemia occurs with disease complicated by widespread skeletal involvement.[1] Types of cancers include breast cancer and multiple myeloma.[1][5][10][Figure caption and citation for the preceding image starts]: CT chest showing compression fracture of multiple vertebral bodies in a child presenting with acute lymphoblastic leukemia. Biochemistry showed hypercalcemia with a suppressed parathyroid hormone levelSukumar SP, Balachandran K, Sahoo JP, et al. Acute lymphocytic leukaemia presenting as a metabolic bone disease. BMJ Case Reports 2013; doi:10.1136/bcr-2013-008758 [Citation ends].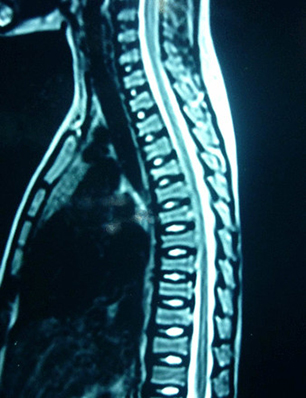 [Figure caption and citation for the preceding image starts]: Whole body planar images suggestive of skeletal infiltration in a child with acute lymphoblastic leukemia showing areas of abnormal increased uptake. Biochemistry showed hypercalcemia with a suppressed parathyroid hormone levelSukumar SP, Balachandran K, Sahoo JP, et al. Acute lymphocytic leukaemia presenting as a metabolic bone disease. BMJ Case Reports 2013; doi:10.1136/bcr-2013-008758 [Citation ends].
[Figure caption and citation for the preceding image starts]: Whole body planar images suggestive of skeletal infiltration in a child with acute lymphoblastic leukemia showing areas of abnormal increased uptake. Biochemistry showed hypercalcemia with a suppressed parathyroid hormone levelSukumar SP, Balachandran K, Sahoo JP, et al. Acute lymphocytic leukaemia presenting as a metabolic bone disease. BMJ Case Reports 2013; doi:10.1136/bcr-2013-008758 [Citation ends].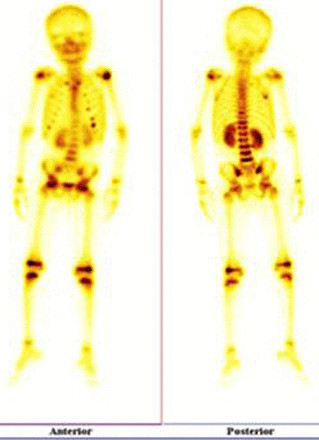
Use of this content is subject to our disclaimer