Aetiology
Humoral hypercalcaemia of malignancy is most commonly associated with:[1][2][10]
Renal cancer
Ovarian cancer
Breast cancer
Endometrial cancer
Human T-lymphotrophic virus-associated lymphoma
Squamous cell carcinoma.
Local osteolytic hypercalcaemia is most commonly associated with:[1][10]
Breast cancer
Multiple myeloma.
Calcitriol (1,25-dihydroxyvitamin D)-mediated hypercalcaemia is associated with:[1][10]
Lymphomas (of all types)
Granulomatous disease (such as active sarcoidosis) or tuberculosis.
Ectopic parathyroid hormone secretion by tumours is rare, but has been reported.[1][11][12]
Pathophysiology
Humoral hypercalcaemia of malignancy: tumour secretion of parathyroid hormone-related peptide (PTHrP) leads to activation of osteoclastic bone resorption and suppression of osteoblastic bone formation. This results in skeletal release of calcium and subsequent hypercalcaemia. PTHrP also acts at the level of the kidney to reduce calcium clearance, as well as to reduce the renal phosphorus threshold, leading to hyperphosphaturia and hypophosphataemia.[1][2]
Local osteolytic hypercalcaemia: in the setting of malignancy with widespread skeletal involvement, local release of cytokines (e.g., interleukin [IL]-1 and IL-6), chemokines, and PTHrP leads to increased osteoclastic bone resorption, and to increased release of calcium into the serum that overwhelms the kidney's capacity to clear calcium.[5][Figure caption and citation for the preceding image starts]: CT chest showing compression fracture of multiple vertebral bodies in a child presenting with acute lymphoblastic leukaemia. Biochemistry showed hypercalcaemia with a suppressed parathyroid hormone levelSukumar SP, Balachandran K, Sahoo JP, et al. Acute lymphocytic leukaemia presenting as a metabolic bone disease. BMJ Case Reports 2013; doi:10.1136/bcr-2013-008758 [Citation ends].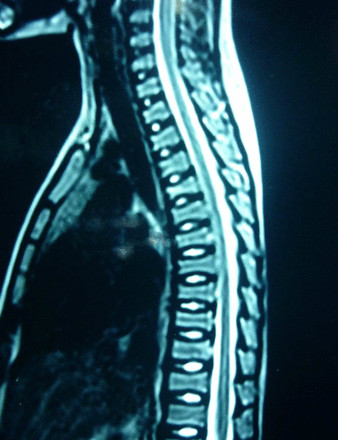 [Figure caption and citation for the preceding image starts]: Whole body planar images suggestive of skeletal infiltration in a child with acute lymphoblastic leukaemia showing areas of abnormal increased uptake. Biochemistry showed hypercalcaemia with a suppressed parathyroid hormone levelSukumar SP, Balachandran K, Sahoo JP, et al. Acute lymphocytic leukaemia presenting as a metabolic bone disease. BMJ Case Reports 2013; doi:10.1136/bcr-2013-008758 [Citation ends].
[Figure caption and citation for the preceding image starts]: Whole body planar images suggestive of skeletal infiltration in a child with acute lymphoblastic leukaemia showing areas of abnormal increased uptake. Biochemistry showed hypercalcaemia with a suppressed parathyroid hormone levelSukumar SP, Balachandran K, Sahoo JP, et al. Acute lymphocytic leukaemia presenting as a metabolic bone disease. BMJ Case Reports 2013; doi:10.1136/bcr-2013-008758 [Citation ends].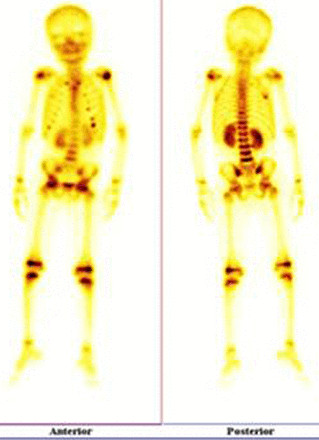
Calcitriol (1,25-dihydroxyvitamin D)-mediated hypercalcaemia: overexpression of 1-alpha hydroxylase (the enzyme that converts precursor 25-hydroxyvitamin D [25OHD] to calcitriol [(1,25-dihydroxyvitamin D)]) by malignant or adjacent normal cells leads to autonomous production of bioactive vitamin D.[1][5] Calcitriol (1,25-dihydroxyvitamin D) in turn increases intestinal calcium absorption and subsequent hypercalcaemia. In addition, calcitriol (1,25-dihydroxyvitamin D) may stimulate osteoclast-mediated bone resorption.[5]
Ectopic secretion of authentic parathyroid hormone with subsequent hypercalcaemia has been rarely reported.[1][11][12]
Classification
Severity
While there is no universally accepted classification of mild, moderate, or severe hypercalcaemia, the following criteria are widely used:[6][7][8]
Mild hypercalcaemia: total calcium of less than 3 mmol/L (<12 mg/dL) or ionised calcium of 1.4 to 2.0 mmol/L (5.6 to 8.0 mg/dL)
Moderate hypercalcaemia: total calcium of 3.0 to 3.5 mmol/L (12.0 to 13.9 mg/dL) or ionised calcium of 2.5 mmol/L or greater (≥10 mg/dL)
Severe hypercalcaemia: 3.5 mmol/L or greater (≥14 mg/dL) or ionised calcium of 2.5 to 3.0 mmol/L (10-12 mg/dL).
The National Cancer Institute's Common Terminology Criteria for Adverse Events (CTCAE) classifies hypercalcaemia of malignancy into four grades premised on corrected serum calcium:[9]
Grade 1: corrected serum calcium (SCa) of >upper limit of normal* to 2.9 mmol/L (11.5 mg/dL); ionised calcium >upper limit of normal to 1.5 mmol/L (6 mg/dL)
Grade 2: corrected SCa of >2.9 to 3.1 mmol/L (>11.5 to 12.5 mg/dL); ionised calcium >1.5 to 1.6 mmol/L (>6.0 to 6.4 mg/dL); symptomatic
Grade 3: corrected SCa of >3.1 to 3.4 mmol/L (>12.5 to 13.5 mg/dL); ionised calcium >1.6 to 1.8 mmol/L (>6.4 to 7.2 mg/dL); hospitalisation indicated
Grade 4: corrected SCa of >3.4 mmol/L (>13.5 mg/dL); ionized calcium >1.8 mmol/L (>7.2 mg/dL); life-threatening consequences.
*upper limit of normal: serum calcium 2.7 mmol/L (10.8 mg/dL); ionised calcium 1.3 mmol/L (5.3 mg/dL) (values may vary among laboratories)
Causes of hypercalcaemia of malignancy
Humoral hypercalcaemia of malignancy is most commonly associated with:[1][10]
Renal cancer
Ovarian cancer
Breast cancer
Endometrial cancer
Human T-lymphotrophic virus-associated lymphoma
Squamous cell carcinoma.
Local osteolytic hypercalcaemia is most commonly associated with:[1][10]
Breast cancer
Multiple myeloma.
Calcitriol (1,25-dihydroxyvitamin D)-mediated hypercalcaemia is associated with:[1][10]
Lymphomas (of all types)
Granulomatous disease (such as active sarcoidosis) or tuberculosis.
Ectopic parathyroid hormone secretion by tumours is rare, but has been reported.[1][11][12]
Use of this content is subject to our disclaimer