Etiology
Ptosis is an important and often under-recognized cause of vision loss. The condition may be a manifestation of a number of local and systemic conditions that require further evaluation. Understanding the cause guides further evaluation and enhances the utility of diagnostic testing.[4][5][6]
Infectious or inflammatory
The presence of decreased vision, globe proptosis (displacement of eyeball from eye socket), and significant pain suggest an infectious or inflammatory process.
Chalazion is a very common cause of ptosis resulting from focal inflammation of an obstructed meibomian gland. Lesions may be associated with pain and local or diffuse erythema.
Stye (hordeolum) presents in similar fashion to chalazion, and represents an acute infection of secretions within eyelid sebaceous glands.
Uveitis represents inflammation of the iris, ciliary body, or choroid, resulting from traumatic, infectious, autoimmune, or neoplastic causes.[7] Ptosis is a secondary response to ocular pain, photophobia, and eyelid edema. Uveitis has no direct relation to the onset of ptosis; however, patients may present with ptosis as a compensatory mechanism related to photophobia. Mild periorbital edema and erythema may be present. Prompt ophthalmologic evaluation is necessary for appropriate diagnosis and treatment.
Blepharochalasis is a rare familial variant of angioneurotic edema that occurs during adolescence or young adulthood. It is characterized by recurrent episodes of inflammatory eyelid edema. After several episodes, the eyelid skin has a crepe-paper-like appearance. True ptosis may coexist secondary to attenuation of the levator aponeurosis.[8]
The presence of headache, vision loss, and a third nerve palsy is suspicious for giant cell (temporal) arteritis. Urgent ophthalmologic evaluation is necessary to prevent permanent loss of vision.
Preseptal cellulitis is an inflammation of the structures anterior to the orbital septum. It is a relatively common local or diffuse infectious process of the periorbital tissues resulting from superficial trauma, chalazia, hordeola, and styes, or adjacent sinus infection. Visual acuity and extraocular movement are not affected.
Orbital cellulitis is characterized anatomically by infectious involvement of tissues posterior to the orbital septum. Orbital cellulitis is an ophthalmic emergency with vision-threatening implications from adjacent sinus infection, recent trauma, facial surgery, or immunocompromised state.
Orbital inflammatory syndrome (OIS) is an inflammatory process of orbital soft tissue affecting children and adults. The subtype is specified by nature of involvement, such as dacryoadenitis (most common) or myositis. Systemic infectious, autoimmune, and neoplastic etiologies are often implicated, while some cases are idiopathic.
Autoimmune
Ptosis may be a result of an underlying autoimmune disorder, such as myasthenia gravis, multiple sclerosis (MS) or thyroid eye disease.
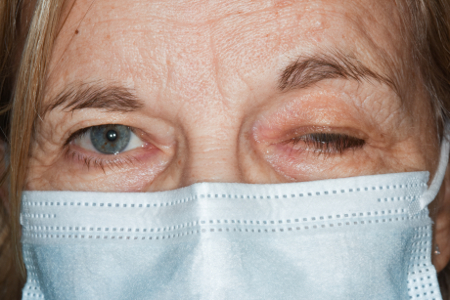
Myasthenia gravis is an immunologic condition characterized by blockage of neuromuscular transmission resulting in local or diffuse weakness. Ptosis is the most common sign. Generalized weakness associated with dysphonia, dysphagia, and dyspnea is highly suspicious for airway and respiratory compromise, findings that require urgent evaluation. Diagnosis is verified through clinical history, provocative testing, serum assays, or electromyogram studies.[9][Figure caption and citation for the preceding image starts]: Drooping eyelid (ptosis) in 69 year old female patient due to myasthenia gravis (MG). MG is a rare autoimmune neuromuscular disorder that weakens and fatigues the body's voluntary muscles, which include the muscles that control movement of the eyes and eyelidsDr P Marazzi/Science Photo Library; used with permission [Citation ends].
MS is rarely associated with isolated ptosis, as diagnosis requires recognizing neurologic signs and symptoms over time, and identifying lesions affecting different areas of the central nervous system. Ophthalmologic symptoms, when they occur, reflect optic nerve or brainstem white matter involvement. Decreased vision, ocular pain with eye movement, and ocular dysmotility are common signs and symptoms of MS.
Thyroid eye disease (Graves disease) is an autoimmune inflammatory disorder with potential vision-threatening complications. It is the most common cause of eyelid retraction and both unilateral and bilateral proptosis. Orbital disease does not necessarily accompany thyroid disease, and patients may be hyperthyroid, hypothyroid, or euthyroid. Strabismus and diplopia secondary to restrictive extraocular myopathy is common. Women are affected more than men, in a bimodal age distribution (middle-aged and older adults). Decreased visual acuity, visual field abnormalities, and relative afferent pupillary defects suggest compressive optic neuropathy for which urgent ophthalmologic or oculoplastic referral is indicated.[10]
Iatrogenic
Iatrogenic causes of ptosis include previous eye or eyelid surgery.
Previous eye or eyelid surgery may cause disinsertion and dehiscence of the levator aponeurosis from its tarsal attachments.
Surgical implants may restrict action of the extraocular muscles or ultimately lead to globe malposition.
Some patients may develop ptosis from gold weight eyelid implants for paralytic lagophthalmos or a scleral buckle for retinal detachment repair.
Depending on the nature of the implant, measurements of palpebral fissure (widest point between the upper and lower eyelid in primary gaze), margin to reflex distance (distance from a corneal light reflex in primary gaze to the upper eyelid), and levator function (excursion of the upper eyelid in downgaze to upgaze with the frontalis muscle immobilized) can be variable.
[Figure caption and citation for the preceding image starts]: Measurement of vertical interpalpebral fissureFrom the collection of Dr Allen Putterman [Citation ends].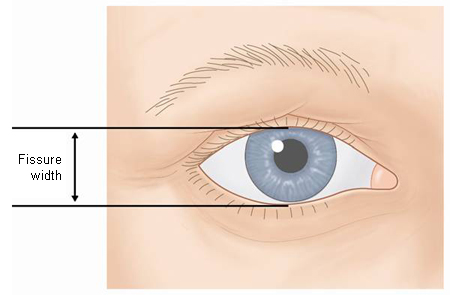 [Figure caption and citation for the preceding image starts]: Position of upper eyelid in downgazeFrom the collection of Dr Allen Putterman [Citation ends].
[Figure caption and citation for the preceding image starts]: Position of upper eyelid in downgazeFrom the collection of Dr Allen Putterman [Citation ends]. [Figure caption and citation for the preceding image starts]: Position of upper eyelid in upgazeFrom the collection of Dr Allen Putterman [Citation ends].
[Figure caption and citation for the preceding image starts]: Position of upper eyelid in upgazeFrom the collection of Dr Allen Putterman [Citation ends].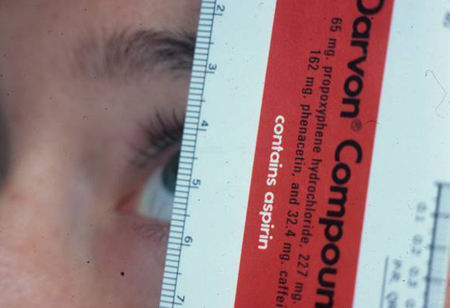 [Figure caption and citation for the preceding image starts]: Measurement of margin-reflex distanceFrom the collection of Dr Allen Putterman [Citation ends].
[Figure caption and citation for the preceding image starts]: Measurement of margin-reflex distanceFrom the collection of Dr Allen Putterman [Citation ends].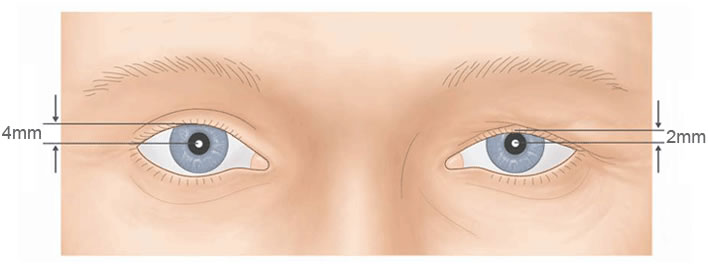 [Figure caption and citation for the preceding image starts]: Ptosis in an 89 year old male patient following a botox injection to correct double vision (diplopia)Dr P Marazzi/Science Photo Library; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Ptosis in an 89 year old male patient following a botox injection to correct double vision (diplopia)Dr P Marazzi/Science Photo Library; used with permission [Citation ends].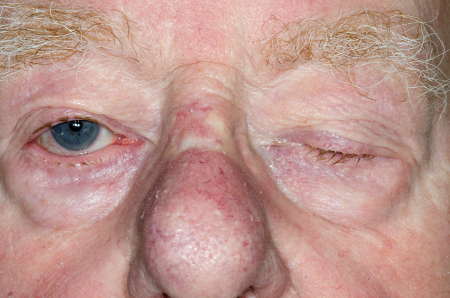
Mechanical
Mechanical ptosis involves a mass lesion (tumor or foreign body) governing eyelid position and motility.
Globe malposition refers to any process that alters the normal anatomic position of the globe within the orbit, including volume changes of the globe. Alterations of this relationship result in eyelid malposition.
Eyelid tumors cause a mechanical form of ptosis. The location and size of the lesion determine the severity of eyelid malposition. Symptomatic benign and malignant lesions are often treated with surgical excision and eyelid reconstruction. Lesions of significant size, resulting in disruption of eyelid architecture or involving the medial and lateral canthi, are more likely to invade the orbit and surrounding structures. All neoplastic eyelid lesions are referred to surgeons experienced in eyelid reconstruction to prevent ocular complications.
Orbital tumors cause neurogenic and mechanical forms of ptosis, and disrupt orbital architecture resulting in pseudoptosis. The type of lesion and its location determine the clinical manifestations. Certain tumors cause profound vision loss, proptosis, strabismus, and pain. Others are asymptomatic. All orbital lesions require evaluation by an ophthalmologist or oculoplastic surgeon.
Neurogenic
Neurogenic causes of ptosis should raise suspicion for vision-threatening and life-threatening conditions.
Benign essential blepharospasm (BEB) is a bilateral facial dystonia affecting the orbicularis oculi, corrugator, and procerus muscles. Patients present with progressive, involuntary eyelid twitching, blinking, or closure. Benign Essential Blepharospasm Research Foundation Opens in new window Symptoms are often worse during visual tasks (e.g., reading or driving), rendering patients functionally blind.
Chronic progressive external ophthalmoplegia (CPEO) is an inherited condition manifest by progressive, symmetric extraocular muscle paresis and ptosis. Patients often do not complain of diplopia despite obvious strabismus. Potential life-threatening systemic findings, such as cardiac conduction defects in Kearns-Sayre syndrome, may coexist.[11]
Third nerve (oculomotor) palsy is an acute-onset dysfunction of eyelid and extraocular motility resulting in ptosis and strabismus. Involvement may be partial or complete. Most cases are ischemic in origin, reflecting comorbid hypertension, diabetes mellitus, and arteriosclerotic disease. Pupillary abnormalities (e.g., dilated pupil that responds poorly to light) suggest nerve compression, neoplastic, and aneurysmal processes.[12][Figure caption and citation for the preceding image starts]: Oculomotor nerve palsy. Face of a 36-year-old woman with third nerve palsy after surgery to treat a subarachnoid haemorrhage. A berry aneurysm, a common localised dilation of an intercranial artery, caused the subarachnoid hemorrhage. Third nerve palsy is a dysfunction of the third cranial nerve, the oculomotor nerve, which controls the movement of the eyes. It leads to an inability to move the eye, double vision, a fixed and non-reactive pupil and eyelid drooping (ptosis, seen here, right eye)Dr P Marazzi/Science Photo Library; used with permission [Citation ends].
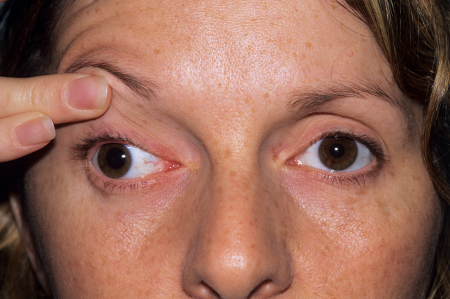 [Figure caption and citation for the preceding image starts]: Oculomotor nerve palsy. Face of a 36-year-old woman with third nerve palsy after surgery to treat a subarachnoid haemorrhage. A berry aneurysm, a common localised dilation of an intercranial artery, caused the subarachnoid hemorrhage. Third nerve palsy is a dysfunction of the third cranial nerve, the oculomotor nerve, which controls the movement of the eyes. It leads to an inability to move the eye, double vision, a fixed and non-reactive pupil and eyelid drooping (ptosis, seen here, right eye)Dr P Marazzi/Science Photo Library; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Oculomotor nerve palsy. Face of a 36-year-old woman with third nerve palsy after surgery to treat a subarachnoid haemorrhage. A berry aneurysm, a common localised dilation of an intercranial artery, caused the subarachnoid hemorrhage. Third nerve palsy is a dysfunction of the third cranial nerve, the oculomotor nerve, which controls the movement of the eyes. It leads to an inability to move the eye, double vision, a fixed and non-reactive pupil and eyelid drooping (ptosis, seen here, right eye)Dr P Marazzi/Science Photo Library; used with permission [Citation ends].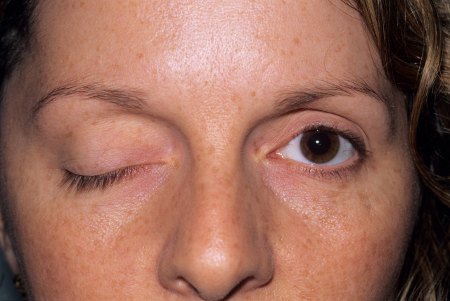
Horner syndrome is a lesion in the sympathetic pathway resulting in ptosis, miosis, and variable degrees of anhidrosis. Involvement of the inferior tarsal muscle (analog to the upper eyelid, superior tarsal muscle) results in lower eyelid elevation with a further decrease in vertical interpalpebral fissure and pseudo-enophthalmos. Evaluation for an occult malignancy, vascular dissection, or an aneurysm is recommended in these cases.[13]
A stroke results in a constellation of neurologic findings determined by the location of ischemia or hemorrhage. Clinical observations and measurements may be difficult to interpret and often are inconsistent. Ptosis may be prominent following a stroke involving the vertebrobasilar circulation. Management of resultant ischemic injury and edema is paramount.
Traumatic
Traumatic ptosis results from direct trauma to the levator muscle, its aponeurosis, or the superior tarsal muscle.
Levator muscle trauma may result in partial and complete transection of the levator aponeurosis. Ptosis results from disruption of the soft-tissue and bony attachments, or globe malposition. Globe inspection is mandatory, with a low threshold of action in pursuing head and orbital imaging or seeking ophthalmologic consultation. Eyelid function depends on the extent of injury incurred.
An eyelid foreign body may reflect previous trauma or surgical intervention. Eyelid laceration is evident by clinical history and physical exam. Determination of levator function may be difficult secondary to soft-tissue edema. Wound characteristics are important to identify (e.g., prolapse of orbital fat). Urgent surgical referral is necessary for primary wound evaluation and repair.
Orbital and facial fractures may be associated with trauma to orbital and intracranial structures and adjacent paranasal sinuses. Surgical reduction and repair is indicated for significant enophthalmos and ptosis, diplopia, or soft-tissue and extraocular muscle entrapment. Prosthesis fitting may be indicated in congenital micro-ophthalmos, or postenucleation (total globe removal) and postevisceration (partial globe removal with sclera and ocular musculature intact) patients.[Figure caption and citation for the preceding image starts]: Male patient suffering from post-traumatic acquired ptosis, likely caused by an injury to the eyelidBarraquer, Barcelona - ISM/Science Photo Library; used with permission [Citation ends].

Age-related or congenital
Age-related laxity of the periorbital and orbital soft tissue is often a corollary to aponeurotic and involutional forms of ptosis. Eyelid pathology with changes to the eyelid retractors and supportive soft tissue represents the vast majority of conditions that cause ptosis and pseudoptosis.
Involutional (age-related) changes to the forehead skin result in brow ptosis, headache, brow ache, and prominent transverse forehead furrows with chronic contracture. Orbital fat prolapses forward secondary to attenuation of the orbital septum.
Dermatochalasis (redundancy and laxity of eyelid skin) more commonly affects older adults and often coexists with true eyelid ptosis. Patients may present with similar symptoms of brow ache, eyelashes in the visual field, and loss of superior visual field. The upper eyelid crease may be obscured.
Congenital myogenic ptosis results from dysgenesis of the levator muscle, originating from birth. Muscle fibers are replaced by fibrofatty tissue, which decreases the ability of the muscle to contract effectively.[14] Children with congenital myogenic ptosis may have amblyopia, especially in cases of bilateral asymmetry. Acquired forms (rare) may be a manifestation of local or diffuse disease.[Figure caption and citation for the preceding image starts]: Bilateral, asymmetric, congenital myogenic ptosisMid Essex Hospital Services NHS Trust/Science Photo Library; used with permission [Citation ends].
 [Figure caption and citation for the preceding image starts]: Ptosis in a 6-year-old boy. Ptosis is normally due to weakness of the levator muscle of the upper eyelid, here of the left eye (at right). This patient has had this condition since birth, and has had three operations aimed at correcting the conditionMid Essex Hospital Services NHS Trust/Science Photo Library; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Ptosis in a 6-year-old boy. Ptosis is normally due to weakness of the levator muscle of the upper eyelid, here of the left eye (at right). This patient has had this condition since birth, and has had three operations aimed at correcting the conditionMid Essex Hospital Services NHS Trust/Science Photo Library; used with permission [Citation ends].
Blepharophimosis is an autosomal-dominant, congenital eyelid syndrome presenting with severe ptosis, telecanthus, and epicanthus inversus.
Use of this content is subject to our disclaimer