Mallory-Weiss tear
- Overview
- Theory
- Diagnosis
- Management
- Follow up
- Resources
Treatment algorithm
Please note that formulations/routes and doses may differ between drug names and brands, drug formularies, or locations. Treatment recommendations are specific to patient groups: see disclaimer
Look out for this icon: for treatment options that are affected, or added, as a result of your patient's comorbidities.
active non-variceal bleeding
resuscitation plus supportive care
Prioritise resuscitation in line with standard ABC practice; protect the airway to prevent aspiration and obtain peripheral venous access. Follow your local protocol.
Give intravenous fluids to all patients.[31]Siau K, Hearnshaw S, Stanley AJ, et al. British Society of Gastroenterology (BSG)-led multisociety consensus care bundle for the early clinical management of acute upper gastrointestinal bleeding. Frontline Gastroenterol. 2020 Mar 27;11(4):311-23. https://www.bsg.org.uk/wp-content/uploads/2019/11/flgastro-2019-101395.pdf http://www.ncbi.nlm.nih.gov/pubmed/32582423?tool=bestpractice.com
Monitor the patient using a validated early warning score (e.g., National Early Warning Score 2 [NEWS2]) and use clinical review to determine the infusion rate for your patient.[31]Siau K, Hearnshaw S, Stanley AJ, et al. British Society of Gastroenterology (BSG)-led multisociety consensus care bundle for the early clinical management of acute upper gastrointestinal bleeding. Frontline Gastroenterol. 2020 Mar 27;11(4):311-23. https://www.bsg.org.uk/wp-content/uploads/2019/11/flgastro-2019-101395.pdf http://www.ncbi.nlm.nih.gov/pubmed/32582423?tool=bestpractice.com NEWS2 Opens in new window
Guidelines from the National Institute for Health and Care Excellence (NICE) in the UK and a consensus care bundle for acute upper gastrointestinal bleeding led by the British Society of Gastroenterology (BSG) recommend using a crystalloid solution as a bolus of 500 mL in less than 15 minutes in haemodynamically unstable patients.[31]Siau K, Hearnshaw S, Stanley AJ, et al. British Society of Gastroenterology (BSG)-led multisociety consensus care bundle for the early clinical management of acute upper gastrointestinal bleeding. Frontline Gastroenterol. 2020 Mar 27;11(4):311-23. https://www.bsg.org.uk/wp-content/uploads/2019/11/flgastro-2019-101395.pdf http://www.ncbi.nlm.nih.gov/pubmed/32582423?tool=bestpractice.com [54]National Institute for Health and Care Excellence. Intravenous fluid therapy in adults in hospital. May 2017 [internet publication]. https://www.nice.org.uk/guidance/cg174 The European Society of Gastrointestinal Endoscopy (ESGE) guidelines recommend prompt intravascular volume replacement using crystalloid fluids in haemodynamically unstable patients.[32]Gralnek IM, Stanley AJ, Morris AJ, et al. Endoscopic diagnosis and management of nonvariceal upper gastrointestinal hemorrhage (NVUGIH): European Society of Gastrointestinal Endoscopy (ESGE) guideline - update 2021. Endoscopy. 2021 Mar;53(3):300-32. https://www.thieme-connect.com/products/ejournals/html/10.1055/a-1369-5274 http://www.ncbi.nlm.nih.gov/pubmed/33567467?tool=bestpractice.com
Practical tip
Before diagnostic endoscopy consider intubating the patient if needed (e.g., if there is haematemesis, or there is a perceived risk of a haemodynamically unstable patient having blood in the stomach, or if the patient presents with an altered mental status).Make sure the patient is appropriately resuscitated before undergoing diagnostic endoscopy.
Request an urgent critical care review for any patient with ongoing haemodynamic instability despite adequate resuscitative efforts. Consider activating major haemorrhage protocols early.[31]Siau K, Hearnshaw S, Stanley AJ, et al. British Society of Gastroenterology (BSG)-led multisociety consensus care bundle for the early clinical management of acute upper gastrointestinal bleeding. Frontline Gastroenterol. 2020 Mar 27;11(4):311-23. https://www.bsg.org.uk/wp-content/uploads/2019/11/flgastro-2019-101395.pdf http://www.ncbi.nlm.nih.gov/pubmed/32582423?tool=bestpractice.com
Consider seeking advice from an appropriate specialist if the patient is taking warfarin or a direct oral anticoagulant (DOAC).
The BSG consensus care bundle for acute upper gastrointestinal bleeding and the 2021 update to the BSG and ESGE guideline on endoscopy in patients on antiplatelet or anticoagulant therapy recommend:[31]Siau K, Hearnshaw S, Stanley AJ, et al. British Society of Gastroenterology (BSG)-led multisociety consensus care bundle for the early clinical management of acute upper gastrointestinal bleeding. Frontline Gastroenterol. 2020 Mar 27;11(4):311-23. https://www.bsg.org.uk/wp-content/uploads/2019/11/flgastro-2019-101395.pdf http://www.ncbi.nlm.nih.gov/pubmed/32582423?tool=bestpractice.com [64]Veitch AM, Radaelli F, Alikhan R, et al. Endoscopy in patients on antiplatelet or anticoagulant therapy: British Society of Gastroenterology (BSG) and European Society of Gastrointestinal Endoscopy (ESGE) guideline update. Gut. 2021 Sep;70(9):1611-28. https://www.bsg.org.uk/wp-content/uploads/2021/08/BSG_ESGE-antiplatelet-and-anticoagulant-update-2021.pdf http://www.ncbi.nlm.nih.gov/pubmed/34362780?tool=bestpractice.com
Suspending DOACs at presentation and seeking advice from a haematologist when managing patients with severe haemorrhage to weigh up the risks and benefits of the DOAC
Suspending warfarin at presentation
The BSG consensus care bundle stresses the importance of ensuring a plan is in place for restarting warfarin.[31]Siau K, Hearnshaw S, Stanley AJ, et al. British Society of Gastroenterology (BSG)-led multisociety consensus care bundle for the early clinical management of acute upper gastrointestinal bleeding. Frontline Gastroenterol. 2020 Mar 27;11(4):311-23. https://www.bsg.org.uk/wp-content/uploads/2019/11/flgastro-2019-101395.pdf http://www.ncbi.nlm.nih.gov/pubmed/32582423?tool=bestpractice.com Consult a specialist to discuss the risks associated with stopping warfarin and the need for monitoring.[31]Siau K, Hearnshaw S, Stanley AJ, et al. British Society of Gastroenterology (BSG)-led multisociety consensus care bundle for the early clinical management of acute upper gastrointestinal bleeding. Frontline Gastroenterol. 2020 Mar 27;11(4):311-23. https://www.bsg.org.uk/wp-content/uploads/2019/11/flgastro-2019-101395.pdf http://www.ncbi.nlm.nih.gov/pubmed/32582423?tool=bestpractice.com [64]Veitch AM, Radaelli F, Alikhan R, et al. Endoscopy in patients on antiplatelet or anticoagulant therapy: British Society of Gastroenterology (BSG) and European Society of Gastrointestinal Endoscopy (ESGE) guideline update. Gut. 2021 Sep;70(9):1611-28. https://www.bsg.org.uk/wp-content/uploads/2021/08/BSG_ESGE-antiplatelet-and-anticoagulant-update-2021.pdf http://www.ncbi.nlm.nih.gov/pubmed/34362780?tool=bestpractice.com
In haemodynamically unstable patients, the 2021 update to the BSG and ESGE guideline recommends:[64]Veitch AM, Radaelli F, Alikhan R, et al. Endoscopy in patients on antiplatelet or anticoagulant therapy: British Society of Gastroenterology (BSG) and European Society of Gastrointestinal Endoscopy (ESGE) guideline update. Gut. 2021 Sep;70(9):1611-28. https://www.bsg.org.uk/wp-content/uploads/2021/08/BSG_ESGE-antiplatelet-and-anticoagulant-update-2021.pdf http://www.ncbi.nlm.nih.gov/pubmed/34362780?tool=bestpractice.com
In patients who are taking warfarin, give intravenous vitamin K and four-factor prothrombin complex concentrate. Fresh frozen plasma can be used if prothrombin complex concentrate is not available
If the patient is taking a DOAC, consider the use of reversal agents: idarucizumab in patients taking dabigatran, and andexanet alfa in patients taking anti-factor Xa. Intravenous four-factor prothrombin complex concentrate can be used if andexanet alfa is not available.
Note that NICE recommends:[33]National Institute for Health and Care Excellence. Acute upper gastrointestinal bleeding in over 16s: management. August 2016 [internet publication]. https://www.nice.org.uk/guidance/cg141
Prothrombin complex concentrate in patients who are taking warfarin and actively bleeding
Following local warfarin protocols to treat patients who are taking warfarin and whose upper gastrointestinal bleeding has stopped
Recombinant factor Vlla (eptacog alfa) when all other methods have failed.
If any medications are temporarily stopped, also seek advice on the appropriate time for these to be restarted. The 2021 update to the BSG and ESGE guideline on endoscopy in patients on antiplatelet or anticoagulant therapy recommends restarting anticoagulation:[64]Veitch AM, Radaelli F, Alikhan R, et al. Endoscopy in patients on antiplatelet or anticoagulant therapy: British Society of Gastroenterology (BSG) and European Society of Gastrointestinal Endoscopy (ESGE) guideline update. Gut. 2021 Sep;70(9):1611-28. https://www.bsg.org.uk/wp-content/uploads/2021/08/BSG_ESGE-antiplatelet-and-anticoagulant-update-2021.pdf http://www.ncbi.nlm.nih.gov/pubmed/34362780?tool=bestpractice.com
As soon as possible after 7 days of anticoagulant interruption in patients with low thrombotic risk
Preferably within 3 days of anticoagulant interruption in patients with high thrombotic risk, with heparin bridging.
If the patient is taking aspirin, other non-steroidal anti-inflammatory drugs (including cyclooxygenase-2 [COX-2] inhibitors), or dual antiplatelet therapy:
In general, continue aspirin in the acute phase, if your patient is taking this for secondary prevention.[31]Siau K, Hearnshaw S, Stanley AJ, et al. British Society of Gastroenterology (BSG)-led multisociety consensus care bundle for the early clinical management of acute upper gastrointestinal bleeding. Frontline Gastroenterol. 2020 Mar 27;11(4):311-23. https://www.bsg.org.uk/wp-content/uploads/2019/11/flgastro-2019-101395.pdf http://www.ncbi.nlm.nih.gov/pubmed/32582423?tool=bestpractice.com [33]National Institute for Health and Care Excellence. Acute upper gastrointestinal bleeding in over 16s: management. August 2016 [internet publication]. https://www.nice.org.uk/guidance/cg141 [64]Veitch AM, Radaelli F, Alikhan R, et al. Endoscopy in patients on antiplatelet or anticoagulant therapy: British Society of Gastroenterology (BSG) and European Society of Gastrointestinal Endoscopy (ESGE) guideline update. Gut. 2021 Sep;70(9):1611-28. https://www.bsg.org.uk/wp-content/uploads/2021/08/BSG_ESGE-antiplatelet-and-anticoagulant-update-2021.pdf http://www.ncbi.nlm.nih.gov/pubmed/34362780?tool=bestpractice.com
Consider seeking urgent advice from a specialist if there is major haemorrhage.
NICE doesn’t make a specific recommendation about major haemorrhage, but advises continuing aspirin only once haemostasis has been achieved.[33]National Institute for Health and Care Excellence. Acute upper gastrointestinal bleeding in over 16s: management. August 2016 [internet publication]. https://www.nice.org.uk/guidance/cg141
The consensus care bundle for acute upper gastrointestinal bleeding led by the BSG and the 2021 update to the BSG and ESGE guideline on endoscopy in patients on antiplatelet or anticoagulant therapy recommend continuing aspirin if this is taken as part of dual antiplatelet therapy with a P2Y12 inhibitor (e.g., clopidogrel, prasugrel, ticagrelor), and the P2Y12 is temporarily stopped.[31]Siau K, Hearnshaw S, Stanley AJ, et al. British Society of Gastroenterology (BSG)-led multisociety consensus care bundle for the early clinical management of acute upper gastrointestinal bleeding. Frontline Gastroenterol. 2020 Mar 27;11(4):311-23. https://www.bsg.org.uk/wp-content/uploads/2019/11/flgastro-2019-101395.pdf http://www.ncbi.nlm.nih.gov/pubmed/32582423?tool=bestpractice.com [64]Veitch AM, Radaelli F, Alikhan R, et al. Endoscopy in patients on antiplatelet or anticoagulant therapy: British Society of Gastroenterology (BSG) and European Society of Gastrointestinal Endoscopy (ESGE) guideline update. Gut. 2021 Sep;70(9):1611-28. https://www.bsg.org.uk/wp-content/uploads/2021/08/BSG_ESGE-antiplatelet-and-anticoagulant-update-2021.pdf http://www.ncbi.nlm.nih.gov/pubmed/34362780?tool=bestpractice.com
The 2021 update to the BSG and ESGE guideline recommends that, if aspirin is stopped, it should be restarted as soon as haemostasis is achieved or there is no further evidence of haemorrhage.[31]Siau K, Hearnshaw S, Stanley AJ, et al. British Society of Gastroenterology (BSG)-led multisociety consensus care bundle for the early clinical management of acute upper gastrointestinal bleeding. Frontline Gastroenterol. 2020 Mar 27;11(4):311-23. https://www.bsg.org.uk/wp-content/uploads/2019/11/flgastro-2019-101395.pdf http://www.ncbi.nlm.nih.gov/pubmed/32582423?tool=bestpractice.com [64]Veitch AM, Radaelli F, Alikhan R, et al. Endoscopy in patients on antiplatelet or anticoagulant therapy: British Society of Gastroenterology (BSG) and European Society of Gastrointestinal Endoscopy (ESGE) guideline update. Gut. 2021 Sep;70(9):1611-28. https://www.bsg.org.uk/wp-content/uploads/2021/08/BSG_ESGE-antiplatelet-and-anticoagulant-update-2021.pdf http://www.ncbi.nlm.nih.gov/pubmed/34362780?tool=bestpractice.com
The BSG care bundle cites two studies that demonstrate a three-fold increase in the risk of cardiovascular or cerebrovascular events if aspirin, prescribed for the secondary prevention, is discontinued.[31]Siau K, Hearnshaw S, Stanley AJ, et al. British Society of Gastroenterology (BSG)-led multisociety consensus care bundle for the early clinical management of acute upper gastrointestinal bleeding. Frontline Gastroenterol. 2020 Mar 27;11(4):311-23. https://www.bsg.org.uk/wp-content/uploads/2019/11/flgastro-2019-101395.pdf http://www.ncbi.nlm.nih.gov/pubmed/32582423?tool=bestpractice.com [66]Biondi-Zoccai GG, Lotrionte M, Agostoni P, et al. A systematic review and meta-analysis on the hazards of discontinuing or not adhering to aspirin among 50,279 patients at risk for coronary artery disease. Eur Heart J. 2006 Nov;27(22):2667-74. https://academic.oup.com/eurheartj/article/27/22/2667/2887446 http://www.ncbi.nlm.nih.gov/pubmed/17053008?tool=bestpractice.com [67]Maulaz AB, Bezerra DC, Michel P, et al. Effect of discontinuing aspirin therapy on the risk of brain ischemic stroke. Arch Neurol. 2005 Aug;62(8):1217-20. https://jamanetwork.com/journals/jamaneurology/fullarticle/789195 http://www.ncbi.nlm.nih.gov/pubmed/16087761?tool=bestpractice.com
The 2021 update to the BSG and ESGE guideline recommends considering permanently discontinuing aspirin if the patient is taking it for primary prevention.[64]Veitch AM, Radaelli F, Alikhan R, et al. Endoscopy in patients on antiplatelet or anticoagulant therapy: British Society of Gastroenterology (BSG) and European Society of Gastrointestinal Endoscopy (ESGE) guideline update. Gut. 2021 Sep;70(9):1611-28. https://www.bsg.org.uk/wp-content/uploads/2021/08/BSG_ESGE-antiplatelet-and-anticoagulant-update-2021.pdf http://www.ncbi.nlm.nih.gov/pubmed/34362780?tool=bestpractice.com
If the patient is taking any other non-steroidal anti-inflammatory drugs (including COX-2 inhibitors), NICE recommends stopping these during the acute phase.[31]Siau K, Hearnshaw S, Stanley AJ, et al. British Society of Gastroenterology (BSG)-led multisociety consensus care bundle for the early clinical management of acute upper gastrointestinal bleeding. Frontline Gastroenterol. 2020 Mar 27;11(4):311-23. https://www.bsg.org.uk/wp-content/uploads/2019/11/flgastro-2019-101395.pdf http://www.ncbi.nlm.nih.gov/pubmed/32582423?tool=bestpractice.com
If the patient is taking dual antiplatelet therapy, seek advice from the appropriate specialist to weigh up the benefits and risks of continuing the P2Y12 inhibitor. Discuss the balance of benefits versus risk with your patient. In general, if the patient:[31]Siau K, Hearnshaw S, Stanley AJ, et al. British Society of Gastroenterology (BSG)-led multisociety consensus care bundle for the early clinical management of acute upper gastrointestinal bleeding. Frontline Gastroenterol. 2020 Mar 27;11(4):311-23. https://www.bsg.org.uk/wp-content/uploads/2019/11/flgastro-2019-101395.pdf http://www.ncbi.nlm.nih.gov/pubmed/32582423?tool=bestpractice.com
Does not have coronary artery stents, the P2Y12 inhibitor should be stopped temporarily until haemostasis is achieved
Does have coronary artery stents, dual antiplatelet therapy should ideally be continued due to the high risk of stent thrombosis. However, the risks and benefits of doing so need to be carefully considered by a specialist.
blood transfusion
Additional treatment recommended for SOME patients in selected patient group
If the patient has massive bleeding, transfuse with blood, platelets, and clotting factors in line with your local protocols.[33]National Institute for Health and Care Excellence. Acute upper gastrointestinal bleeding in over 16s: management. August 2016 [internet publication]. https://www.nice.org.uk/guidance/cg141
Base decisions on blood transfusion on the full clinical picture; bear in mind that overtransfusion may be as damaging as under-transfusion.[33]National Institute for Health and Care Excellence. Acute upper gastrointestinal bleeding in over 16s: management. August 2016 [internet publication]. https://www.nice.org.uk/guidance/cg141
The British Society of Gastroenterology consensus care bundle recommends to consider a higher trigger for transfusion than Hb <70 g/L in patients with ischaemic heart disease or haemodynamic instability.[31]Siau K, Hearnshaw S, Stanley AJ, et al. British Society of Gastroenterology (BSG)-led multisociety consensus care bundle for the early clinical management of acute upper gastrointestinal bleeding. Frontline Gastroenterol. 2020 Mar 27;11(4):311-23. https://www.bsg.org.uk/wp-content/uploads/2019/11/flgastro-2019-101395.pdf http://www.ncbi.nlm.nih.gov/pubmed/32582423?tool=bestpractice.com
Give platelet transfusion to patients who are actively bleeding and have a platelet count of <50×109/L.[31]Siau K, Hearnshaw S, Stanley AJ, et al. British Society of Gastroenterology (BSG)-led multisociety consensus care bundle for the early clinical management of acute upper gastrointestinal bleeding. Frontline Gastroenterol. 2020 Mar 27;11(4):311-23. https://www.bsg.org.uk/wp-content/uploads/2019/11/flgastro-2019-101395.pdf http://www.ncbi.nlm.nih.gov/pubmed/32582423?tool=bestpractice.com [33]National Institute for Health and Care Excellence. Acute upper gastrointestinal bleeding in over 16s: management. August 2016 [internet publication]. https://www.nice.org.uk/guidance/cg141
Give fresh frozen plasma if the patient is actively bleeding and has a prothrombin time (or international normalised ratio) or activated partial thromboplastin time >1.5 times normal.[33]National Institute for Health and Care Excellence. Acute upper gastrointestinal bleeding in over 16s: management. August 2016 [internet publication]. https://www.nice.org.uk/guidance/cg141
Give cryoprecipitate if the patient has a fibrinogen level that remains <1.5 g/L despite fresh frozen plasma.[33]National Institute for Health and Care Excellence. Acute upper gastrointestinal bleeding in over 16s: management. August 2016 [internet publication]. https://www.nice.org.uk/guidance/cg141
In haemodynamically stable patients follow a restrictive transfusion protocol (trigger: Hb <70 g/L; target: 70-100 g/L).[31]Siau K, Hearnshaw S, Stanley AJ, et al. British Society of Gastroenterology (BSG)-led multisociety consensus care bundle for the early clinical management of acute upper gastrointestinal bleeding. Frontline Gastroenterol. 2020 Mar 27;11(4):311-23. https://www.bsg.org.uk/wp-content/uploads/2019/11/flgastro-2019-101395.pdf http://www.ncbi.nlm.nih.gov/pubmed/32582423?tool=bestpractice.com
Do not offer platelet transfusion if the patient is haemodynamically stable and not actively bleeding.[33]National Institute for Health and Care Excellence. Acute upper gastrointestinal bleeding in over 16s: management. August 2016 [internet publication]. https://www.nice.org.uk/guidance/cg141
anti-emetic
Additional treatment recommended for SOME patients in selected patient group
Follow your local protocols for the pre-endoscopy care of patients with active non-variceal upper gastrointestinal bleeding.
In practice, consider giving an anti-emetic for nausea and vomiting, which may be a cause or an aggravating factor in patients with MWT.
Primary options
cyclizine: 50 mg orally/intravenously three times daily
OR
promethazine: 25 mg orally every 6-8 hours when required
OR
ondansetron: 4-8 mg intravenously as a single dose
OR
prochlorperazine: 5-10 mg orally two to three times daily; 12.5 mg intramuscularly every 6 hours when required
These drug options and doses relate to a patient with no comorbidities.
Primary options
cyclizine: 50 mg orally/intravenously three times daily
OR
promethazine: 25 mg orally every 6-8 hours when required
OR
ondansetron: 4-8 mg intravenously as a single dose
OR
prochlorperazine: 5-10 mg orally two to three times daily; 12.5 mg intramuscularly every 6 hours when required
Drug choice, dose and interactions may be affected by the patient's comorbidities. Check your local drug formulary.
Show drug information for a patient with no comorbidities
Primary options
cyclizine
OR
promethazine
OR
ondansetron
OR
prochlorperazine
Plus – diagnostic endoscopy with or without endoscopic treatment
diagnostic endoscopy with or without endoscopic treatment
Treatment recommended for ALL patients in selected patient group
Following the risk assessment, consider patients with a Glasgow-Blatchford score ≤1 for outpatient management, in line with recommendations from the British Society of Gastroenterology (BSG) and the European Society of Gastrointestinal Endoscopy (ESGE).[31]Siau K, Hearnshaw S, Stanley AJ, et al. British Society of Gastroenterology (BSG)-led multisociety consensus care bundle for the early clinical management of acute upper gastrointestinal bleeding. Frontline Gastroenterol. 2020 Mar 27;11(4):311-23. https://www.bsg.org.uk/wp-content/uploads/2019/11/flgastro-2019-101395.pdf http://www.ncbi.nlm.nih.gov/pubmed/32582423?tool=bestpractice.com [32]Gralnek IM, Stanley AJ, Morris AJ, et al. Endoscopic diagnosis and management of nonvariceal upper gastrointestinal hemorrhage (NVUGIH): European Society of Gastrointestinal Endoscopy (ESGE) guideline - update 2021. Endoscopy. 2021 Mar;53(3):300-32. https://www.thieme-connect.com/products/ejournals/html/10.1055/a-1369-5274 http://www.ncbi.nlm.nih.gov/pubmed/33567467?tool=bestpractice.com See Risk stratification under Diagnosis recommendations.
Refer all patients with suspected acute upper gastrointestinal (GI) bleeding for upper GI endoscopy (i.e., gastroscopy).[31]Siau K, Hearnshaw S, Stanley AJ, et al. British Society of Gastroenterology (BSG)-led multisociety consensus care bundle for the early clinical management of acute upper gastrointestinal bleeding. Frontline Gastroenterol. 2020 Mar 27;11(4):311-23. https://www.bsg.org.uk/wp-content/uploads/2019/11/flgastro-2019-101395.pdf http://www.ncbi.nlm.nih.gov/pubmed/32582423?tool=bestpractice.com [32]Gralnek IM, Stanley AJ, Morris AJ, et al. Endoscopic diagnosis and management of nonvariceal upper gastrointestinal hemorrhage (NVUGIH): European Society of Gastrointestinal Endoscopy (ESGE) guideline - update 2021. Endoscopy. 2021 Mar;53(3):300-32. https://www.thieme-connect.com/products/ejournals/html/10.1055/a-1369-5274 http://www.ncbi.nlm.nih.gov/pubmed/33567467?tool=bestpractice.com [33]National Institute for Health and Care Excellence. Acute upper gastrointestinal bleeding in over 16s: management. August 2016 [internet publication]. https://www.nice.org.uk/guidance/cg141 Follow your local protocol for recommendations on the optimal timing of the procedure for your patient. Guidelines from the National Institute for Health and Care Excellence (NICE) and the ESGE, and a consensus care bundle led by the BSG, agree that endoscopy should always be performed early (i.e., within 24 hours of presentation) with suspected acute upper GI bleed. However, the exact timing of the procedure within the 24-hour period is controversial, and specific recommendations from NICE, the BSG, and the ESGE differ as follows.
The ESGE recommends early (≤24 hours from presentation) upper GI endoscopy following haemodynamic resuscitation. The ESGE does not recommend urgent (defined by the ESGE as ≤12 hours from presentation) endoscopy.[32]Gralnek IM, Stanley AJ, Morris AJ, et al. Endoscopic diagnosis and management of nonvariceal upper gastrointestinal hemorrhage (NVUGIH): European Society of Gastrointestinal Endoscopy (ESGE) guideline - update 2021. Endoscopy. 2021 Mar;53(3):300-32. https://www.thieme-connect.com/products/ejournals/html/10.1055/a-1369-5274 http://www.ncbi.nlm.nih.gov/pubmed/33567467?tool=bestpractice.com
NICE and the BSG care bundle recommend:[31]Siau K, Hearnshaw S, Stanley AJ, et al. British Society of Gastroenterology (BSG)-led multisociety consensus care bundle for the early clinical management of acute upper gastrointestinal bleeding. Frontline Gastroenterol. 2020 Mar 27;11(4):311-23. https://www.bsg.org.uk/wp-content/uploads/2019/11/flgastro-2019-101395.pdf http://www.ncbi.nlm.nih.gov/pubmed/32582423?tool=bestpractice.com [33]National Institute for Health and Care Excellence. Acute upper gastrointestinal bleeding in over 16s: management. August 2016 [internet publication]. https://www.nice.org.uk/guidance/cg141
Urgent endoscopy, immediately after resuscitation, if the patient is unstable with severe acute upper GI bleeding
Endoscopy within 24 hours of admission for all other patients with upper GI bleeding.
Practical tip
Ensure that haemodynamically unstable patients are adequately resuscitated before undergoing diagnostic endoscopy.
For more on diagnostic endoscopy, see Imaging under Diagnosis recommendations.
After the endoscopy, review the endoscopy report and instructions from the endoscopist on the ward.[32]Gralnek IM, Stanley AJ, Morris AJ, et al. Endoscopic diagnosis and management of nonvariceal upper gastrointestinal hemorrhage (NVUGIH): European Society of Gastrointestinal Endoscopy (ESGE) guideline - update 2021. Endoscopy. 2021 Mar;53(3):300-32. https://www.thieme-connect.com/products/ejournals/html/10.1055/a-1369-5274 http://www.ncbi.nlm.nih.gov/pubmed/33567467?tool=bestpractice.com
Once the haemorrhage is confirmed by endoscopy, refer the patient to a gastroenterology service for endoscopic treatment.[31]Siau K, Hearnshaw S, Stanley AJ, et al. British Society of Gastroenterology (BSG)-led multisociety consensus care bundle for the early clinical management of acute upper gastrointestinal bleeding. Frontline Gastroenterol. 2020 Mar 27;11(4):311-23. https://www.bsg.org.uk/wp-content/uploads/2019/11/flgastro-2019-101395.pdf http://www.ncbi.nlm.nih.gov/pubmed/32582423?tool=bestpractice.com [33]National Institute for Health and Care Excellence. Acute upper gastrointestinal bleeding in over 16s: management. August 2016 [internet publication]. https://www.nice.org.uk/guidance/cg141
Endoscopic techniques are specialised and should only be undertaken by someone with adequate training and experience.
NICE recommends using one of the following methods for the endoscopic treatment of non-variceal upper gastrointestinal bleeding:[33]National Institute for Health and Care Excellence. Acute upper gastrointestinal bleeding in over 16s: management. August 2016 [internet publication]. https://www.nice.org.uk/guidance/cg141
A mechanical method (e.g., clips) with or without adrenaline (epinephrine)
Thermal coagulation with adrenaline
Fibrin or thrombin with adrenaline.
Do not use adrenaline as monotherapy for endoscopic treatment.[33]National Institute for Health and Care Excellence. Acute upper gastrointestinal bleeding in over 16s: management. August 2016 [internet publication]. https://www.nice.org.uk/guidance/cg141
Practical tip
Do not give proton-pump inhibitors pre-endoscopy. This is in line with recommendations from NICE guidelines and a consensus care bundle for acute upper GI bleeding led by the BSG.[31]Siau K, Hearnshaw S, Stanley AJ, et al. British Society of Gastroenterology (BSG)-led multisociety consensus care bundle for the early clinical management of acute upper gastrointestinal bleeding. Frontline Gastroenterol. 2020 Mar 27;11(4):311-23. https://www.bsg.org.uk/wp-content/uploads/2019/11/flgastro-2019-101395.pdf http://www.ncbi.nlm.nih.gov/pubmed/32582423?tool=bestpractice.com [33]National Institute for Health and Care Excellence. Acute upper gastrointestinal bleeding in over 16s: management. August 2016 [internet publication]. https://www.nice.org.uk/guidance/cg141 NICE does not recommend the use of H2 antagonists before endoscopy.[33]National Institute for Health and Care Excellence. Acute upper gastrointestinal bleeding in over 16s: management. August 2016 [internet publication]. https://www.nice.org.uk/guidance/cg141
More info: Approaches to endoscopic treatment of non-variceal upper GI bleeding
Accepted endoscopic modalities include the following.
Injection therapy
This is commonly used in the treatment of ulceration causing upper GI bleeding, in combination with thermal or mechanical therapy, or with fibrin or thrombin. Its role in the management of MWT bleeding has been studied in a small series.[69]Peng YC, Tung CF, Chow WK, et al. Efficacy of endoscopic isotonic saline-epinephrine injection for the management of active Mallory-Weiss tears. J Clin Gastroenterol. 2001 Feb;32(2):119-22. http://www.ncbi.nlm.nih.gov/pubmed/11205645?tool=bestpractice.com [70]Chau CH, Siu WT, Law BK, et al. Randomized controlled trial comparing epinephrine injection plus heat probe coagulation versus epinephrine injection plus argon plasma coagulation for bleeding peptic ulcers. Gastrointest Endosc. 2003 Apr;57(4):455-61. http://www.ncbi.nlm.nih.gov/pubmed/12665753?tool=bestpractice.com
Aliquots ranging from 0.5 to 20 mL are injected around or into the bleeding point.
Haemoclip placement, alone or in combination with adrenaline injection
This is as safe and effective as other methods for controlling actively bleeding lesions.[71]Yuan Y, Wang C, Hunt RH. Endoscopic clipping for acute nonvariceal upper-GI bleeding: a meta-analysis and critical appraisal of randomized controlled trials. Gastrointest Endosc. 2008 Aug;68(2):339-51. http://www.ncbi.nlm.nih.gov/pubmed/18656600?tool=bestpractice.com [72]Sung JJ, Tsoi KK, Lai LH, et al. Endoscopic clipping versus injection and thermo-coagulation in the treatment of non-variceal upper gastrointestinal bleeding: a meta-analysis. Gut. 2007 Oct;56(10):1364-73. https://www.ncbi.nlm.nih.gov/labs/pmc/articles/PMC2000277 http://www.ncbi.nlm.nih.gov/pubmed/17566018?tool=bestpractice.com [73]Guo SB, Gong AX, Leng J, et al. Application of endoscopic hemoclips for nonvariceal bleeding in the upper gastrointestinal tract. Worl J Gastroentererol. 2009 Sep 14;15(34):4322-6. https://www.ncbi.nlm.nih.gov/labs/pmc/articles/PMC2744190 http://www.ncbi.nlm.nih.gov/pubmed/19750577?tool=bestpractice.com
Thermal coagulation
This includes multipolar electrocoagulation, heater probe, and argon plasma coagulation. Thermal coagulation is safe and often successful when given by experienced operators.[74]Laine L. Multipolar electrocoagulation in the treatment of active upper gastrointestinal tract hemorrhage. A prospective controlled trial. N Engl J Med. 1987 Jun 25;316(26):1613-7. http://www.ncbi.nlm.nih.gov/pubmed/3295547?tool=bestpractice.com [75]Papp JP. Electrocoagulation of actively bleeding Mallory-Weiss tears. Gastrointest Endosc. 1980 Nov;26(4):128-30. http://www.ncbi.nlm.nih.gov/pubmed/7450460?tool=bestpractice.com
Mechanical therapy
Endoscopic band ligation (EBL) for MWT has been described in case reports and small randomised controlled trials. The mechanism is similar to that described for variceal band ligation: the affected mucosa is suctioned into the ligating cup device, after which a rubber band is deployed. EBL is simple and safe.[76]Matsui S, Kamisako T, Kudo M, et al. Endoscopic band ligation for control of nonvariceal upper GI hemorrhage: comparison with bipolar electrocoagulation. Gastrointest Endosc. 2002 Feb;55(2):214-8. http://www.ncbi.nlm.nih.gov/pubmed/11818925?tool=bestpractice.com [77]Cho YS, Chae HS, Kim HK, et al. Endoscopic band ligation and endoscopic hemoclip placement for patients with Mallory-Weiss syndrome and active bleeding. World J Gastroenterol. 2008 Apr 7;14(13):2080-4. https://www.ncbi.nlm.nih.gov/labs/pmc/articles/PMC2701530 http://www.ncbi.nlm.nih.gov/pubmed/18395910?tool=bestpractice.com [78]Ertekin C, Taviloglu K, Barbaros U, et al. Endoscopic band ligation: alternative treatment method in nonvariceal upper gastrointestinal hemorrhage. J Laparoendosc Adv Surg Tech A. 2002 Feb;12(1):41-5. http://www.ncbi.nlm.nih.gov/pubmed/11905861?tool=bestpractice.com In most cases, EBL is used as a single therapy in which the bleeding point is aspirated and ligated. In practice, EBL may be considered as a treatment option in patients with uncontrollable bleeding from MWT.
Cap-mounted clips are recommended by the ESGE guidelines in patients with persistent bleeding despite standard endoscopic treatments.[32]Gralnek IM, Stanley AJ, Morris AJ, et al. Endoscopic diagnosis and management of nonvariceal upper gastrointestinal hemorrhage (NVUGIH): European Society of Gastrointestinal Endoscopy (ESGE) guideline - update 2021. Endoscopy. 2021 Mar;53(3):300-32. https://www.thieme-connect.com/products/ejournals/html/10.1055/a-1369-5274 http://www.ncbi.nlm.nih.gov/pubmed/33567467?tool=bestpractice.com Persistent bleeding is defined as ongoing active bleeding refractory to standard haemostasis modalities.[32]Gralnek IM, Stanley AJ, Morris AJ, et al. Endoscopic diagnosis and management of nonvariceal upper gastrointestinal hemorrhage (NVUGIH): European Society of Gastrointestinal Endoscopy (ESGE) guideline - update 2021. Endoscopy. 2021 Mar;53(3):300-32. https://www.thieme-connect.com/products/ejournals/html/10.1055/a-1369-5274 http://www.ncbi.nlm.nih.gov/pubmed/33567467?tool=bestpractice.com
Topical therapy
A topical hemostatic spray/powder is recommended by the ESGE for patients with persistent bleeding despite standard endoscopic treatments.[32]Gralnek IM, Stanley AJ, Morris AJ, et al. Endoscopic diagnosis and management of nonvariceal upper gastrointestinal hemorrhage (NVUGIH): European Society of Gastrointestinal Endoscopy (ESGE) guideline - update 2021. Endoscopy. 2021 Mar;53(3):300-32. https://www.thieme-connect.com/products/ejournals/html/10.1055/a-1369-5274 http://www.ncbi.nlm.nih.gov/pubmed/33567467?tool=bestpractice.com
[Figure caption and citation for the preceding image starts]: Mallory-Weiss tear after adrenaline injection (the bleeding has stopped, allowing better visualisation of the lesion)From the collection of Juan Carlos Munoz, MD, University of Florida [Citation ends].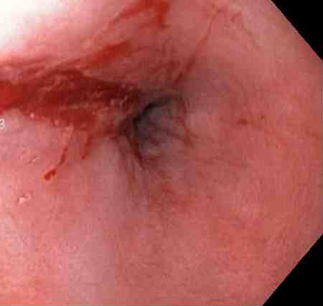 [Figure caption and citation for the preceding image starts]: Adrenaline 1:10,000 is injected intravenously next to Mallory-Weiss tearFrom the collection of Juan Carlos Munoz, MD, University of Florida [Citation ends].
[Figure caption and citation for the preceding image starts]: Adrenaline 1:10,000 is injected intravenously next to Mallory-Weiss tearFrom the collection of Juan Carlos Munoz, MD, University of Florida [Citation ends].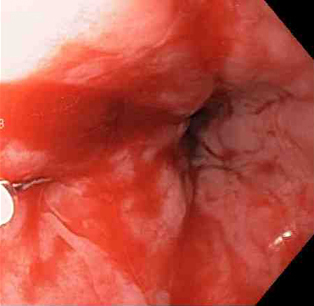 [Figure caption and citation for the preceding image starts]: Actively bleeding tear appears as a red longitudinal defect with normal surrounding mucosaFrom the collection of Juan Carlos Munoz, MD, University of Florida [Citation ends].
[Figure caption and citation for the preceding image starts]: Actively bleeding tear appears as a red longitudinal defect with normal surrounding mucosaFrom the collection of Juan Carlos Munoz, MD, University of Florida [Citation ends].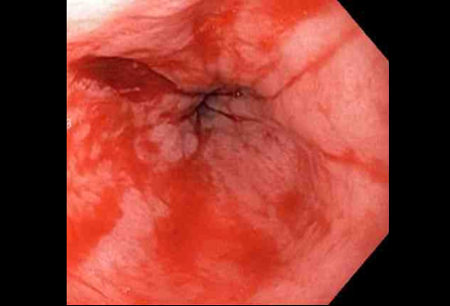 [Figure caption and citation for the preceding image starts]: A haemoclip deployed in the centre of the lesion (no previous adrenaline was infused in this case)From the collection of Juan Carlos Munoz, MD, University of Florida [Citation ends].
[Figure caption and citation for the preceding image starts]: A haemoclip deployed in the centre of the lesion (no previous adrenaline was infused in this case)From the collection of Juan Carlos Munoz, MD, University of Florida [Citation ends].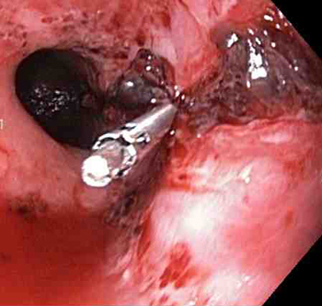 [Figure caption and citation for the preceding image starts]: Non-bleeding adherent clotFrom the collection of Juan Carlos Munoz, MD, University of Florida [Citation ends].
[Figure caption and citation for the preceding image starts]: Non-bleeding adherent clotFrom the collection of Juan Carlos Munoz, MD, University of Florida [Citation ends].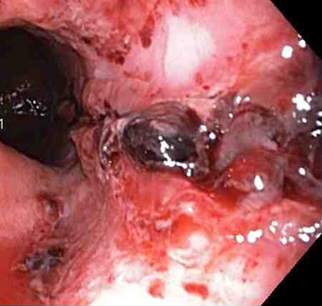 [Figure caption and citation for the preceding image starts]: Three haemoclips deployed to complete closure of the mucosal defectFrom the collection of Juan Carlos Munoz, MD, University of Florida [Citation ends].
[Figure caption and citation for the preceding image starts]: Three haemoclips deployed to complete closure of the mucosal defectFrom the collection of Juan Carlos Munoz, MD, University of Florida [Citation ends].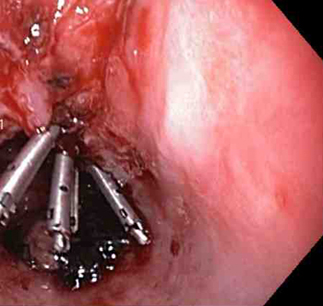
proton-pump inhibitor
Additional treatment recommended for SOME patients in selected patient group
The National Institute for Health and Care Excellence (NICE) in the UK recommends giving a proton-pump inhibitor (PPI) post-endoscopy to patients with stigmata (a visible vessel and adherent blood clot) of recent haemorrhage shown on endoscopy; however, NICE does not make a specific recommendation on the preferred route of administration or dose.[33]National Institute for Health and Care Excellence. Acute upper gastrointestinal bleeding in over 16s: management. August 2016 [internet publication]. https://www.nice.org.uk/guidance/cg141
Note that the European Society of Gastrointestinal Endoscopy recommends high-dose PPI post-endoscopy for all patients who receive endoscopic treatments.[32]Gralnek IM, Stanley AJ, Morris AJ, et al. Endoscopic diagnosis and management of nonvariceal upper gastrointestinal hemorrhage (NVUGIH): European Society of Gastrointestinal Endoscopy (ESGE) guideline - update 2021. Endoscopy. 2021 Mar;53(3):300-32. https://www.thieme-connect.com/products/ejournals/html/10.1055/a-1369-5274 http://www.ncbi.nlm.nih.gov/pubmed/33567467?tool=bestpractice.com
Primary options
omeprazole: 80 mg intravenously initially over 40-60 minutes, followed by 8 mg/hour intravenous infusion for 72 hours, then switch to oral therapy
More omeprazoleAlternative dose regimens may be recommended; consult a specialist for further guidance on dose.
OR
esomeprazole: 80 mg intravenously initially over 30 minutes, followed by 8 mg/hour intravenous infusion for 72 hours, then switch to oral therapy
More esomeprazoleAlternative dose regimens may be recommended; consult a specialist for further guidance on dose.
These drug options and doses relate to a patient with no comorbidities.
Primary options
omeprazole: 80 mg intravenously initially over 40-60 minutes, followed by 8 mg/hour intravenous infusion for 72 hours, then switch to oral therapy
More omeprazoleAlternative dose regimens may be recommended; consult a specialist for further guidance on dose.
OR
esomeprazole: 80 mg intravenously initially over 30 minutes, followed by 8 mg/hour intravenous infusion for 72 hours, then switch to oral therapy
More esomeprazoleAlternative dose regimens may be recommended; consult a specialist for further guidance on dose.
Drug choice, dose and interactions may be affected by the patient's comorbidities. Check your local drug formulary.
Show drug information for a patient with no comorbidities
Primary options
omeprazole
OR
esomeprazole
emergency surgery or radiological intervention
Additional treatment recommended for SOME patients in selected patient group
Patients who rebleed after endoscopic and medical treatments may need emergency surgery or interventional radiology to control the bleeding.[32]Gralnek IM, Stanley AJ, Morris AJ, et al. Endoscopic diagnosis and management of nonvariceal upper gastrointestinal hemorrhage (NVUGIH): European Society of Gastrointestinal Endoscopy (ESGE) guideline - update 2021. Endoscopy. 2021 Mar;53(3):300-32. https://www.thieme-connect.com/products/ejournals/html/10.1055/a-1369-5274 http://www.ncbi.nlm.nih.gov/pubmed/33567467?tool=bestpractice.com [33]National Institute for Health and Care Excellence. Acute upper gastrointestinal bleeding in over 16s: management. August 2016 [internet publication]. https://www.nice.org.uk/guidance/cg141
In patients who rebleed after first or failed endoscopic treatment, or are at high risk of rebleeding after endoscopic treatment, guidelines from the National Institute for Health and Care Excellence in the UK recommend:[33]National Institute for Health and Care Excellence. Acute upper gastrointestinal bleeding in over 16s: management. August 2016 [internet publication]. https://www.nice.org.uk/guidance/cg141
Repeat endoscopy for patients who rebleed with a view to perform further endoscopic treatment or emergency surgery
Interventional radiology for unstable patients who rebleed after endoscopic treatment. Refer the patient urgently for surgery if interventional radiology is not promptly available
Repeat endoscopy, with treatment as appropriate, for all patients at high risk of rebleeding, particularly if there is doubt about adequate haemostasis at the first endoscopy.
[Figure caption and citation for the preceding image starts]: 56-year-old female had a gastroscopy for upper GI bleeding 5 days prior treated with a single clip. She continued having melaena and low Hb for the following 5 days after initial procedure. A second gastroscopy detected a longitudinal gastric laceration without perforation on the corpus to cardiaFrom the collection of Juan Carlos Munoz, MD, University of Florida [Citation ends].
[Figure caption and citation for the preceding image starts]: Diagnosed as a gastric tear without perforation from previous gastroscopy evaluation. Managed with application of haemoclips and emergency surgical consultFrom the collection of Juan Carlos Munoz, MD, University of Florida [Citation ends].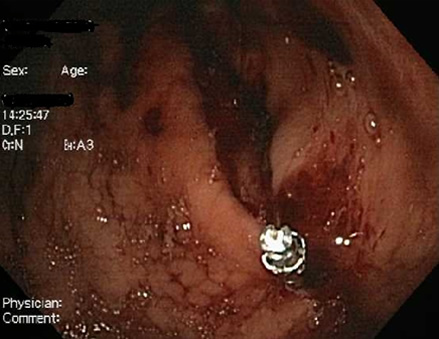 [Figure caption and citation for the preceding image starts]: A total of seven haemoclips were appliedFrom the collection of Juan Carlos Munoz, MD, University of Florida [Citation ends].
[Figure caption and citation for the preceding image starts]: A total of seven haemoclips were appliedFrom the collection of Juan Carlos Munoz, MD, University of Florida [Citation ends].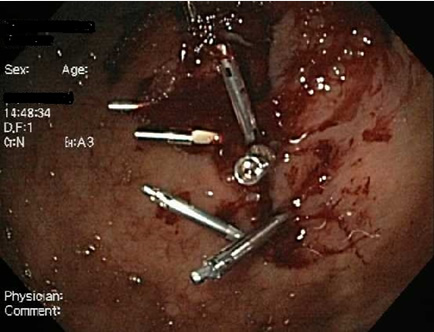 [Figure caption and citation for the preceding image starts]: 16 days later, the tear has closedFrom the collection of Juan Carlos Munoz, MD, University of Florida [Citation ends].
[Figure caption and citation for the preceding image starts]: 16 days later, the tear has closedFrom the collection of Juan Carlos Munoz, MD, University of Florida [Citation ends].

Choose a patient group to see our recommendations
Please note that formulations/routes and doses may differ between drug names and brands, drug formularies, or locations. Treatment recommendations are specific to patient groups. See disclaimer
Use of this content is subject to our disclaimer
