Tests
1st tests to order
CBC with differential
Test
Leukocytosis ranges from 12,000 to 18,000 cells/mm³.
Eosinophilia ranges from 1000 to 3000 cells/mm³, but can be as high as 8000 cells/mm³.[2]
Eosinophils make up 10% to 50% of the leukocytosis.
The degree of eosinophilia correlates with the number of adult worms causing the infection, and consequently with the number of newborn larvae entering the blood.[2] A low eosinophil count is a rare finding and, along with a sudden drop in the eosinophil count, constitutes a poor prognostic sign that may be associated with death.[46][53]
Result
leukocytosis, eosinophilia
creatine kinase and other muscle enzymes
serum potassium
Test
Hypokalemia is a frequent finding.[54]
Result
reduced
serum albumin
Test
Hypoalbuminemia is a frequent finding and results in an increase of extracellular water content and subsequent edema.[2]
Result
reduced
serum IgE
Test
Highly elevated.
It has been speculated that the increase in IgE represents a protective reaction on the part of the human host.[55]
Result
elevated
Tests to consider
antibody serology
Test
The simplest method for confirming the diagnosis of trichinellosis.[34][56]
The International Commission on Trichinellosis recommends the ELISA method using excretory/secretory antigens of the muscle larvae, for screening purposes.[57][58] Usually positive in the systemic (parenteral) phase of the disease and by the time clinical symptoms develop, and may remain positive for years.[54]
May occasionally be negative during the systemic phase, but if there is a strong clinical suspicion of trichinellosis, serology should be repeated as the phenomenon of seroconversion is of great diagnostic value.
Positive results obtained by ELISA should be confirmed with Western blot.[57]
Result
positive
muscle biopsy
Test
Less frequently used technique in clinical practice.[34] Sensitivity is greatest 4 weeks after infection, when the majority of patients are experiencing an improvement in symptoms. Therefore, it may not be ethically justifiable to undertake such an invasive procedure at this time.
Biopsy samples are obtained from the deltoid muscle and examined by pressing between 2 slides, digesting using 1% HCl-1% pepsin (thus releasing larvae from the muscle), or by regular histopathologic inspection for the detection of larvae.[2]
If performed too early in the systemic phase, the result may be negative.
Useful for typing the Trichinella species and determining the larval muscular burden.[Figure caption and citation for the preceding image starts]: Larva of Trichinella spiralis in a muscle nurse cellFrom: Summary of Basic Science and Clinical Information section of The Trichinella Page (http://www.trichinella.org); used with permission from Dr Dickson Despommier [Citation ends]. [Figure caption and citation for the preceding image starts]: Trichinella spiralis cysts seen embedded in a muscle tissue specimen, in a case of trichinellosisCDC [Citation ends].
[Figure caption and citation for the preceding image starts]: Trichinella spiralis cysts seen embedded in a muscle tissue specimen, in a case of trichinellosisCDC [Citation ends].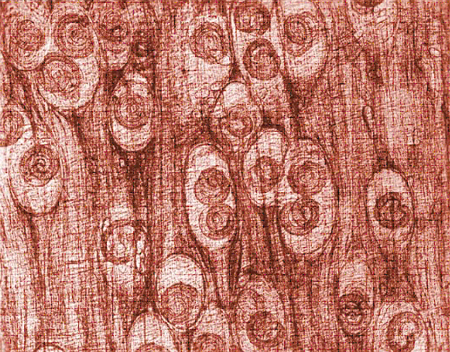
Result
larvae on microscopy
electromyography
Test
Increased contractibility of striated muscle can be detected using electromyography. However, the findings are nonspecific and seldom helpful in confirming the diagnosis of trichinellosis.
Electromyographic changes may persist for years after the initial infection.[59]
Result
decreased potential amplitude and interference of electrical conduction
urinalysis
Test
May be able to detect manifestations of tubular or glomerular compromise in severe cases, such as hematuria, proteinuria, and presence of casts.[63]
Result
normal; hematuria, proteinuria, and casts may be present
serum creatinine and creatinine clearance
Test
May identify renal failure in severe cases.[63]
Result
may be elevated
serum aminotransferases
Test
Occasionally elevated in patients with severe disease and liver compromise.[64]
Result
may be elevated
MRI or CT brain
Test
May be considered in suspected cases of neurotrichinellosis.
Due to their minute size and lack of calcification in the early stages of the disease, Trichinella larvae in the muscle cannot be detected by conventional radiology.
In neurotrichinellosis, small hypodense areas, most probably representing infarctions secondary to parasite-induced vasculitis, may be detected in the brain parenchyma on CT or MRI.[6][60]
Result
hypodensities in brain parenchyma
EEG
Test
Should be undertaken in suspected cases of trichinellosis complicated by encephalitis.
Trichinella myocarditis is characterized by several ECG changes, including nonspecific alteration of ventricular repolarization represented by ST-T wave abnormalities and arrhythmias (bundle-branch block or sinus tachycardia). Less commonly, other bradyarrhythmias and tachyarrhythmias, and low-voltage QRS complexes in the limb leads, are seen.[62]
Result
diffuse slowing of electrical activity
cerebrospinal fluid analysis
Test
In cases of central nervous system compromise, analysis of the cerebrospinal fluid may reveal mild elevations in lymphocytes, eosinophils, and/or protein.[61]
Result
may be abnormal
ECG
Test
Should be undertaken in suspected cases of trichinella myocarditis.
ST-T wave abnormalities represent nonspecific alteration of ventricular repolarization.
Less commonly, other bradyarrhythmias and tachyarrhythmias, and low-voltage QRS complexes in the limb leads, are seen.[62]
Result
ST-T wave abnormalities, arrhythmias (bundle-branch block or sinus tachycardia)
serum troponin
Test
May be a useful screening test in suspected cases of myocarditis.[66]
Result
elevated if myocarditis present
Two-dimensional echocardiography
Test
May identify features associated with myocarditis.[67]
Result
may demonstrate global or segmental ventricular hypokinesis, ventricular dilation, and pericardial effusions
Use of this content is subject to our disclaimer