Tests
1st tests to order
biopsy of the primary site
Test
Indicated if a primary lesion has been detected during examination. Base of tongue tumors require biopsy under general anesthesia. Tonsil tumors can be accessed with incisional biopsy in the office. The National Comprehensive Cancer Network (NCCN) recommends considering examination under anesthesia with biopsy confirmation for patients presenting with a p16-positive cervical lymph node prior to treatment decision-making.[2] Patients at high risk for general anesthesia and those who undergo a thorough examination including tongue base palpation, or those who require systemic therapy/radiation therapy and will not have their treatment plan affected regardless of surgical evaluation need not undergo examination under anesthesia.[2]
Result
assesses tumor histology characterized by atypical keratinocytes with pleomorphism, hyperchromatic nuclei, and mitosis invading the basement membrane; degree of differentiation varies from well, to moderate, to poorly differentiated
CT scan of the head and neck
Test
Tumor characteristics on CT scan are space-occupying growth with obliteration of fat planes, infiltration of muscles, bony destruction, and peripheral enhancement with intravenous contrast.[Figure caption and citation for the preceding image starts]: Large base of tongue tumor seen on axial CT scanFrom the collection of Dr Linda X. Yin; used with permission [Citation ends].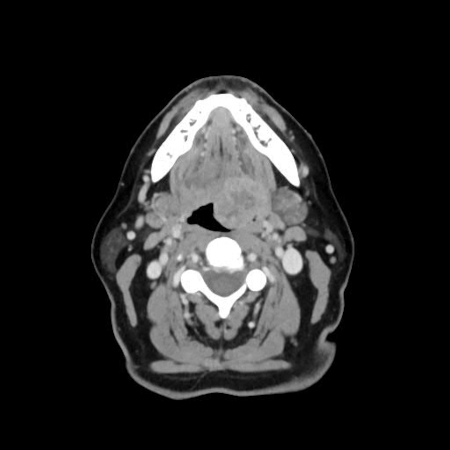
Lymph node enlargement (>1 cm) and central necrosis are indirect signs of malignancy.[42] However, small and superficial tumors may not be seen, and the presence of dental artifacts may obscure the tumor on CT scan.
Result
establish the location, size, and extent of the tumor
fine needle aspiration cytology (FNAC) of neck nodes
Test
If a suspicious neck node has been found, but no primary tumor is detected on examination, then the next step is FNAC of the node.[48] This may be guided by ultrasound to improve the accuracy of diagnosis.[49][50] Ultrasound guidance improves the accuracy of fine needle aspiration biopsies in oropharyngeal cancer, compared with palpation guidance.
Result
detects neck node metastases
in situ hybridization for human papillomavirus (HPV)-16, p16 immunohistochemistry, or PCR in biopsy specimen
Test
To identify HPV status, WHO recommends direct HPV testing (in situ hybridization and/or PCR based assays) or indirect testing (p16 immunohistochemical staining).[1][3][4] The National Comprehensive Cancer Network recommends that all patients with oropharyngeal cancer should undergo tumor HPV testing by p16 immunohistochemistry.[2] When using p16, the 70% cutoff with nuclear and cytoplasmic expression with at least moderate to strong intensity is recommended by NCCN.[2] The College of American Pathologists recommends testing all newly diagnosed patients with oropharyngeal squamous cell carcinoma for p16. In most cases of unknown primary metastatic to a level II or III lymph node, high-risk HPV and Epstein-Barr virus testing is also recommended.[2][51]
Result
HPV-associated cancers (HPV-positive): diffuse p16 expression (nuclear and cytoplasmic)
Tests to consider
MRI of the head and neck
PET-CT of the head and neck
Test
PET-CT fusion scan combines both physiologic and anatomic information from PET scan and CT scan, and further improves the accuracy of detecting distant metastases over either modality alone. Accuracy in detecting distant metastases is 94% with PET-CT, 90% with PET alone, and 74% with CT alone.[45] Because most oropharyngeal cancers are treated with radiation to preserve anatomic organs, PET-CT also improves the accuracy of planning radiation therapy treatment.[47] For these reasons, PET-CT is emerging as the preferred modality for staging of oropharyngeal cancer.It can also detect disease recurrence with a greater accuracy (90%) than conventional follow-up with clinical exam, endoscopy, CT, and MRI.[64][65][66] However, it is limited by difficulty distinguishing tumor from infection. It should be repeated 3 months after treatment to avoid false-positive results secondary to inflammation after treatment.[67][Figure caption and citation for the preceding image starts]: 74-year-old man with squamous cell carcinoma of the left tongue base extending into the hypopharynx. Fluorodeoxyglucose PET/CT images demonstrate focal increased metabolic activity in the left hypopharynx/tongue base (arrows)From the collection of Dr Fabio Almeida; used with permission [Citation ends].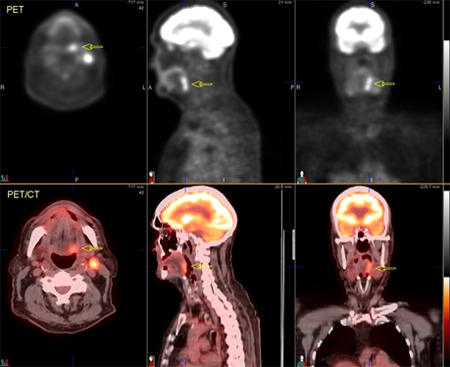 [Figure caption and citation for the preceding image starts]: 60-year-old man with squamous cell carcinoma of the right tongue base. Fluorodeoxyglucose PET/CT images demonstrate focal increased metabolic activity in the right tongue base, which extends inferior to the hypopharynx (arrows) and across the midline. On the CT images (top row), soft-tissue irregularity can be seen, but the margins of the tumor are difficult to defineFrom the collection of Dr Fabio Almeida; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: 60-year-old man with squamous cell carcinoma of the right tongue base. Fluorodeoxyglucose PET/CT images demonstrate focal increased metabolic activity in the right tongue base, which extends inferior to the hypopharynx (arrows) and across the midline. On the CT images (top row), soft-tissue irregularity can be seen, but the margins of the tumor are difficult to defineFrom the collection of Dr Fabio Almeida; used with permission [Citation ends].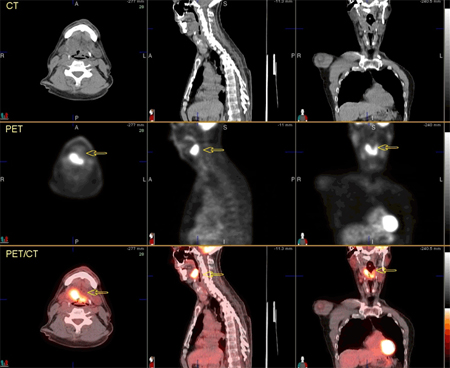 [Figure caption and citation for the preceding image starts]: 74-year-old man with squamous cell carcinoma of the left tongue base extending into the hypopharynx. Images after chemoradiation therapy, showing complete resolution of metabolic foci. Mild diffuse increased metabolism in the oropharyngeal region consistent with mild post-therapy inflammationFrom the collection of Dr Fabio Almeida; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: 74-year-old man with squamous cell carcinoma of the left tongue base extending into the hypopharynx. Images after chemoradiation therapy, showing complete resolution of metabolic foci. Mild diffuse increased metabolism in the oropharyngeal region consistent with mild post-therapy inflammationFrom the collection of Dr Fabio Almeida; used with permission [Citation ends]. [Figure caption and citation for the preceding image starts]: 60-year-old man with squamous cell carcinoma of the right tongue base. PET/CT images show mild increased metabolism in a mid right neck lymph node, of concern for metastatic involvement (arrows)From the collection of Dr Fabio Almeida; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: 60-year-old man with squamous cell carcinoma of the right tongue base. PET/CT images show mild increased metabolism in a mid right neck lymph node, of concern for metastatic involvement (arrows)From the collection of Dr Fabio Almeida; used with permission [Citation ends].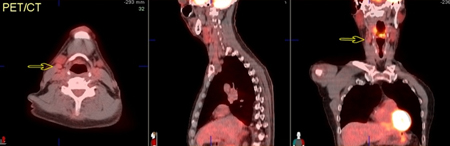 [Figure caption and citation for the preceding image starts]: 60-year-old man with squamous cell carcinoma of the right tongue base. Axial images further caudally show extent of tumor involvement in the hypopharynx including invasion through the hyoid boneFrom the collection of Dr Fabio Almeida; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: 60-year-old man with squamous cell carcinoma of the right tongue base. Axial images further caudally show extent of tumor involvement in the hypopharynx including invasion through the hyoid boneFrom the collection of Dr Fabio Almeida; used with permission [Citation ends].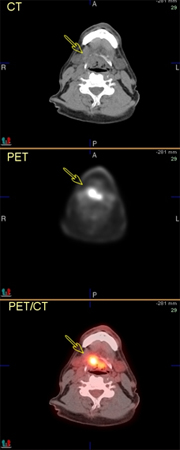
Result
demonstrates tumor size, extension, presence or absence of involved neck nodes, distant metastases, and second primary
panendoscopy or triple endoscopy
Test
Indicated in the presence of neck metastases of unknown primary after PET-CT to biopsy suspected sites.[68]
Given the potential benefit of triple endoscopy in detecting small second primary lesions in patients with a high risk of second primaries because of their lifestyle (e.g., heavy smoking and drinking), the role of triple endoscopy can be seen as complementary to PET scanning in selected patients, particularly if the patient has risk factors such as smoking and heavy alcohol use.
Result
detects second primary or tumor not visible on imaging for blind biopsy
modified barium swallow
excision biopsy of neck nodes
Test
Usually performed if fine needle aspiration cytology is inconclusive after multiple attempts.
Result
detects neck node metastases
circulating tumor high-risk HPV DNA
CBC
Test
Baseline blood counts are necessary before biopsy, chemotherapy, and radiation and should be repeated during treatment because of bone marrow depression from both chemotherapy and radiation.
Result
usually normal but may show anemia
electrolytes
Test
Recommended as baseline before treatment.
Result
usually normal but may be elevated
BUN
Test
Poor oral intake may lead to prerenal azotemia. Cisplatin-based chemotherapy may lead to renal failure and ototoxicity during treatment and requires close monitoring.
Result
usually normal but may be elevated
serum creatinine
Test
Cisplatin-based chemotherapy may lead to renal failure during treatment and requires close monitoring.
Result
usually normal but may be elevated
total protein
Test
Recommended as baseline before treatment because of weight loss for nutritional support and during radiation or chemoradiation because of mucositis.
Result
usually normal but may be low
albumin
Test
Recommended as baseline before treatment because of weight loss for nutritional support and during radiation or chemoradiation because of mucositis.
Result
usually normal but may be low
prealbumin
Test
Recommended as baseline before treatment because of weight loss for nutritional support and during radiation or chemoradiation because of mucositis.
Result
usually normal but may be low
LFTs
Test
If elevated, usually indicates liver disease from chronic alcohol consumption. Elevated alkaline phosphatase level may indicate bony metastases.
Result
usually normal but may be elevated
Use of this content is subject to our disclaimer