Tests
1st tests to order
echocardiogram
Test
The preferred imaging modality. [Figure caption and citation for the preceding image starts]: Apical 4-chamber echocardiographic image of an ostium primum defect (arrows). LA: left atrium; LV: left ventricle; RA: right atriumImage courtesy of Patrick W. O'Leary, MD [Citation ends].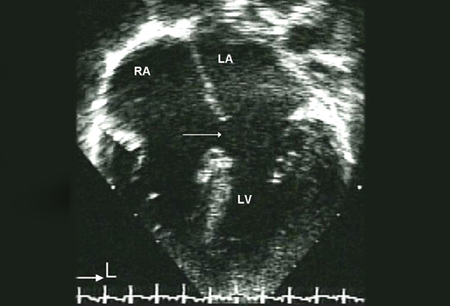 [Figure caption and citation for the preceding image starts]: Parasternal short-axis echocardiographic image demonstrating right ventricular enlargement in a patient with an interatrial communication. LV: left ventricle; RV: right ventricleImage courtesy of Patrick W. O'Leary, MD [Citation ends].
[Figure caption and citation for the preceding image starts]: Parasternal short-axis echocardiographic image demonstrating right ventricular enlargement in a patient with an interatrial communication. LV: left ventricle; RV: right ventricleImage courtesy of Patrick W. O'Leary, MD [Citation ends].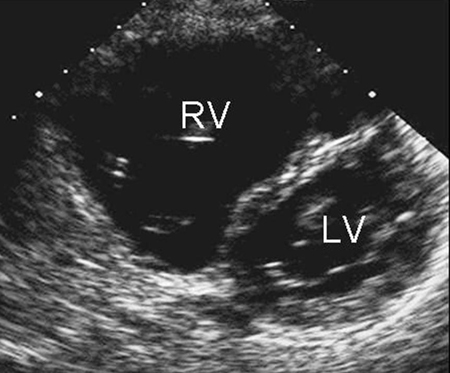 [Figure caption and citation for the preceding image starts]: Apical 4-chamber echocardiographic image demonstrating right ventricular enlargement in a patient with an interatrial communication. L: lateral; LV: left ventricle; RA: right atrium; RV: right ventricle; S: superiorImage courtesy of Patrick W. O'Leary, MD [Citation ends].
[Figure caption and citation for the preceding image starts]: Apical 4-chamber echocardiographic image demonstrating right ventricular enlargement in a patient with an interatrial communication. L: lateral; LV: left ventricle; RA: right atrium; RV: right ventricle; S: superiorImage courtesy of Patrick W. O'Leary, MD [Citation ends].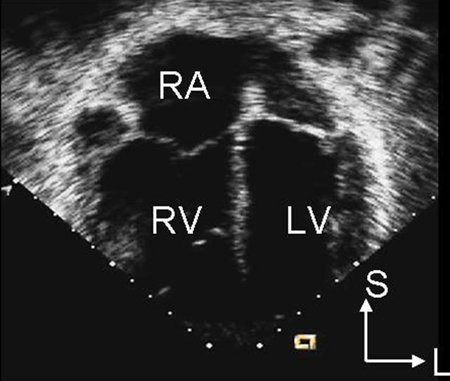
Transthoracic echocardiography is usually useful in demonstrating a defect in children. Transesophageal echocardiography is often necessary in older patients if the transthoracic image quality is poor. Image quality may be poorer in adults.
Useful to identify all types of interatrial communications, to determine defect size and adequacy of the rim for device placement in secundum defects, and to ensure normally connected pulmonary veins.
Two-dimensional echocardiography demonstrates right atrial and ventricular enlargement, as well as the defect itself, especially for secundum defects.
Interatrial communications are best seen in subcostal views due to the septum being orthogonal to the ultrasound beam. Secundum defects result in dropout of the mid portion of the atrial septum, and primum defects result in dropout of the inferior portion, in a four-chamber view from the apex.
Superior sinus venosus defects are defined by an interatrial communication in the posterosuperior portion of the atrium, with the superior caval vein at times overriding the defect. Coronary sinus defects have a communication at the orifice of the coronary sinus.
Doppler examination is used to characterize shunt volume and to determine flow pattern through the defect. Noninvasive calculation of the ratio of pulmonary to systemic blood flow, Qp:Qs, can be done with Doppler echocardiography but is no longer used stringently to make clinical decisions.
Contrast media or "bubble study" can help demonstrate a right-to-left shunt (e.g., if a sinus venosus defect cannot be visualized directly), especially with Valsalva maneuver.
Result
visualization of the defect; determination of flow pattern and shunt volume
ECG
Test
Not a diagnostic test, but diagnostic clues may be present. Often normal if the shunt is small.
P waves >2.5 mm, suggesting right atrial enlargement, or R-wave voltages in lead V1 greater than the upper limit of normal for age, suggesting right ventricular hypertrophy, may be present in larger defects. A notch near the apex of the R wave in the inferior limb leads, known as the crochetage pattern, is also found in patients with interatrial communications.
Primum-type defects frequently produce a counterclockwise frontal-plane loop and left-axis deviation.
Sinus venosus defects are associated with a P-wave axis <30°.[24]
Result
normal; or tall P waves, large R waves in V1, crochetage pattern in inferior limb leads
chest x-ray
Test
Not diagnostic, but diagnostic clues may be present.
May be normal if left-to-right shunt is small. With larger shunt volumes, heart may be enlarged and pulmonary vascular markings may be increased.
Cannot differentiate between different types of interatrial communications.
Result
normal or enlarged heart with increased pulmonary markings
Tests to consider
pulse oximetry
Test
May help to define the amount of right-to-left shunting and resulting cyanosis. Systemic arterial desaturation may occur in older patients as a consequence of elevated pulmonary vascular resistance, or in patients with left superior vena cava draining directly to the left atrium in unroofed coronary sinus defects.
Result
cyanosis if relevant right-to-left shunting
chest CT/MRI
Test
May be needed to help define pulmonary venous anatomy if echocardiography is insufficient. The ability to view structures simultaneously in all 3 dimensions makes CT/MRI valuable in delineating complex congenital heart disease, particularly in patients with limited acoustic windows.[10] Both CT and MR angiography help delineate extracardiac lesions that are not, or inadequately, shown on echocardiography. They may be needed in patients with interatrial communications to help define pulmonary venous anatomy if all pulmonary veins cannot be shown by transthoracic or trans-esophageal echocardiography.[10]
Hemodynamic data, direction of intracardiac shunting, and degree of shunting, can be calculated from MRI phase-contrast imaging. In addition, physiologic sequelae, including pulmonary artery dilation and pulmonary vascular pruning, can be identified.[10]
Result
clarification of pulmonary venous anatomy
cardiac catheterization
Test
Not required for diagnosis, but is used to detect pulmonary vascular resistance in the subset of patients at risk for pulmonary vascular obstructive disease; it is considered the gold standard for measuring hemodynamics in patients with congenital heart disease and advanced pulmonary vascular disease, especially to assess operability.[10]
If patients develop a right-to-left shunt, reversibility of the shunt with pulmonary vasodilators should be assessed to guide therapy. If the right-to-left shunt is reversible with pulmonary vasodilators, the interatrial communication can be surgically closed. However, if the right-to-left shunt is irreversible, surgery is not an option.
When available, inhaled nitric oxide, alone or in combination with oxygen, is considered the preferred agent for vasodilator testing. It is safe and short acting and offers a better pulmonary vasodilator effect than systemic agents. However, nitric oxide is not always affordable and thus is not readily available in all cardiac catheterization laboratories, particularly in low- to middle-income countries. Alternative vasodilator agents include epoprostenol, adenosine, iloprost, treprostinil, milrinone, and nitroglycerin.[10]
Result
detection of pulmonary vascular resistance; reversibility of right-to-left shunt
Use of this content is subject to our disclaimer