Adhesive capsulitis
- Overview
- Theory
- Diagnosis
- Management
- Follow up
- Resources
Treatment algorithm
Please note that formulations/routes and doses may differ between drug names and brands, drug formularies, or locations. Treatment recommendations are specific to patient groups: see disclaimer
all patients
activity modification and physical therapy
Patients should be advised to avoid exacerbating activities in order to interrupt the cycle of ongoing inflammation. This may mean that pain control and avoidance of physical therapy are necessary in the early painful stages of treatment.
Physical therapy is the cornerstone of successful treatment of adhesive capsulitis, and should be initiated as early as possible in the disease course.
A home exercise regimen, consisting of both active and passive range of motion exercises, combined with formal supervised outpatient therapy is optimal once pain control is achieved.[38]Hanchard NC, Goodchild L, Thompson J, et al. Evidence-based clinical guidelines for the diagnosis, assessment and physiotherapy management of contracted (frozen) shoulder: quick reference summary. Physiotherapy. 2012 Jun;98(2):117-20. http://www.ncbi.nlm.nih.gov/pubmed/22507361?tool=bestpractice.com
Preliminary findings from a systematic review of 7 different mobilization techniques have shown that the Maitland technique (a high-grade mobilization technique) and combined mobilizations have beneficial effects. However, more research is needed to determine the most successful mobilization technique.[40]Noten S, Meeus M, Stassijns G, et al. Efficacy of different types of mobilization techniques in patients with primary adhesive capsulitis of the shoulder: a systematic review. Arch Phys Med Rehabil. 2016 May;97(5):815-25. http://www.ncbi.nlm.nih.gov/pubmed/26284892?tool=bestpractice.com
Addition of treatment modalities such as iontophoresis (electrical pulse activity), phonophoresis (ultrasound therapy), and cryotherapy may be of some benefit. However, evidence supporting their success is not clear.[41]Green S, Buchbinder R, Hetrick S. Physiotherapy interventions for shoulder pain. Cochrane Database Syst Rev. 2003 Apr 22;(2):CD004258. https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD004258/full http://www.ncbi.nlm.nih.gov/pubmed/12804509?tool=bestpractice.com
A useful exercise that can be performed at the patient's home and with the therapist is known as the sleeper stretch, which works on improving internal rotation. In the lateral decubitus position (patient on side), with the affected shoulder down against the bed, the elbow is flexed 90° and the unaffected arm pushes it toward the bed. [Figure caption and citation for the preceding image starts]: Demonstration of sleeper stretch exerciseFrom the private collection of Matthew T. Provencher, MD, CDR MC USN and Lance E. LeClere, MD, LCDR MC USN; used with permission [Citation ends].
nonsteroidal anti-inflammatory drug (NSAID) or oral corticosteroid
Treatment recommended for ALL patients in selected patient group
As the initial stages of adhesive capsulitis are associated with an inflammatory process, NSAIDs may provide symptomatic relief as well as decrease the severity of the disease. They are regarded as the mainstay of treatment and should be considered for all patients presenting with evidence of adhesive capsulitis providing there are no contraindications.
There is some limited evidence that oral corticosteroids may offer early pain relief, but the benefits are short-term and may not last beyond 6 weeks.[42]Buchbinder R, Green S, Youd JM, et al. Oral steroids for adhesive capsulitis. Cochrane Database Syst Rev. 2006 Oct 18;(4):CD006189. https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD006189/full http://www.ncbi.nlm.nih.gov/pubmed/17054278?tool=bestpractice.com An oral corticosteroid may be considered an alternative to NSAIDs in the earlier phases of the disease, during painful periods and flare-ups associated with decreased range of glenohumeral motion. However, most physicians prefer to perform a glenohumeral or subacromial injection with corticosteroid if NSAIDs are not effective. One randomized controlled trial has shown that intra-articular injection provides greater improvement in range of motion and patient satisfaction after 4 weeks, compared with oral corticosteroids.[43]Lorbach O, Anagnostakos K, Scherf C, et al. Nonoperative management of adhesive capsulitis of the shoulder: oral cortisone application versus intra-articular cortisone injections. J Shoulder Elbow Surg. 2010 Mar;19(2):172-9. http://www.ncbi.nlm.nih.gov/pubmed/19800262?tool=bestpractice.com
Primary options
ibuprofen: 200-400 mg orally every 4-6 hours when required, maximum 2400 mg/day
OR
meloxicam: 7.5 mg orally once or twice daily when required, maximum 15 mg/day
OR
naproxen: 500 mg orally initially, followed by 250 mg every 6-8 hours when required, maximum 1250 mg/day
Secondary options
methylprednisolone: 24 mg orally once daily on day one, then decrease dose by 4 mg/day over 6 days
corticosteroid injection
The preferred technique is an intra-articular glenohumeral injection using triamcinolone acetonide administered together with a local anesthetic (e.g., lidocaine without epinephrine).
Provides a concentrated, local treatment of the inflammatory process involved in adhesive capsulitis. It also provides the added benefit of pain relief, which is invaluable for participation in physical therapy.[43]Lorbach O, Anagnostakos K, Scherf C, et al. Nonoperative management of adhesive capsulitis of the shoulder: oral cortisone application versus intra-articular cortisone injections. J Shoulder Elbow Surg. 2010 Mar;19(2):172-9. http://www.ncbi.nlm.nih.gov/pubmed/19800262?tool=bestpractice.com [47]Marx RG, Malizia RW, Kenter K, et al. Intra-articular corticosteroid injection for the treatment of idiopathic adhesive capsulitis of the shoulder. HSS J. 2007 Sep;3(2):202-7. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2504264 http://www.ncbi.nlm.nih.gov/pubmed/18751795?tool=bestpractice.com [48]Bulgen DY, Binder AI, Hazleman BL, et al. Frozen shoulder: prospective clinical study with an evaluation of three treatment regimens. Ann Rheum Dis. 1984 Jun;43(3):353-60. https://ard.bmj.com/content/annrheumdis/43/3/353.full.pdf http://www.ncbi.nlm.nih.gov/pubmed/6742895?tool=bestpractice.com [49]Shah N, Lewis M. Shoulder adhesive capsulitis: systematic review of randomised trials using multiple corticosteroid injections. Br J Gen Pract. 2007 Aug;57(541):662-7. https://bjgp.org/content/57/541/662.long http://www.ncbi.nlm.nih.gov/pubmed/17688763?tool=bestpractice.com [50]Blanchard V, Barr S, Cerisola FL. The effectiveness of corticosteroid injections compared with physiotherapeutic interventions for adhesive capsulitis: a systematic review. Physiotherapy. 2010 Jun;96(2):95-107. http://www.ncbi.nlm.nih.gov/pubmed/20420956?tool=bestpractice.com [51]Jacobs LG, Smith MG, Khan SA, et al. Manipulation or intra-articular steroids in the management of adhesive capsulitis of the shoulder? A prospective randomized trial. J Shoulder Elbow Surg. May-Jun 2009;18(3):348-53. http://www.ncbi.nlm.nih.gov/pubmed/19393928?tool=bestpractice.com [52]Bal A, Eksioglu E, Gulec B, et al. Effectiveness of corticosteroid injection in adhesive capsulitis. Clin Rehabil. 2008 Jun;22(6):503-12. http://www.ncbi.nlm.nih.gov/pubmed/18511530?tool=bestpractice.com It may therefore be considered for those patients who present with pain despite initial physical therapy and NSAIDs.
A randomized controlled trial found that an intra-articular corticosteroid injection given prior to the start of a physical therapy program provided faster improvement in pain, range of motion, and function compared with oral NSAIDs and physical therapy for up to 8 weeks after treatment. However, no significant difference was found at the final follow-up at 3 months. This finding is similar to previous studies; therefore, it is reasonable to consider offering a corticosteroid injection prior to the start of a physical therapy program in order to facilitate early, aggressive physical therapy.[53]Page MJ, Green S, Kramer S, et al. Manual therapy and exercise for adhesive capsulitis (frozen shoulder). Cochrane Database Syst Rev. 2014 Aug 26;(8):CD011275. https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD011275/full http://www.ncbi.nlm.nih.gov/pubmed/25157702?tool=bestpractice.com [54]Ranalletta M, Rossi LA, Bongiovanni SL, et al. Corticosteroid injections accelerate pain relief and recovery of function compared with oral NSAIDs in patients with adhesive capsulitis: a randomized controlled trial. Am J Sports Med. 2016 Feb;44(2):474-81. http://www.ncbi.nlm.nih.gov/pubmed/26657263?tool=bestpractice.com
One meta-analysis shows that multiple injections are beneficial for up to 16 weeks on average, with as many as 3 injections having a positive effect.[49]Shah N, Lewis M. Shoulder adhesive capsulitis: systematic review of randomised trials using multiple corticosteroid injections. Br J Gen Pract. 2007 Aug;57(541):662-7. https://bjgp.org/content/57/541/662.long http://www.ncbi.nlm.nih.gov/pubmed/17688763?tool=bestpractice.com
Contraindications include septic arthritis, previous adverse reaction, or systemic infection.
Injection into the subacromial space can be considered; there is some evidence that this is equally beneficial and may result in fewer corticosteroid-related adverse effects.[55]Shang X, Zhang Z, Pan X, et al. Intra-articular versus subacromial corticosteroid injection for the treatment of adhesive capsulitis: a meta-analysis and systematic review. Biomed Res Int. 2019;2019:1274790. https://www.hindawi.com/journals/bmri/2019/1274790 http://www.ncbi.nlm.nih.gov/pubmed/31737653?tool=bestpractice.com
Primary options
triamcinolone acetonide: consult specialist for guidance on intramuscular or subacromial space injection
activity modification and physical therapy
Treatment recommended for ALL patients in selected patient group
Patients should be advised to avoid exacerbating activities in order to interrupt the cycle of ongoing inflammation. This may mean that pain control and avoidance of physical therapy are necessary in the early painful stages of treatment.
Physical therapy is the cornerstone of successful treatment of adhesive capsulitis, and should be initiated as early as possible in the disease course.
A home exercise regimen, consisting of both active and passive range of motion exercises, combined with formal supervised outpatient therapy is optimal once pain control is achieved.[38]Hanchard NC, Goodchild L, Thompson J, et al. Evidence-based clinical guidelines for the diagnosis, assessment and physiotherapy management of contracted (frozen) shoulder: quick reference summary. Physiotherapy. 2012 Jun;98(2):117-20. http://www.ncbi.nlm.nih.gov/pubmed/22507361?tool=bestpractice.com
Preliminary findings from a systematic review of 7 different mobilization techniques have shown that the Maitland technique (a high-grade mobilization technique) and combined mobilizations have beneficial effects. However, more research is needed to determine the most successful mobilization technique.[40]Noten S, Meeus M, Stassijns G, et al. Efficacy of different types of mobilization techniques in patients with primary adhesive capsulitis of the shoulder: a systematic review. Arch Phys Med Rehabil. 2016 May;97(5):815-25. http://www.ncbi.nlm.nih.gov/pubmed/26284892?tool=bestpractice.com
Addition of treatment modalities such as iontophoresis (electrical pulse activity), phonophoresis (ultrasound therapy), and cryotherapy may be of some benefit. However, evidence supporting their success is not clear.[41]Green S, Buchbinder R, Hetrick S. Physiotherapy interventions for shoulder pain. Cochrane Database Syst Rev. 2003 Apr 22;(2):CD004258. https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD004258/full http://www.ncbi.nlm.nih.gov/pubmed/12804509?tool=bestpractice.com
A useful exercise that can be performed at the patient's home and with the therapist is known as the sleeper stretch, which works on improving internal rotation. In the lateral decubitus position (patient on side), with the affected shoulder down against the bed, the elbow is flexed 90° and the unaffected arm pushes it toward the bed. [Figure caption and citation for the preceding image starts]: Demonstration of sleeper stretch exerciseFrom the private collection of Matthew T. Provencher, MD, CDR MC USN and Lance E. LeClere, MD, LCDR MC USN; used with permission [Citation ends].
NSAID
Treatment recommended for SOME patients in selected patient group
As the initial stages of adhesive capsulitis are associated with an inflammatory process, early in the disease course a scheduled regimen of NSAIDs may provide symptomatic relief as well as decrease the severity of the disease.
They may provide additional symptomatic relief in those patients receiving corticosteroid injection providing there are no contraindications.
Primary options
ibuprofen: 200-400 mg orally every 4-6 hours when required, maximum 2400 mg/day
OR
meloxicam: 7.5 mg orally once or twice daily when required, maximum 15 mg/day
OR
naproxen: 500 mg orally initially, followed by 250 mg every 6-8 hours when required, maximum 1250 mg/day
manipulation under anesthesia
If oral pharmacotherapeutic interventions and intra-articular corticosteroid injections do not provide sufficient pain relief and the patient is not progressing in physical therapy, then manipulation under general anesthesia and pharmacologic muscle relaxation can free adhesive and fibrotic tissues and may allow for a gain in range of motion.[56]Flannery O, Mullett H, Colville J. Adhesive shoulder capsulitis: does the timing of manipulation influence outcome? Acta Orthop Belg. 2007 Feb;73(1):21-5. http://www.ncbi.nlm.nih.gov/pubmed/17441653?tool=bestpractice.com
There is evidence that early manipulation is more effective than manipulation later in the disease course.[56]Flannery O, Mullett H, Colville J. Adhesive shoulder capsulitis: does the timing of manipulation influence outcome? Acta Orthop Belg. 2007 Feb;73(1):21-5. http://www.ncbi.nlm.nih.gov/pubmed/17441653?tool=bestpractice.com
Patients may experience an increase in pain following manipulation. Placement of an inter-scalene anesthetic block or inter-scalene infusion pump can allow for post-manipulative analgesia, and thus more aggressive post-manipulative physical therapy.
Care should be exercised when treating patients with previous surgery or poor bone quality to prevent disruption of previous surgical repairs or fractures.
Concern over fracture or intra-articular pathology has led some to advocate for arthroscopic capsular release over manipulation under anesthesia.[57]Neviaser AS, Neviaser RJ. Adhesive capsulitis of the shoulder. J Am Acad Orthop Surg. 2011 Sep;19(9):536-42. https://journals.lww.com/jaaos/Fulltext/2011/09000/Adhesive_Capsulitis_of_the_Shoulder.4.aspx http://www.ncbi.nlm.nih.gov/pubmed/21885699?tool=bestpractice.com [58]Loew M, Heichel TO, Lehner B. Intraarticular lesions in primary frozen shoulder after manipulation under general anesthesia. J Shoulder Elbow Surg. Jan-Feb 2005;14(1):16-21. http://www.ncbi.nlm.nih.gov/pubmed/15723009?tool=bestpractice.com The two procedures may also be performed in conjunction.
To date, there have not been any high-quality studies to support the use of arthroscopic release with or without the addition of a manipulation under anesthesia. However, one systematic review demonstrated a mild benefit of arthroscopic capsular release over manipulation under anesthesia in patients with diabetes or recalcitrant idiopathic adhesive capsulitis.[59]Grant JA, Schroeder N, Miller BS, et al. Comparison of manipulation and arthroscopic capsular release for adhesive capsulitis: a systematic review. J Shoulder Elbow Surg. 2013 Aug;22(8):1135-45. http://www.ncbi.nlm.nih.gov/pubmed/23510748?tool=bestpractice.com One multicenter, three-armed, superiority randomized trial compared manipulation under anesthesia, arthroscopic capsular release, or early structured physical therapy in patients with adhesive capsulitis referred to secondary care. The study reported none of the interventions as clinically superior, based on the primary outcome targets of a 5-point difference on the Oxford Shoulder Score (OSS; 0-48) between physical therapy and either form of surgery, or 4 points difference between manipulation and capsular release at 12 months after randomization.[60]Rangan A, Brealey SD, Keding A, et al. Management of adults with primary frozen shoulder in secondary care (UK FROST): a multicentre, pragmatic, three-arm, superiority randomised clinical trial. Lancet. 2020 Oct 3;396(10256):977-89. https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(20)31965-6/fulltext http://www.ncbi.nlm.nih.gov/pubmed/33010843?tool=bestpractice.com
activity modification and physical therapy
Treatment recommended for ALL patients in selected patient group
Patients should be advised to avoid exacerbating activities in order to interrupt the cycle of ongoing inflammation. This may mean that pain control and avoidance of physical therapy are necessary in the early painful stages of treatment.
Physical therapy is the cornerstone of successful treatment of adhesive capsulitis, and should be initiated as early as possible in the disease course.
A home exercise regimen, consisting of both active and passive range of motion exercises, combined with formal supervised outpatient therapy is optimal once pain control is achieved.[38]Hanchard NC, Goodchild L, Thompson J, et al. Evidence-based clinical guidelines for the diagnosis, assessment and physiotherapy management of contracted (frozen) shoulder: quick reference summary. Physiotherapy. 2012 Jun;98(2):117-20. http://www.ncbi.nlm.nih.gov/pubmed/22507361?tool=bestpractice.com
Preliminary findings from a systematic review of 7 different mobilization techniques have shown that the Maitland technique (a high-grade mobilization technique) and combined mobilizations have beneficial effects. However, more research is needed to determine the most successful mobilization technique.[40]Noten S, Meeus M, Stassijns G, et al. Efficacy of different types of mobilization techniques in patients with primary adhesive capsulitis of the shoulder: a systematic review. Arch Phys Med Rehabil. 2016 May;97(5):815-25. http://www.ncbi.nlm.nih.gov/pubmed/26284892?tool=bestpractice.com
Addition of treatment modalities such as iontophoresis (electrical pulse activity), phonophoresis (ultrasound therapy), and cryotherapy may be of some benefit. However, evidence supporting their success is not clear.[41]Green S, Buchbinder R, Hetrick S. Physiotherapy interventions for shoulder pain. Cochrane Database Syst Rev. 2003 Apr 22;(2):CD004258. https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD004258/full http://www.ncbi.nlm.nih.gov/pubmed/12804509?tool=bestpractice.com
A useful exercise that can be performed at the patient's home and with the therapist is known as the sleeper stretch, which works on improving internal rotation. In the lateral decubitus position (patient on side), with the affected shoulder down against the bed, the elbow is flexed 90° and the unaffected arm pushes it toward the bed. [Figure caption and citation for the preceding image starts]: Demonstration of sleeper stretch exerciseFrom the private collection of Matthew T. Provencher, MD, CDR MC USN and Lance E. LeClere, MD, LCDR MC USN; used with permission [Citation ends].
NSAID
Treatment recommended for SOME patients in selected patient group
As the initial stages of adhesive capsulitis are associated with an inflammatory process, early in the disease course a scheduled regimen of NSAIDs may provide symptomatic relief as well as decrease the severity of the disease.
They may provide additional symptomatic relief in those patients undergoing manipulation under anesthesia providing there are no contraindications.
Primary options
ibuprofen: 200-400 mg orally every 4-6 hours when required, maximum 2400 mg/day
OR
meloxicam: 7.5 mg orally once or twice daily when required, maximum 15 mg/day
OR
naproxen: 500 mg orally initially, followed by 250 mg every 6-8 hours when required, maximum 1250 mg/day
hydrodilation
There is evidence that arthrographic distension, or hydrodilation, with saline and corticosteroid provides short-term benefits in pain, range of movement, and function in adhesive capsulitis. It is uncertain whether this is better than alternative interventions.[61]Buchbinder R, Green S, Youd JM, et al. Arthrographic distension for adhesive capsulitis (frozen shoulder). Cochrane Database Syst Rev. 2008 Jan 23;(1):CD007005. https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD007005/full http://www.ncbi.nlm.nih.gov/pubmed/18254123?tool=bestpractice.com
One randomized trial evaluating the efficacy of three injection methods (i.e., intra-articular corticosteroid, subacromial space corticosteroid, and hydrodilation) in the treatment of primary adhesive capsulitis found more rapid improvement in pain and range of motion with hydrodilation at 1- and 3-month follow-up, but similar clinical outcomes among all three groups at the final follow-up at 6 months.[62]Yoon JP, Chung SW, Kim JE, et al. Intra-articular injection, subacromial injection, and hydrodilatation for primary frozen shoulder: a randomized clinical trial. J Shoulder Elbow Surg. 2016 Mar;25(3):376-83. http://www.ncbi.nlm.nih.gov/pubmed/26927433?tool=bestpractice.com
activity modification and physical therapy
Treatment recommended for ALL patients in selected patient group
Patients should be advised to avoid exacerbating activities in order to interrupt the cycle of ongoing inflammation. This may mean that pain control and avoidance of physical therapy are necessary in the early painful stages of treatment.
Physical therapy is the cornerstone of successful treatment of adhesive capsulitis, and should be initiated as early as possible in the disease course.
A home exercise regimen, consisting of both active and passive range of motion exercises, combined with formal supervised outpatient therapy is optimal once pain control is achieved.[38]Hanchard NC, Goodchild L, Thompson J, et al. Evidence-based clinical guidelines for the diagnosis, assessment and physiotherapy management of contracted (frozen) shoulder: quick reference summary. Physiotherapy. 2012 Jun;98(2):117-20. http://www.ncbi.nlm.nih.gov/pubmed/22507361?tool=bestpractice.com
Preliminary findings from a systematic review of 7 different mobilization techniques have shown that the Maitland technique (a high-grade mobilization technique) and combined mobilizations have beneficial effects. However, more research is needed to determine the most successful mobilization technique.[40]Noten S, Meeus M, Stassijns G, et al. Efficacy of different types of mobilization techniques in patients with primary adhesive capsulitis of the shoulder: a systematic review. Arch Phys Med Rehabil. 2016 May;97(5):815-25. http://www.ncbi.nlm.nih.gov/pubmed/26284892?tool=bestpractice.com
Addition of treatment modalities such as iontophoresis (electrical pulse activity), phonophoresis (ultrasound therapy), and cryotherapy may be of some benefit. However, evidence supporting their success is not clear.[41]Green S, Buchbinder R, Hetrick S. Physiotherapy interventions for shoulder pain. Cochrane Database Syst Rev. 2003 Apr 22;(2):CD004258. https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD004258/full http://www.ncbi.nlm.nih.gov/pubmed/12804509?tool=bestpractice.com
A useful exercise that can be performed at the patient's home and with the therapist is known as the sleeper stretch, which works on improving internal rotation. In the lateral decubitus position (patient on side), with the affected shoulder down against the bed, the elbow is flexed 90° and the unaffected arm pushes it toward the bed. [Figure caption and citation for the preceding image starts]: Demonstration of sleeper stretch exerciseFrom the private collection of Matthew T. Provencher, MD, CDR MC USN and Lance E. LeClere, MD, LCDR MC USN; used with permission [Citation ends].
NSAID
Treatment recommended for SOME patients in selected patient group
As the initial stages of adhesive capsulitis are associated with an inflammatory process, early in the disease course a scheduled regimen of NSAIDs may provide symptomatic relief as well as decrease the severity of the disease.
They may provide additional symptomatic relief in those patients undergoing hydrodilation providing there are no contraindications.
Primary options
ibuprofen: 200-400 mg orally every 4-6 hours when required, maximum 2400 mg/day
OR
meloxicam: 7.5 mg orally once or twice daily when required, maximum 15 mg/day
OR
naproxen: 500 mg orally initially, followed by 250 mg every 6-8 hours when required, maximum 1250 mg/day
arthroscopic capsular release
Over time, arthroscopy has come to play an essential role in the surgical treatment of refractory adhesive capsulitis.
Arthroscopic release of the anterior capsule, rotator interval, and/or release of the coracohumeral ligament provides improvement in pain and function.[18]Berghs BM, Sole-Molins X, Bunker TD. Arthroscopic release of adhesive capsulitis. J Shoulder Elbow Surg. Mar-Apr 2004;13(2):180-5. http://www.ncbi.nlm.nih.gov/pubmed/14997096?tool=bestpractice.com [63]Pearsall AW 4th, Osbahr DC, Speer KP. An arthroscopic technique for treating patients with frozen shoulder. Arthroscopy. Jan-Feb 1999;15(1):2-11. http://www.ncbi.nlm.nih.gov/pubmed/10024027?tool=bestpractice.com [64]Warner JJ, Allen A, Marks PH, et al. Arthroscopic release for chronic, refractory adhesive capsulitis of the shoulder. J Bone Joint Surg Am. 1996 Dec;78(12):1808-16. http://www.ncbi.nlm.nih.gov/pubmed/8986657?tool=bestpractice.com [65]Warner JJ, Allen AA, Marks PH, et al. Arthroscopic release of postoperative capsular contracture of the shoulder. J Bone Joint Surg Am. 1997 Aug;79(8):1151-8. http://www.ncbi.nlm.nih.gov/pubmed/9278074?tool=bestpractice.com Both short-term and long-term benefits have been shown.[18]Berghs BM, Sole-Molins X, Bunker TD. Arthroscopic release of adhesive capsulitis. J Shoulder Elbow Surg. Mar-Apr 2004;13(2):180-5. http://www.ncbi.nlm.nih.gov/pubmed/14997096?tool=bestpractice.com [66]Nicholson GP. Arthroscopic capsular release for stiff shoulders: effect of etiology on outcomes. Arthroscopy. 2003 Jan;19(1):40-9. http://www.ncbi.nlm.nih.gov/pubmed/12522401?tool=bestpractice.com [67]Ide J, Takagi K. Early and long-term results of arthroscopic treatment for shoulder stiffness. J Shoulder Elbow Surg. Mar-Apr 2004;13(2):174-9. http://www.ncbi.nlm.nih.gov/pubmed/14997095?tool=bestpractice.com A posterior capsular release may be considered with loss of internal rotation despite adequate physical therapy and stretching. Release of the intra-articular portion of the subscapularis tendon and/or an extended release of the inferior glenohumeral ligament from inferior to posterior may improve range of motion, but only short-term results are available.[68]Liem D, Meier F, Thorwesten L, et al. The influence of arthroscopic subscapularis tendon and capsule release on internal rotation strength in treatment of frozen shoulder. Am J Sports Med. 2008 May;36(5):921-6. http://www.ncbi.nlm.nih.gov/pubmed/18272795?tool=bestpractice.com [69]Chen J, Chen S, Li Y, et al. Is the extended release of the inferior glenohumeral ligament necessary for frozen shoulder? Arthroscopy. 2010 Apr;26(4):529-35. http://www.ncbi.nlm.nih.gov/pubmed/20362834?tool=bestpractice.com
The use of arthroscopic release is being considered earlier in the course of the disease. However, optimal timing of surgical intervention has yet to be defined.[Figure caption and citation for the preceding image starts]: Arthroscopic view of contracted anterior capsule with extensive synovitis and thickeningFrom the private collection of Matthew T. Provencher, MD, CDR MC USN and Lance E. LeClere, MD, LCDR MC USN; used with permission [Citation ends]. [Figure caption and citation for the preceding image starts]: Arthroscopic view of completed anterior releaseFrom the private collection of Matthew T. Provencher, MD, CDR MC USN and Lance E. LeClere, MD, LCDR MC USN; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Arthroscopic view of completed anterior releaseFrom the private collection of Matthew T. Provencher, MD, CDR MC USN and Lance E. LeClere, MD, LCDR MC USN; used with permission [Citation ends].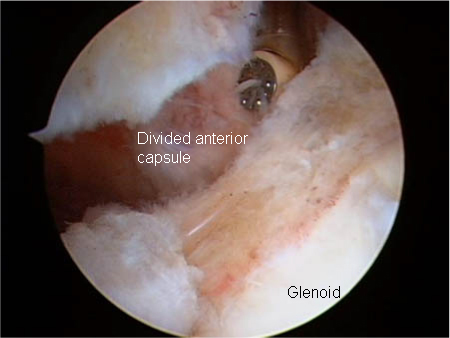 [Figure caption and citation for the preceding image starts]: Arthroscopic view of contracted rotator interval showing extensive scarring and synovitisFrom the private collection of Matthew T. Provencher, MD, CDR MC USN and Lance E. LeClere, MD, LCDR MC USN; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Arthroscopic view of contracted rotator interval showing extensive scarring and synovitisFrom the private collection of Matthew T. Provencher, MD, CDR MC USN and Lance E. LeClere, MD, LCDR MC USN; used with permission [Citation ends].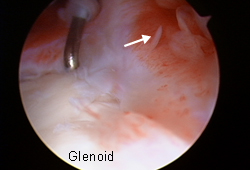 [Figure caption and citation for the preceding image starts]: Arthroscopic view of rotator interval releaseFrom the private collection of Matthew T. Provencher, MD, CDR MC USN and Lance E. LeClere, MD, LCDR MC USN; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Arthroscopic view of rotator interval releaseFrom the private collection of Matthew T. Provencher, MD, CDR MC USN and Lance E. LeClere, MD, LCDR MC USN; used with permission [Citation ends]. [Figure caption and citation for the preceding image starts]: Arthroscopic view of posterior capsular releaseFrom the private collection of Matthew T. Provencher, MD, CDR MC USN and Lance E. LeClere, MD, LCDR MC USN; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Arthroscopic view of posterior capsular releaseFrom the private collection of Matthew T. Provencher, MD, CDR MC USN and Lance E. LeClere, MD, LCDR MC USN; used with permission [Citation ends].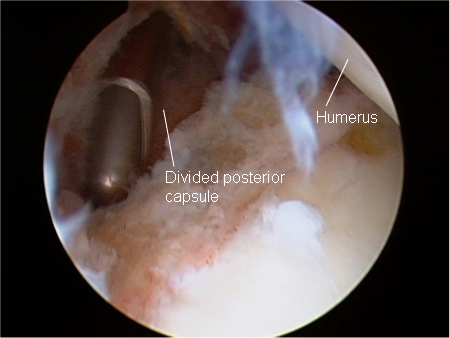
activity modification and physical therapy
Treatment recommended for ALL patients in selected patient group
Patients should be advised to avoid exacerbating activities in order to interrupt the cycle of ongoing inflammation. This may mean that pain control and avoidance of physical therapy are necessary in the early painful stages of treatment.
Physical therapy is the cornerstone of successful treatment of adhesive capsulitis, and should be initiated as early as possible in the disease course.
A home exercise regimen, consisting of both active and passive range of motion exercises, combined with formal supervised outpatient therapy is optimal once pain control is achieved.[38]Hanchard NC, Goodchild L, Thompson J, et al. Evidence-based clinical guidelines for the diagnosis, assessment and physiotherapy management of contracted (frozen) shoulder: quick reference summary. Physiotherapy. 2012 Jun;98(2):117-20. http://www.ncbi.nlm.nih.gov/pubmed/22507361?tool=bestpractice.com
Preliminary findings from a systematic review of 7 different mobilization techniques have shown that the Maitland technique (a high-grade mobilization technique) and combined mobilizations have beneficial effects. However, more research is needed to determine the most successful mobilization technique.[40]Noten S, Meeus M, Stassijns G, et al. Efficacy of different types of mobilization techniques in patients with primary adhesive capsulitis of the shoulder: a systematic review. Arch Phys Med Rehabil. 2016 May;97(5):815-25. http://www.ncbi.nlm.nih.gov/pubmed/26284892?tool=bestpractice.com
Addition of treatment modalities such as iontophoresis (electrical pulse activity), phonophoresis (ultrasound therapy), and cryotherapy may be of some benefit. However, evidence supporting their success is not clear.[41]Green S, Buchbinder R, Hetrick S. Physiotherapy interventions for shoulder pain. Cochrane Database Syst Rev. 2003 Apr 22;(2):CD004258. https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD004258/full http://www.ncbi.nlm.nih.gov/pubmed/12804509?tool=bestpractice.com
A useful exercise that can be performed at the patient's home and with the therapist is known as the sleeper stretch, which works on improving internal rotation. In the lateral decubitus position (patient on side), with the affected shoulder down against the bed, the elbow is flexed 90° and the unaffected arm pushes it toward the bed. [Figure caption and citation for the preceding image starts]: Demonstration of sleeper stretch exerciseFrom the private collection of Matthew T. Provencher, MD, CDR MC USN and Lance E. LeClere, MD, LCDR MC USN; used with permission [Citation ends].
NSAID
Treatment recommended for SOME patients in selected patient group
As the initial stages of adhesive capsulitis are associated with an inflammatory process, early in the disease course a scheduled regimen of NSAIDs may provide symptomatic relief as well as decrease the severity of the disease.
They may provide additional symptomatic relief in those patients undergoing arthroscopic capsular release, providing there are no contraindications.
Primary options
ibuprofen: 200-400 mg orally every 4-6 hours when required, maximum 2400 mg/day
OR
meloxicam: 7.5 mg orally once or twice daily when required, maximum 15 mg/day
OR
naproxen: 500 mg orally initially, followed by 250 mg every 6-8 hours when required, maximum 1250 mg/day

Choose a patient group to see our recommendations
Please note that formulations/routes and doses may differ between drug names and brands, drug formularies, or locations. Treatment recommendations are specific to patient groups. See disclaimer
Use of this content is subject to our disclaimer