Approach
Although the presentation of decompression sickness may vary enormously, the mainstay of treatment is prompt recompression in a hyperbaric chamber.[1][7] While the patient is in transit to such a facility, administration of oxygen and fluid replacement is recommended.[38]
In the chamber, the patient is compressed to a prespecified depth and breathes 100% oxygen. The patient is returned to normal atmospheric pressure via a gradual, staged decompression. The goal is resolution of symptoms. The clinical outcome correlates with time to treatment though delayed recompression may still be of benefit if factors preclude immediate decompression.[39][40]
The management of barotrauma depends on its location (e.g., ear, lung, teeth). Nitrogen narcosis is immediately reversible by reduction of ambient pressure (i.e., ascent).[3][Figure caption and citation for the preceding image starts]: A typical multiplace hyperbaric chamberFrom the collection of Dr. Oliver Firth; used with permission [Citation ends].
Decompression sickness
Initial first aid treatment should be given according to accepted principles of basic and advanced life support. Recommendations on specific aspects of rescuing a submerged unresponsive compressed-gas diver are available.[41] The diver should be nursed horizontally (supine or in the recovery position), to prevent postural hypotension and enhance nitrogen washout.[38][42] To avoid further bubble provocation, nitrous oxide anesthesia should not be administered, and the diver should be encouraged to remain still.
Oxygen: prompt administration of 100% oxygen has been shown to improve clinical outcome.[43] This increases oxygen delivery to hypoxic tissues and speeds the rate of inert gas elimination. By reducing the partial pressure of inert gas in bubbles, diffusion into tissues is enhanced and bubble size diminished.[44]
Fluids: divers are prone to dehydration due to immersion diuresis, seasickness, and bubble-induced capillary leakage. Isotonic oral fluids can be given in a conscious patient with mild decompression illness. Otherwise, 1 to 2 liters of intravenous fluids during the first postinjury hour is recommended, followed by an infusion with the goal of normotension and urine output of 0.5 to 1.0 mL/kg/hour.[1]
Temperature control: wet divers are often cold and should be dried, as hypothermia will slow inert gas washout. Conversely, increased body temperature may encourage bubble formation.[45]
Recompression: the patient should be recompressed in a hyperbaric chamber as soon as is practically possible. A 95% probability of relief has been demonstrated if treatment is initiated within 30 minutes. This drops to 77% if the delay exceeds 6 hours.[46] While new evidence suggests a role for delayed recompression if prompt treatment is not feasible to travel from a remote dive location precludes timely intervention, whenever possible patients should be recompressed as quickly as possible.[40] To minimize the detrimental effect of continued bubble formation or expansion with decreased atmospheric pressure at altitude, transport to a suitable facility should ideally be via ground or by aircraft pressurized to sea level.[47] In the hyperacute setting, recompression may act to mechanically reduce bubble volume (Boyle’s law) and/or force gas back into solution (Henry’s law). In addition to reduction in bubble volume, hyperbaric oxygen’s modulation of systemic inflammatory response likely also plays a significant role, especially in more delayed presentations.[48]
Empirically derived recompression schedules (or "treatment tables") have been developed, which vary in their maximum depth (pressure), duration, and the breathing gas mixture used.
Breathing 100% oxygen while under pressure leads to:
Rapid elimination of inert gas
Inhibition of secondary inflammatory and reperfusion injury
Hyperoxygenation of ischemic tissues
Reduction of edema formation
Oxygen can cause pulmonary and neurologic toxicity at partial pressures exceeding 0.55 atmosphere absolute (ATA) and 1.5 ATA, respectively. A latent period prior to the onset of toxicity allows higher partial pressures to be used, with periodic "air breaks" introduced to minimize risk. Commonly used oxygen treatment tables include:
US Navy Treatment Table 6: the standard generally recommended for initial treatment.[3] Recompression to 2.8 ATA (60 feet, or 18 m) for 3 sessions of 20 minutes with 100% oxygen, interspersed with 5-minute air breaks, is followed by similar but longer cycles at 1.9 ATA (30 feet, or 9 m), with a total treatment time of 285 minutes. For severe or refractory cases, further "extensions" at 59 feet (18 m), or deeper excursions on different gas mixtures (e.g., helium-oxygen, Heliox), can be used. Limited data suggest that initial treatment with Heliox may reduce the number of follow-up recompression sessions required, although ultimate outcome is not altered.[49]
US Navy Treatment Table 5: a shortened version of US Navy Treatment Table 6, which is used in the treatment of cutaneous or pain-only symptoms (type I DCS). If full remission has not been achieved within 10 minutes of reaching 2.8 ATA, the table is converted to a US Navy Treatment Table 6.
Other tables are reserved for specific situations: for example, where oxygen is unavailable, or for saturation divers (US Navy Treatment Table 7).
Recurrent symptoms during recompression should prompt reconsideration of the treatment table, the ancillary clinical management, and sometimes the diagnosis. Follow-up treatments may be required to treat the sequelae of bubble damage, and are generally continued until complete resolution of symptoms has occurred, or no significant change is observed between two consecutive treatments (i.e., a "plateau" has been reached).
Ear barotrauma
Middle ear barotrauma of descent is treated by avoidance of all further pressure changes (e.g., diving, flying, forceful autoinflation) until resolution has occurred. The use of nasal or systemic decongestants is seldom warranted. Antibiotics are indicated only rarely, in cases of gross or developing infection.
For inner ear barotrauma, initial conservative measures are bed rest, head elevation, and minimization of perilymph pressure increases. The patient should avoid coughing, sneezing, equalizing, and any physical exertion (e.g., the use of stool softeners is recommended). If symptoms persist or deteriorate, operative intervention is considered. Oval or round window repair prevents further perilymph leakage and may improve vertigo, tinnitus, and hearing.[50]
Analgesics can be administered for pain relief.
Pulmonary barotrauma
Initial treatment of suspected pulmonary barotrauma should aim to minimize factors promoting further gas expansion or escape. Such factors include:
Ascent (in water, in a hyperbaric chamber, or to altitude)
Exertion
Coughing
Increased respiratory rate
Raised intra-abdominal pressure.
Treatment of the different manifestations of pulmonary barotrauma should be as follows.
Pulmonary tissue damage: 100% oxygen is administered to correct arterial hypoxemia, avoiding positive pressure ventilation where possible as this may exacerbate lung damage. Hemodynamic support may be required.[3]
Pneumothorax: this is managed according to standard protocols. Air embolism must be excluded. Mild cases may resolve with normobaric 100% oxygen. Depending on clinical severity, placement of a chest drain or emergency needle thoracostomy may be required. Pneumothorax should be definitively treated (i.e., chest tube placed) prior to recompression therapy to avoid precipitation of tension pneumothorax on decompression.[3] Similarly, if a pneumothorax is noted during recompression, it must be drained in the chamber, as it will otherwise re-expand on ascent. Use of a one-way Heimlich valve is preferred to an underwater seal drain, to minimize the risk of flooding the thoracic cavity with chamber pressure changes.
Mediastinal emphysema: if diagnosed, pneumothorax and air embolism should be excluded as their treatment takes precedence. If asymptomatic, rest and observation may suffice. Mild symptomatic cases may resolve with normobaric 100% oxygen. Recompression is only very rarely indicated.
Air embolism: treatment follows the principles of decompression illness. Prompt recompression is key. Head down positioning is no longer recommended. While in transit to a hyperbaric chamber, horizontal positioning of the patient helps reduce the risk of further embolism or emboli migration. Administration of 100% oxygen by close-fitting mask will help dissolve and dissipate emboli, treat hypoxia, reduce cerebral edema, and limit the acute inflammatory reaction. Particular preparations prior to chamber entry are required. Due to the risk of occult pneumothorax, femoral central venous lines are preferred to those in jugular or subclavian veins. Any pneumothorax must be drained with a chest tube before recompression, to avoid progression to a tension pneumothorax during hyperbaric exposure. Air in the endotracheal cuffs of intubated patients should be replaced with an equivalent amount of liquid (e.g., saline or distilled water) or monitored through pressure changes by staff to prevent loss of seal or overinflation. Myringotomy may be required in these patients if they are unable to equalize their middle ear spaces voluntarily during recompression treatment. In cerebral arterial gas embolism, patients can present with generalised seizures, which are treated similarly to seizures from any other cause. First-line anticonvulsants are intravenous lorazepam or rectal diazepam if there is no intravenous access. If seizures recur or fail to respond within 30 minutes, either a phenytoin or a phenobarbital infusion may be used.
Sinus barotrauma
Pressure changes should be avoided while the underlying sinus inflammation resolves. This may occur spontaneously, or require the use of local or systemic decongestants and intranasal corticosteroids. Analgesics can be administered for pain relief. Recurrent or refractory cases may need endoscopic exploration or surgery, to improve patency of the ostia or to remove obstructions such as polyps or redundant mucosal folds.
Other barotraumas
Avoidance of pressure changes until tissue damage has resolved is common to the treatment of all other barotraumas. Dental barotrauma requires analgesia and repair. Gastrointestinal barotrauma is rarely severe, but if gastric rupture occurs, stomach contents may enter the peritoneal cavity and surgical repair is imperative. Mask or suit barotraumas (mask/suit squeeze) will resolve spontaneously.
Analgesics can be administered for pain relief. Dental barotrauma is usually very painful and analgesics are generally required. These can also be used in sinus and mask/suit squeeze barotraumas, although acetaminophen alone is probably sufficient in the latter. Repair of dental defects/injuries may also be necessary.[Figure caption and citation for the preceding image starts]: Ocular barotrauma caused by "mask squeeze"From the collection of Dr. Phillipa Squires, BMJ Education; used with permission [Citation ends].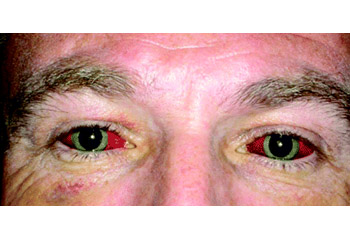
Nitrogen narcosis
This is entirely reversible by reduction of ambient pressure (i.e., ascent to shallow depths).[3] Persistent symptoms on the surface should not be attributed to nitrogen narcosis alone.
Use of this content is subject to our disclaimer