Treatment decisions for adolescent idiopathic scoliosis (AIS) are based on the initial deformity at presentation and rate of curve progression, as well as an overall assessment of the patient's growth potential.
The main goal of treatment is to prevent progression of the spinal deformity until the patient reaches skeletal maturity. Once the patient has reached skeletal maturity, the risk of curve progression decreases significantly. Treatment options for AIS include observational monitoring, bracing, or surgical spinal arthrodesis (fusion). The selection of treatment is based on the severity of the curve and the amount of growth remaining until skeletal maturity.
Screening scoliometer measurement <5° or standing coronal Cobb angle measurement ≤10°
These measurements allow a diagnosis of postural deformity to be made. No treatment or observational monitoring is necessary unless the patient or family identify worsening postural asymmetry or the patient develops symptoms to suggest the presence of another underlying cause for the spinal deformity.[1]Parent S, Newton PO, Wenger DR. Adolescent idiopathic scoliosis: etiology, anatomy, natural history, and bracing. Instr Course Lect. 2005;54:529-36.
http://www.ncbi.nlm.nih.gov/pubmed/15948477?tool=bestpractice.com
[2]Yaszay B, Newton PO. Idiopathic scoliosis. In: Weinstein SL, Flynn JM, Crawford HA, eds. Lovell and Winter's Pediatric Orthopaedics. 8th ed. Philadelphia: Wolters Kluwer, 2021:659-720.[13]Bunnell WP. The natural history of idiopathic scoliosis before skeletal maturity. Spine. 1986 Oct;11(8):773-6.
http://www.ncbi.nlm.nih.gov/pubmed/3810290?tool=bestpractice.com
[50]Weinstein SL, Dolan LA, Spratt KF, et al. Health and function of patients with untreated idiopathic scoliosis: a 50-year natural history study. JAMA. 2003 Feb 5;289(5):559-67.
https://jama.ama-assn.org/cgi/content/full/289/5/559
http://www.ncbi.nlm.nih.gov/pubmed/12578488?tool=bestpractice.com
[51]Bagnall KM, Beuerlein M, Johnson P, et al. Pineal transplantation after pinealectomy in young chickens has no effect on the development of scoliosis. Spine. 2001 May 1;26(9):1022-7.
http://www.ncbi.nlm.nih.gov/pubmed/11337620?tool=bestpractice.com
[52]Goldberg MS, Mayo NE, Poitras B, et al. The Ste-Justine Adolescent Idiopathic Scoliosis Cohort Study. Part II: Perception of health, self and body image, and participation in physical activities. Spine. 1994 Jul 15;19(14):1562-72.
http://www.ncbi.nlm.nih.gov/pubmed/7939992?tool=bestpractice.com
[53]Weinstein SL. Idiopathic scoliosis. Natural history. Spine. 1986 Oct;11(8):780-3.
http://www.ncbi.nlm.nih.gov/pubmed/3810292?tool=bestpractice.com
[54]Weinstein SL, Ponseti IV. Curve progression in idiopathic scoliosis. J Bone Joint Surg Am. 1983 Apr;65(4):447-55.
http://www.ncbi.nlm.nih.gov/pubmed/6833318?tool=bestpractice.com
[55]Weinstein SL, Zavala DC, Ponseti IV. Idiopathic scoliosis: long-term follow-up and prognosis in untreated patients. J Bone Joint Surg Am. 1981 Jun;63(5):702-12.
http://www.ncbi.nlm.nih.gov/pubmed/6453874?tool=bestpractice.com
The patient should be advised to maintain a regular fitness routine, specifically towards developing improved core strength and conditioning.
Standing coronal Cobb angle measurement of 11° to 20°
Observational monitoring with follow-up standing PA and lateral scoliosis x-rays should be undertaken at 4- to 12-month intervals (depending on the estimated rate of growth and remaining growth potential at the time of evaluation).[1]Parent S, Newton PO, Wenger DR. Adolescent idiopathic scoliosis: etiology, anatomy, natural history, and bracing. Instr Course Lect. 2005;54:529-36.
http://www.ncbi.nlm.nih.gov/pubmed/15948477?tool=bestpractice.com
[2]Yaszay B, Newton PO. Idiopathic scoliosis. In: Weinstein SL, Flynn JM, Crawford HA, eds. Lovell and Winter's Pediatric Orthopaedics. 8th ed. Philadelphia: Wolters Kluwer, 2021:659-720.[13]Bunnell WP. The natural history of idiopathic scoliosis before skeletal maturity. Spine. 1986 Oct;11(8):773-6.
http://www.ncbi.nlm.nih.gov/pubmed/3810290?tool=bestpractice.com
[50]Weinstein SL, Dolan LA, Spratt KF, et al. Health and function of patients with untreated idiopathic scoliosis: a 50-year natural history study. JAMA. 2003 Feb 5;289(5):559-67.
https://jama.ama-assn.org/cgi/content/full/289/5/559
http://www.ncbi.nlm.nih.gov/pubmed/12578488?tool=bestpractice.com
[51]Bagnall KM, Beuerlein M, Johnson P, et al. Pineal transplantation after pinealectomy in young chickens has no effect on the development of scoliosis. Spine. 2001 May 1;26(9):1022-7.
http://www.ncbi.nlm.nih.gov/pubmed/11337620?tool=bestpractice.com
[52]Goldberg MS, Mayo NE, Poitras B, et al. The Ste-Justine Adolescent Idiopathic Scoliosis Cohort Study. Part II: Perception of health, self and body image, and participation in physical activities. Spine. 1994 Jul 15;19(14):1562-72.
http://www.ncbi.nlm.nih.gov/pubmed/7939992?tool=bestpractice.com
[53]Weinstein SL. Idiopathic scoliosis. Natural history. Spine. 1986 Oct;11(8):780-3.
http://www.ncbi.nlm.nih.gov/pubmed/3810292?tool=bestpractice.com
[54]Weinstein SL, Ponseti IV. Curve progression in idiopathic scoliosis. J Bone Joint Surg Am. 1983 Apr;65(4):447-55.
http://www.ncbi.nlm.nih.gov/pubmed/6833318?tool=bestpractice.com
[55]Weinstein SL, Zavala DC, Ponseti IV. Idiopathic scoliosis: long-term follow-up and prognosis in untreated patients. J Bone Joint Surg Am. 1981 Jun;63(5):702-12.
http://www.ncbi.nlm.nih.gov/pubmed/6453874?tool=bestpractice.com
The patient should be advised to maintain a regular fitness routine, specifically towards developing improved core strength and conditioning.
Standing coronal Cobb angle measurement of 21° to 45°
Brace treatment has traditionally been used in patients with a curve of >21°.[1]Parent S, Newton PO, Wenger DR. Adolescent idiopathic scoliosis: etiology, anatomy, natural history, and bracing. Instr Course Lect. 2005;54:529-36.
http://www.ncbi.nlm.nih.gov/pubmed/15948477?tool=bestpractice.com
[2]Yaszay B, Newton PO. Idiopathic scoliosis. In: Weinstein SL, Flynn JM, Crawford HA, eds. Lovell and Winter's Pediatric Orthopaedics. 8th ed. Philadelphia: Wolters Kluwer, 2021:659-720. Many brace options are available, and the specific type of orthotic used varies between surgeons and from country to country.[56]Sponseller PD. Bracing for adolescent idiopathic scoliosis in practice today. J Pediatr Orthop. 2011 Jan-Feb;31(1 Suppl):S53-60.
http://www.ncbi.nlm.nih.gov/pubmed/21173620?tool=bestpractice.com
Braces commonly used in the US are the Boston and Rosenberger braces and the Charleston bending brace.
Several brace-wearing schedules have also been proposed, ranging from 23 hours per day to nighttime-only bracing. While some studies have supported a dose-dependent relationship between brace wearing and curve progression, it is still unclear which brace-wearing schedule provides the most reliable outcome. The International Scientific Society on Scoliosis Orthopaedic and Rehabilitation Treatment (SOSORT) consensus supports the use of an 18-hour-per-day bracing schedule.[32]Negrini S, Donzelli S, Aulisa AG, et al. 2016 SOSORT guidelines: orthopaedic and rehabilitation treatment of idiopathic scoliosis during growth. Scoliosis Spinal Disord. 2018;13:3.
https://www.doi.org/10.1186/s13013-017-0145-8
http://www.ncbi.nlm.nih.gov/pubmed/29435499?tool=bestpractice.com
Other organisations have also attempted to develop 'Consensus of Care' statements and guidelines in an effort to standardise scoliosis brace treatment protocols.[32]Negrini S, Donzelli S, Aulisa AG, et al. 2016 SOSORT guidelines: orthopaedic and rehabilitation treatment of idiopathic scoliosis during growth. Scoliosis Spinal Disord. 2018;13:3.
https://www.doi.org/10.1186/s13013-017-0145-8
http://www.ncbi.nlm.nih.gov/pubmed/29435499?tool=bestpractice.com
[57]Kotwicki T, Durmala J, Czaprowski D, et al. Conservative management of idiopathic scoliosis: guidelines based on SOSORT 2006 Consensus. Ortop Traumatol Rehabil. 2009 Sep-Oct;11(5):379-95.
http://www.ncbi.nlm.nih.gov/pubmed/19920281?tool=bestpractice.com
[58]Roye BD, Simhon ME, Matsumoto H, et al. Establishing consensus on the best practice guidelines for the use of bracing in adolescent idiopathic scoliosis. Spine Deform. 2020 Aug;8(4):597-604.
http://www.ncbi.nlm.nih.gov/pubmed/32026441?tool=bestpractice.com
The goal of brace therapy is to prevent curve progression until skeletal maturity, at which time the risk of further curve progression significantly reduces. Data from the BrAIST (Bracing in Adolescent Idiopathic Scoliosis Trial) trial have shown a significantly lower risk of curve progression in patients with AIS who wore a brace compared with those who did not.[45]Weinstein SL, Dolan LA, Wright JG, et al. Effects of bracing in adolescents with idiopathic scoliosis. N Engl J Med. 2013 Oct 17;369(16):1512-21.
https://www.doi.org/10.1056/NEJMoa1307337
http://www.ncbi.nlm.nih.gov/pubmed/24047455?tool=bestpractice.com
One Cochrane review concluded that all of the included studies consistently showed that bracing in AIS prevented curve progression, including 7 separate studies that included a total of 662 participants.[59]Negrini S, Minozzi S, Bettany-Saltikov J, et al. Braces for idiopathic scoliosis in adolescents. Cochrane Database Syst Rev. 2015 Jun 18;(6):CD006850.
https://onlinelibrary.wiley.com/doi/10.1002/14651858.CD006850.pub3/full
http://www.ncbi.nlm.nih.gov/pubmed/26086959?tool=bestpractice.com
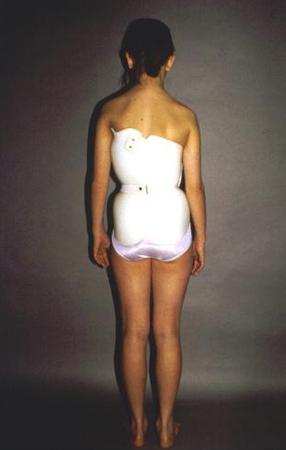
The patient should be advised to maintain a regular fitness routine, specifically towards developing improved core strength and conditioning.[Figure caption and citation for the preceding image starts]: Typical thoracic-lumbar-sacral orthosis (TLSO) scoliosis braceWeinstein SL, et al. Adolescent idiopathic scoliosis. Lancet. 2008;371:1527-1537. Used with permission [Citation ends].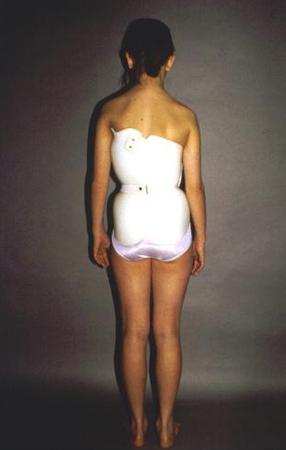
Standing coronal Cobb angle measurement of >45°
Due to risk of further curve progression and associated morbidity as an adult, the treatment recommended for this group of patients is to proceed with surgical spinal arthrodesis. Spinal arthrodesis with instrumentation serves several treatment objectives, including achievement of maximal deformity correction, improvement in appearance with trunk balancing, cessation of continued curve progression, and reduction of both short- and long-term complications related to the spinal deformity.[60]Dickson JH, Mirkovic S, Noble PC, et al. Results of operative treatment of idiopathic scoliosis in adults. J Bone Joint Surg Am. 1995 Apr;77(4):513-23.
http://www.ncbi.nlm.nih.gov/pubmed/7713967?tool=bestpractice.com
The choice of surgical approach and instrumentation technique is dictated by the characteristics of the deformity (e.g., location of the curve apex), degree of spinal flexibility, and surgeon preference.[60]Dickson JH, Mirkovic S, Noble PC, et al. Results of operative treatment of idiopathic scoliosis in adults. J Bone Joint Surg Am. 1995 Apr;77(4):513-23.
http://www.ncbi.nlm.nih.gov/pubmed/7713967?tool=bestpractice.com
Most deformities can be addressed with a posterior approach that has traditionally been the optimal technique for surgical arthrodesis of the scoliotic spine.[61]Kim YJ, Lenke LG, Kim J, et al. Comparative analysis of pedicle screw versus hybrid instrumentation in posterior spinal fusion of adolescent idiopathic scoliosis. Spine. 2006 Feb 1;31(3):291-8.
http://www.ncbi.nlm.nih.gov/pubmed/16449901?tool=bestpractice.com
[62]Lenke LG. Debate: Resolved, a 55 degrees right thoracic adolescent idiopathic scoliotic curve should be treated by posterior spinal fusion and segmental instrumentation using thoracic pedicle screws: Pro: Thoracic pedicle screws should be used to treat a 55 degrees right thoracic adolescent idiopathic scoliosis. J Pediatr Orthop. 2004 May-Jun;24(3):329-34.
http://www.ncbi.nlm.nih.gov/pubmed/15105732?tool=bestpractice.com
[63]Suk SI, Lee CK, Kim WJ, et al. Segmental pedicle screw fixation in the treatment of thoracic idiopathic scoliosis. Spine. 1995 Jun 15;20(12):1399-405.
http://www.ncbi.nlm.nih.gov/pubmed/7676339?tool=bestpractice.com
[64]Suk SI, Lee SM, Chung ER, et al. Selective thoracic fusion with segmental pedicle screw fixation in the treatment of thoracic idiopathic scoliosis: more than 5-year follow-up. Spine. 2005 Jul 15;30(14):1602-9.
http://www.ncbi.nlm.nih.gov/pubmed/16025028?tool=bestpractice.com
Some surgeons use an anterior approach with the belief that the deformity can be corrected with a lower number of fused levels.[65]Muschik MT, Kimmich H, Demmel T. Comparison of anterior and posterior double-rod instrumentation for thoracic idiopathic scoliosis: results of 141 patients. Eur Spine J. 2006 Jul;15(7):1128-38.
http://www.ncbi.nlm.nih.gov/pubmed/16470398?tool=bestpractice.com
[66]Turi M, Johnston CE 2nd, Richards BS. Anterior correction of idiopathic scoliosis using TSRH instrumentation. Spine. 1993 Mar 15;18(4):417-22.
http://www.ncbi.nlm.nih.gov/pubmed/8469999?tool=bestpractice.com
[67]Newton PO. The use of video-assisted thoracoscopic surgery in the treatment of adolescent idiopathic scoliosis. Instr Course Lect. 2005;54:551-8.
http://www.ncbi.nlm.nih.gov/pubmed/15948480?tool=bestpractice.com
[68]Newton PO, Faro FD, Gollogly S, et al. Results of preoperative pulmonary function testing of adolescents with idiopathic scoliosis. A study of six hundred and thirty-one patients. J Bone Joint Surg Am. 2005 Sep;87(9):1937-46.
http://www.ncbi.nlm.nih.gov/pubmed/16140807?tool=bestpractice.com
[69]Newton PO, Marks M, Faro F, et al. Use of video-assisted thoracoscopic surgery to reduce perioperative morbidity in scoliosis surgery. Spine. 2003 Oct 15;28(20):S249-54.
http://www.ncbi.nlm.nih.gov/pubmed/14560200?tool=bestpractice.com
[70]Newton PO, Parent S, Marks M, et al. Prospective evaluation of 50 consecutive scoliosis patients surgically treated with thoracoscopic anterior instrumentation. Spine. 2005 Sep 1;30(17 Suppl):S100-9.
http://www.ncbi.nlm.nih.gov/pubmed/16138057?tool=bestpractice.com
[71]Newton PO, Wenger DR, Mubarak SJ, et al. Anterior release and fusion in pediatric spinal deformity. A comparison of early outcome and cost of thoracoscopic and open thoracotomy approaches. Spine. 1997 Jun 15;22(12):1398-406.
http://www.ncbi.nlm.nih.gov/pubmed/9201845?tool=bestpractice.com
[72]Newton PO, White KK, Faro F, et al. The success of thoracoscopic anterior fusion in a consecutive series of 112 pediatric spinal deformity cases. Spine. 2005 Feb 15;30(4):392-8.
http://www.ncbi.nlm.nih.gov/pubmed/15706335?tool=bestpractice.com
[73]Reddi V, Clarke DV Jr, Arlet V. Anterior thoracoscopic instrumentation in adolescent idiopathic scoliosis: a systematic review. Spine (Phila Pa 1976). 2008 Aug 15;33(18):1986-94.
http://www.ncbi.nlm.nih.gov/pubmed/18665023?tool=bestpractice.com
However, this approach has a higher incidence of implant failure and pseudarthrosis compared with the posterior approach, and has been associated with a risk of pulmonary complications secondary to the need for 'single lung' anaesthesia during the procedure.[74]Betz RR, Harms J, Clements DH 3rd, et al. Comparison of anterior and posterior instrumentation for correction of adolescent thoracic idiopathic scoliosis. Spine. 1999 Feb 1;24(3):225-39.
http://www.ncbi.nlm.nih.gov/pubmed/10025017?tool=bestpractice.com
[75]Lenke LG. Anterior endoscopic discectomy and fusion for adolescent idiopathic scoliosis. Spine. 2003 Aug 1;28(15 Suppl):S36-43.
http://www.ncbi.nlm.nih.gov/pubmed/12897472?tool=bestpractice.com
[76]Lowe TG, Alongi PR, Smith DA, et al. Anterior single rod instrumentation for thoracolumbar adolescent idiopathic scoliosis with and without the use of structural interbody support. Spine. 2003 Aug 1;28(15 Suppl):S36-43.
http://www.ncbi.nlm.nih.gov/pubmed/14520036?tool=bestpractice.com
The patient should be advised to maintain a regular fitness routine, specifically towards developing improved core strength and conditioning.[Figure caption and citation for the preceding image starts]: Posteroanterior scoliosis radiograph of a 13-year-old girl with a 49° right thoracic curvature with apex at the T9-T10 disc spaceFrom the collection of Stuart Weinstein, MD, University of Iowa; used with permission [Citation ends]. [Figure caption and citation for the preceding image starts]: Lateral scoliosis radiograph of a 13-year-old girl with a 49° right thoracic curvatureFrom the collection of Stuart Weinstein, MD, University of Iowa; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Lateral scoliosis radiograph of a 13-year-old girl with a 49° right thoracic curvatureFrom the collection of Stuart Weinstein, MD, University of Iowa; used with permission [Citation ends]. [Figure caption and citation for the preceding image starts]: Thirteen-year-old girl post-posterior spinal instrumentation and fusion for progressive scoliosisFrom the collection of Stuart Weinstein, MD, University of Iowa; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Thirteen-year-old girl post-posterior spinal instrumentation and fusion for progressive scoliosisFrom the collection of Stuart Weinstein, MD, University of Iowa; used with permission [Citation ends]. [Figure caption and citation for the preceding image starts]: Thirteen-year-old girl post-posterior spinal instrumentation and fusion for progressive scoliosisFrom the collection of Stuart Weinstein, MD, University of Iowa; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Thirteen-year-old girl post-posterior spinal instrumentation and fusion for progressive scoliosisFrom the collection of Stuart Weinstein, MD, University of Iowa; used with permission [Citation ends].
 [Figure caption and citation for the preceding image starts]: Lateral scoliosis radiograph of a 13-year-old girl with a 49° right thoracic curvatureFrom the collection of Stuart Weinstein, MD, University of Iowa; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Lateral scoliosis radiograph of a 13-year-old girl with a 49° right thoracic curvatureFrom the collection of Stuart Weinstein, MD, University of Iowa; used with permission [Citation ends]. [Figure caption and citation for the preceding image starts]: Thirteen-year-old girl post-posterior spinal instrumentation and fusion for progressive scoliosisFrom the collection of Stuart Weinstein, MD, University of Iowa; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Thirteen-year-old girl post-posterior spinal instrumentation and fusion for progressive scoliosisFrom the collection of Stuart Weinstein, MD, University of Iowa; used with permission [Citation ends]. [Figure caption and citation for the preceding image starts]: Thirteen-year-old girl post-posterior spinal instrumentation and fusion for progressive scoliosisFrom the collection of Stuart Weinstein, MD, University of Iowa; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Thirteen-year-old girl post-posterior spinal instrumentation and fusion for progressive scoliosisFrom the collection of Stuart Weinstein, MD, University of Iowa; used with permission [Citation ends].