Urgent considerations
See Differentials for more details
Acute stroke
Patients with acute stroke require urgent brain imaging to distinguish between ischaemic stroke, intracerebral haemorrhage, and subdural haematoma. Immediate non-contrast CT effectively excludes intracranial haemorrhage and may detect signs of ischaemic stroke. MRI is also effective for this purpose.[19]
Acute ischaemic stroke requires urgent treatment (e.g., intravenous thrombolysis) or endovascular therapy (e.g., mechanical thrombectomy).[18][19][21][22] Sometimes improving blood flow to ischaemic tissue that is not yet infarcted can restore tissue function and result in resolution of aphasia, even many hours to days after stroke onset.[30] Hypoglycaemia may mimic acute stroke therefore blood glucose levels should be tested in all patients.[19][Figure caption and citation for the preceding image starts]: Diffusion-weighted image (top left) and perfusion-weighted image (top right) at day 1 of stroke; arrow points to area of hypoperfusion (blue). Lower panel shows corresponding views at day 2From the collection of Dr Argye E. Hillis; used with permission [Citation ends].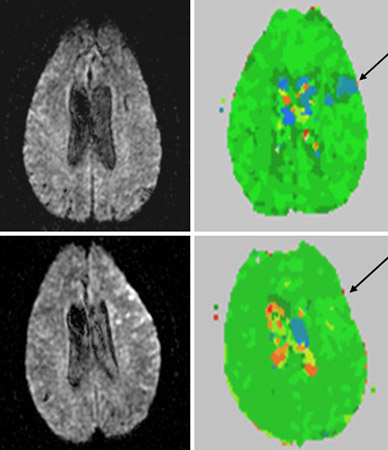
Intracerebral haemorrhage
Must be recognised immediately to prevent increased intracranial pressure and possible herniation that can ensue over the next few hours or days. The patient’s neurological status must be monitored closely for any signs of deterioration. Blood pressure (BP) is frequently elevated at presentation.
The European Stroke Organisation recommends that in patients with hyperacute (<6 hours) intracerebral haemorrhage, systolic BP should be lowered to below 140 mmHg (and kept above 110 mmHg) to reduce haematoma expansion.[36]
In patients with spontaneous intracerebral haemorrhage of mild to moderate severity presenting with systolic BP between 150 mmHg and 220 mmHg, American Heart Association (AHA)/American Stroke Association (ASA) guidelines recommend lowering the systolic BP to a target of 140 mmHg, with the goal of maintaining it in the range of 130 mmHg to 150 mmHg.[37]
If the patient’s level of consciousness deteriorates, tracheal intubation for airway protection should be considered.
Subarachnoid haemorrhage
Requires immediate search for an aneurysm and treatment if indicated. Also prevention or treatment of vasospasm. Blood pressure must be carefully controlled to balance the risk of hypertension-related bleeding with the maintenance of cerebral perfusion pressure.
Herpes encephalitis
Must be recognised immediately to limit the extent of permanent brain damage. Any rapid-onset fluent aphasia accompanied by fever, neck stiffness, and/or nausea and vomiting should be treated as herpes encephalitis with intravenous acyclovir until proven otherwise. After starting treatment, a lumbar puncture is performed to distinguish herpes encephalitis from subarachnoid haemorrhage or other infectious causes (e.g., Lyme disease, West Nile, toxoplasmosis) that require different treatments.
Wernicke's encephalopathy
Wernicke encephalopathy, caused by thiamine deficiency, often causes relatively acute-onset confabulation that can sound much like aphasia. However, it is generally accompanied by ophthalmoplegia, nystagmus, and ataxia. Intravenous thiamine should be administered before glucose if thiamine deficiency is suspected (e.g., in people with alcohol use disorder or in the presence of any of the associated symptoms of Korsakoff's dementia) to prevent permanent injury to the mammillary bodies.
Use of this content is subject to our disclaimer