Complications
Post-traumatic endophthalmitis is a sight‐threatening emergency that requires prompt diagnosis and treatment.
Signs include marked inflammation with fibrin, hypopyon (pus in the eye), vitreous infiltration, and corneal opacification.
Risk factors include penetrating injuries, retained intra-ocular foreign bodies, rural settings, dirty wounds, rupture of the lens capsule, and lengthy delay until primary surgical repair.[52]
The microbial agents most often involved are coagulase-negative Staphylococci, Streptococci, and Bacillus cereus. B cereus accounts for 25% of cases and occurs in soil-contaminated injuries.[18]
Treatment is with intravitreal and systemic antibiotics.[76] One Cochrane review found that vitrectomy offers no advantage over standard treatment of intra-vitreal antibiotics alone.[77]
Prophylaxis should be considered in patients with two or more risk factors.
These occur most often in adolescent and young men following motor vehicle collisions, assaults, or sports-related injuries.
They may be associated with intracranial and ocular injuries.
Common signs of orbital fracture include peri-ocular ecchymosis, diplopia, decreased sensation in the distribution of the infra-orbital nerve, and orbital emphysema.
Imaging of the orbit with computed tomography should be performed to localise the fracture and identify associated injuries.
Incidence is estimated at 0.2% after penetrating trauma.[78]
Clinical features include granulomatous anterior uveitis, moderate to severe vitritis, inflammation of the ciliary body, choroiditis, peripapillary choroidal atrophy, and optic nerve oedema.[79][80][81]
Prompt aggressive corticosteroid or immunosuppressive therapy is required to preserve the vision once the condition is diagnosed.
In cases with severely injured eyes, all efforts should be made to try to save a traumatised eye and avoid primary evisceration or enucleation.[82][83][84]
Primary evisceration or enucleation may be used when surgical repair cannot be performed or for patients who have panophthalmitis.[85]
Inert foreign bodies, such as stone, glass, sand, porcelain, plastic, and silica, are well tolerated. No treatment is necessary unless the visual axis is affected.
Reactive foreign bodies include zinc, iron, copper, and aluminium.
Aluminium and zinc particles may initiate a significant inflammatory reaction with pre-retinal and vitreous fibrosis that can lead to tractional retinal detachment and phthisis bulbi.
Pure copper particles may cause acute chalcosis with severe inflammation and loss of the eye.[86]
Copper alloy particles with less than 85% copper concentration can cause chronic chalcosis characterised by copper deposition in the basement membranes.
Iron particles are often deposited in the iris sphincter and dilator muscle, lens epithelium, non-pigmented ciliary epithelium, retinal pigment epithelium, and retina, and cause siderosis.[87]
Long-term complications of severe burns.
Defined as separation of the longitudinal muscle from the radial ciliary muscle at the level of the scleral spur.
Gonioscopy examination will show widening of the ciliary body band, and intra-ocular pressure (IOP) may be elevated.
May require lowering of IOP to avoid optic nerve damage.
Prolonged intra-ocular hypertension (>22 mmHg) may result in optic nerve damage and possible loss of sight.
This may follow an intra-ocular foreign body.
Other risk factors for retinal detachment include a scleral or corneoscleral entry wound, preoperative retinal detachment, and the size and location of any intra-ocular foreign body.[62]
Pars plana vitrectomy or scleral buckle may be required.
A traumatic angiopathic retinopathy (typically bilateral) that may appear within the first 2 days following severe trauma.
Depending on the extent of the macular area involved, visual acuity may be affected.
Dilated fundus examination shows large cotton-wool spots, a dilated and tortuous vasculature, haemorrhages, and retinal oedema, located most commonly around the optic disc.
The iris adheres to either the cornea (anterior synechia) or lens (posterior synechia). Synechiae can be caused by ocular trauma, may lead to certain types of glaucoma, and is visible on slit-lamp examination.
Long-term complications of severe burns.
May follow choroidal rupture.
Laser photo-coagulation, photo-dynamic therapy, and anti-vascular endothelial growth factor injections are indicated, depending on the location of the lesion.[88]
A concussion cataract is an acute lens opacity that may follow blunt trauma. It can be progressive, requiring surgical removal.
Slit-lamp examination may show the cataract, with or without anterior capsule damage, lens subluxation or dislocation, deep anterior chamber, iridodonesis, or prolapse of the anterior hyaloid in the anterior chamber.
Ocular chemical penetration may also lead to secondary glaucoma owing to trabecular meshwork scarring and reduced aqueous outflow.
A shrunken non-functional eye may occur after severe burns.
Rarely, increased intra-ocular pressure and/or secondary haemorrhage 3-5 days after a hyphaema may complicate the bleed and result in corneal or optic nerve damage.
This is the most common cause of vision loss after successful retinal detachment surgery and it has been reported to occur in up to 40% of eyes after severe trauma.[89]
Formation depends on the type of injury.
Proliferative vitreo-retinopathy presents earliest after perforating injuries (1 month), followed by ruptures (2 month), and injury from an intra-ocular foreign body (3 months).[89]
Other risks factors include vitreous haemorrhage, size of retinal break and extent of retinal detachment, extensive cryopexy, and early silicone oil removal.[90][91][92]
A rare but serious complication of eye surgery. Immediate apposition of the wound lips, regardless of the method used, may be helpful to save the eye.
Following blunt trauma, the supporting lens zonules may rupture partially or completely, causing a lens subluxation or complete dislocation, respectively.
This may follow eye trauma and, if present, frequent follow-up is usually required.
The source of the blood may be any intra-ocular tissue, blood vessels of iris, ciliary body, retina, or choroid.
Can occur following blunt trauma to the eye and is defined as separation of the ciliary body from its insertion to the scleral spur.
Cyclodialysis enables direct communication between the anterior chamber and suprachoroidal space with subsequent increase of the uveoscleral outflow and hypotony.
Gonioscopy shows a cleft between the ciliary body and scleral spur; the size of the defect is not correlated with the degree of hypotony (low intra-ocular pressure).
It requires treatment with cycloplegic eye drops to deepen the anterior chamber and prevent synechia formation. In cases that do not resolve with medical treatment, closure may be attempted using argon laser or surgery.[93][94][95]
Bruch membrane has little elasticity and its stretch during antero-posterior compression causes ruptures in addition to retinal pigment epithelium changes and choriocapillaris.
Prognosis is good unless the lesion runs directly through the macula.[96]
Choroidal ruptures may be single or multiple, and may have a characteristic shape concentric to the optic disc.
Their presence increases the likelihood of other serious pathologies.[97]
Visual loss may be immediate if the rupture involves the macula or may be secondary to choroidal neovascularisation as a late complication.
Induced by blunt ocular trauma and caused by the disruption of the outer segment of photoreceptors.[98]
Presents with decreased vision.
Dilated fundus examination shows sheen-like retinal whitening a few hours after injury.
Commotio retinae in the posterior pole is called Berlin oedema.
If there is foveal involvement, a cherry red spot may appear.
The prognosis is usually good with recovery in 3 to 4 weeks. Visual outcome may be limited by associated macular pigment epitheliopathy, choroidal rupture, or macular-hole formation.
Defined as a retinal lesion. Occurs following high-speed missile injuries to the orbit.
Dilated fundus examination may show large areas of choroidal and retinal rupture and necrosis combined with extensive sub-retinal and retinal haemorrhages.
After resolution of the acute injury, extensive scar tissue and pigmentary changes may appear.
Visual loss may be due to macular involvement, which is frequent.
Chorio-retinal scar formation often prevents secondary retinal detachment.[99]
May be caused by severe open or closed trauma to the globe.
Characteristic signs include pain, elevated intra-ocular pressure, a dark crescent inside the eye with absence of the red reflex, uveal tissue prolapse, and fresh blood streaming from inside the eye.
Produced by a combination of mechanisms, including contusion necrosis and vitreous traction.
Post-traumatic macular hole may appear immediately following the trauma or may be associated with severe Berlin oedema, sub-retinal macular haemorrhage caused by choroidal rupture, or severe cystoid macular oedema.
Post-traumatic macular hole is often oval, whereas idiopathic macular hole is round. Tends to close spontaneously compared with idiopathic hole.[100]
Surgery (vitrectomy, internal limiting-membrane peeling, and gas tamponade) is highly successful, even if other macular pathology is present.[101]
Occurs following high-speed missile injuries to the orbit.
Dilated fundus examination may show large areas of choroidal and retinal rupture and necrosis combined with extensive sub-retinal and retinal haemorrhages.
After resolution of the acute injury, extensive scar tissue and pigmentary changes may appear.
Visual loss may be due to macular involvement, which is frequent.
Appears in the first 24 hours after injury.
It presents with dull, aching pain, photophobia, increased tearing, and blurred vision.
Slit-lamp examination shows white blood cells and flare in the anterior chamber and peri-limbal conjunctival injection.
Can be determined by direct visualisation, but slit-lamp examination looking for a corneal infiltrate with fluorescein staining should be used to confirm the diagnosis.[Figure caption and citation for the preceding image starts]: Corneal ulcer seen with fluorescein stainUsed with kind permission from Drs Smith, Severn, and Clarke [Citation ends].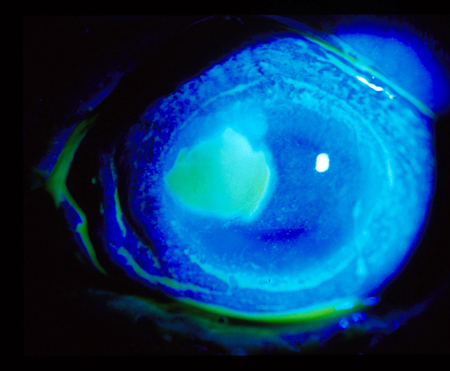
Diagnosis is made by identification of an epithelial defect with underlying stromal infiltrate. There may be associated anterior chamber reaction and hypopyon formation.
If suspected, the patient should be referred to an ophthalmologist for diagnosis and management.
Patients who have a corneal abrasion with infected material (farm instruments, vegetable matter) are at risk of developing infectious (bacterial) keratitis.
Patients in whom such a mechanism is known or suspected should be monitored daily for corneal infiltrate or ulceration.
Use of this content is subject to our disclaimer