Urgent considerations
See Differentials for more details
Urgent (same-day) ophthalmologist consultation is required for all patients with:
Sudden symptom onset (within minutes or hours)
Symptoms associated with new-onset neurological symptoms (such as diplopia, weakness, vertigo, or dysarthria)
Symptoms resulting from trauma
Symptoms associated with new-onset pain, redness, or orbital signs.
These patients require initial accident and emergency department assessment and same-day inpatient or outpatient ophthalmology review. Failure to obtain timely evaluation and treatment may result in permanent vision loss and systemic morbidity.
Acute angle-closure glaucoma
Typically presents as acute monocular loss of vision, severe periorbital pain, elevated intra-ocular pressure, and occasionally abdominal pain with nausea and vomiting.[16]
Treatment with medical agents alone is usually inadequate, and surgical consultation is required. Patients with abdominal symptoms often have a work-up and sometimes treatment (e.g., appendicectomy) for those symptoms, which may lead to delayed diagnosis and permanent vision loss.
Retinal detachment
Retinal detachment can cause visual field loss with unaffected central vision. This is a surgical emergency. Patients may have flashes, floaters, or peripheral vision loss. Once the fovea detaches, the likelihood of restoring good central vision declines rapidly.[32]
Immediate surgical consultation is required, and urgent surgical intervention needed, to avoid permanent vision loss.
Retinal vascular occlusion
May produce similar symptoms to retinal detachment.[19][20] Differentiation of the two conditions is made by careful dilated ophthalmoscopy.
In acute central retinal artery occlusion, intravenous tissue-type plasminogen activator (tPA) may be a treatment option for select patients who present at early time points.[33]
In retinal vein occlusions, treatment includes anti-vascular endothelial growth factor (VEGF) agents, laser photocoagulation, and intravitreal corticosteroids.[25][26][34]
Corneal ulcer
Central corneal ulceration presents with vision loss and painful red eye. [Figure caption and citation for the preceding image starts]: Corneal ulcer with epithelial defect and stromal infiltrateFrom Dr Prem S. Subramanian's personal collection; used with permission [Citation ends].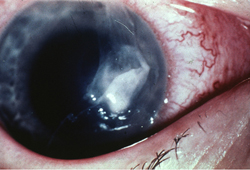
Neurotrophic corneas (from previous herpetic infection) may be painless.
Urgent inpatient medical therapy is often needed to prevent corneal perforation and loss of ocular contents.[12]
Pituitary apoplexy
Acute vision loss with severe headache and ocular motility disorder may indicate sudden haemorrhagic pituitary adenoma expansion.[35] The haemorrhage may be demonstrated by head/brain computerised tomography or magnetic resonance imaging.[36][Figure caption and citation for the preceding image starts]: Pituitary apoplexy: large suprasellar mass with heterogeneous gadolinium enhancement (T1-weighted MRI)From Dr Prem S. Subramanian's personal collection; used with permission [Citation ends].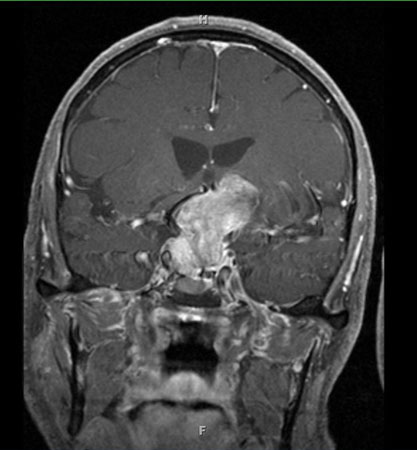
Pituitary apoplexy may be associated with acute hypopituitarism with resulting adrenocorticotropic hormone and cortisol deficiency.[37][38]
Emergent neurosurgical consultation, with admission to the hospital, may be required. Patients with signs and symptoms suggestive of acute hypopituitarism require urgent administration of parenteral corticosteroids along with intravenous fluid replacement.
Arteritic anterior ischaemic optic neuropathy/giant cell arteritis (GCA)
GCA typically presents with sudden, severe, monocular visual loss in patients age ≥50 years.[39][40] Systemic symptoms include weight loss, scalp tenderness, jaw claudication, proximal muscle weakness, and headache. Erythrocyte sedimentation rate and C-reactive protein are typically markedly elevated, although they may be normal in rare circumstances of biopsy-proven disease. Sequential second eye involvement may occur without treatment.
Immediate treatment with high-dose oral or intravenous corticosteroids is recommended to avoid second eye involvement and other vascular complications such as myocardial infarction.
Stroke
Stroke manifestations can include the presence of homonymous field defects or central vision loss, which require urgent neurological consultation.[41][Figure caption and citation for the preceding image starts]: Right eye of patient with homonymous field defectFrom Dr Prem S. Subramanian's personal collection; used with permission [Citation ends].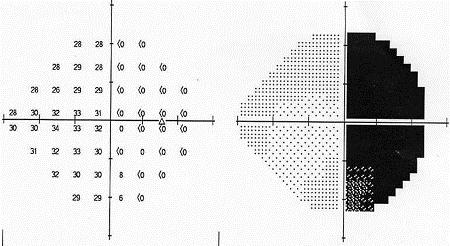 [Figure caption and citation for the preceding image starts]: Left eye of patient with homonymous field defectFrom Dr Prem S. Subramanian's personal collection; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Left eye of patient with homonymous field defectFrom Dr Prem S. Subramanian's personal collection; used with permission [Citation ends].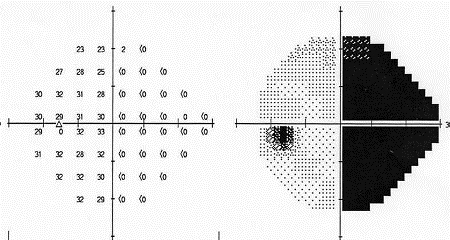
Uveitis
Symptoms of uveitis (posterior, anterior, or panuveitis) develop over days rather than hours and usually manifest as photophobia, ocular redness, and eye pain. Symptoms are typically monocular, but can be binocular. Symptoms may resemble those of conjunctivitis.
Pain is typically relieved with topical cycloplegic agents and topical corticosteroids. Treatment may be prolonged depending on the degree of inflammation.
Prompt ophthalmology referral for corticosteroid or other immunomodulating treatment is essential to prevent long-term consequences, such as glaucoma.
Post-operative endophthalmitis
Patients may present with a painful, red eye with acute vision loss after recent cataract surgery (<1 month) or at any time after other intraocular surgery or injection.
Trauma
All patients with head or orbital trauma require assessment of visual acuity and motility after any life-threatening injuries are stabilised. Visual acuity at presentation is predictive of final outcome.[42]
Removal of penetrating objects in accident and emergency departments increases the risk of displacement; instead, consider shielding these objects.
Open globe trauma mandates urgent ophthalmology-led surgical intervention.[43]
Recent blunt trauma may cause retrobulbar haemorrhage, which can cause elevated intra-ocular pressure and intra-ocular inflammation. Patients may present with a swollen, red eye and decreased vision. Medical and surgical decompression in the accident and emergency department is possible.[7] Urgent ophthalmological consultation is required.
Use of this content is subject to our disclaimer