Investigations
1st investigations to order
haemoglobin and haematocrit
Test
A low haemoglobin or haematocrit will establish the presence of anaemia. It is reasonable to use the lower limit of normal for the individual laboratory.[78]
Result
the World Health Organization defines anaemia as: haemoglobin <130 g/L (13 g/dL) in men aged ≥15 years; <120 g/L (12 g/dL) in non-pregnant women aged ≥15 years; and <110 g/L (11 g/dL) in pregnant women
platelet count
Test
Iron deficiency is associated with thrombocytosis and, if severe, may cause thrombocytopenia.[98]
Result
normal, elevated, or decreased
MCV
Test
This is routinely reported as part of the FBC and is calculated as haematocrit (%) × 10/red blood cell count (× 10⁶/microL). MCV <80 fL is considered microcytic.
Iron deficiency is still considered a potential cause of anaemia unless the MCV is >95 fL; this cutoff has a sensitivity of 97.6%.[99]
A low MCV is encountered in a number of different diseases and so is not specific for IDA.[100]
Result
<80 fL
MCH
Test
This is a measurement of the haemoglobin mass per cell and is calculated from findings on the FBC as Hb (g/dL) × 10/red blood cell count (× 10⁶/microL). A value less than 27.5 picograms/red cell is considered low.
Medium sensitivity and specificity.[101]
Result
low (<27.5 picograms/red cell)
MCHC
Test
This is a measurement of the haemoglobin concentration per cell corrected for the haematocrit and is calculated from findings on the FBC as haemoglobin (g/dL) × 100/haematocrit (%).
Medium sensitivity and specificity.[101]
Result
low (<295 g/L [<29.5 g/dL])
red cell distribution width
Test
The red cell distribution width (RDW) is the coefficient of variation in red cell volume. Increased RDW can be an early finding in IDA even before a change appears in the MCV.
An increased RDW has a sensitivity of 90% to 100% for IDA, but a specificity of only 50% to 70% in distinguishing it from thalassaemia.[4]
Result
>14.6%
peripheral blood smear
Test
The peripheral smear of IDA contains small, pale red cells with anisopoikilocytosis (variation in size and shape) and pencil cells.
Changes on the peripheral smear may be seen before changes in MCV. Sensitivity and specificity varies by experience.[Figure caption and citation for the preceding image starts]: Peripheral blood smear demonstrating some changes often seen with iron deficiency anaemia. Note that many of the red cells are microcytic (compare size of red cell with the lymphocyte nucleus) and hypochromic (wide central pallor). There are some pencil formsFrom personal collection of Dr Rebecca Fischer Connor; used with permission [Citation ends].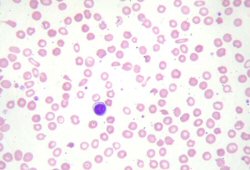
Result
microcytic, hypochromic pencil red cells
reticulocyte count
Test
Reticulocytes are the youngest population of red cells.
Reticulocyte count is low in IDA because the bone marrow does not have sufficient iron to produce red cells.
High sensitivity, low specificity.
Result
low
serum iron
Test
The serum iron level measures the amount of metal bound to transferrin for transport.
Values can vary greatly between laboratories, and values from the same individual performed at the same laboratory can vary as much 40% from day to day, partly because of diurnal variation.[4]
Result
decreased
total iron-binding capacity
Test
Total iron-binding capacity is an indirect measure of the amount of iron that transferrin will bind.
Values can vary greatly between laboratories and overlap between patients with and without iron deficiency.[4]
Result
increased
transferrin saturation
Test
Transferrin saturation = serum iron × 100/total iron-binding capacity (TIBC).
Values of transferrin saturation are more reliable between laboratories than are serum iron or TIBC alone, because sources of error cancel each other out.
Once the transferrin saturation falls below 16%, the decreased supply of iron limits red blood cell production.[4] Among non-pregnant women of childbearing age, serum transferrin saturation <16% has a sensitivity of 20% and a specificity of 93%.[8]
Result
<16%
serum ferritin
Test
This is an indirect yet quantitative and non-invasive measure of iron stores. Ferritin is an intracellular iron storage protein but small amounts are secreted into plasma.[4]
A serum ferritin <45 nanograms/mL has a sensitivity of 85% and a specificity of 92%, and a likelihood ratio of 11, for the diagnosis of IDA.[75][99]
A level between 45 and 100 nanograms/mL has a sensitivity of 9.4% and a specificity of 80% and a likelihood ratio of 0.5.
A level >100 nanograms/mL effectively rules out iron deficiency with a sensitivity of 5.5%, specificity of 29%, and likelihood ratio of 0.1.[99]
Result
low (<12 nanograms/mL is generally diagnostic of IDA, but thresholds vary between guidelines)
coeliac serology
urinalysis
Test
Urinalysis is done routinely in all patients to evaluate blood loss from the renal tract.
Renal tract malignancy is a recognised uncommon cause of IDA.[78]
Result
blood in the urine may indicate blood loss is from the renal tract
Helicobacter pylori testing
Test
Testing for H pylori infection should be carried out in all patients at initial presentation. A positive test (i.e., presence of IgG antibodies or faecal antigen associated with H pylori) should be confirmed with a urease breath test or endoscopy with biopsy.[79]
Result
if positive, H pylori is likely
Investigations to consider
haemoglobin electrophoresis
Test
Recommended in patients with hypochromic, microcytic anaemia if their ethnicity increases the risk of thalassaemia, to prevent unnecessary invasive gastrointestinal investigations.[78]
Result
may show thalassaemia; raised haemoglobin A2 level is a common beta-thalassaemia trait
urease breath test
Test
Rapid response diagnostic procedure used to identify Helicobactor pylori infection if initial H pylori testing (IgG antibodies or faecal antigen) is positive.
Result
if positive, suggestive of the presence of H pylori
autoimmune gastritis testing
Test
Performed if autoimmune gastritis is suspected. Patients with a positive test (i.e., presence of antiparietal cell or intrinsic factor antibodies, elevated gastrin) should be referred for endoscopic evaluation.[79]
Result
if positive, suggestive of an autoimmune aetiology of gastritis
upper gastrointestinal endoscopy (oesophagogastroduodenoscopy)
Test
Performed if the patient has any upper gastrointestinal (GI) symptoms. If the patient is asymptomatic, both upper and lower GI endoscopy are indicated.
All men (without history of obvious blood loss from an area other than the GI tract) and all women who are post-menopausal should be evaluated with upper and lower GI endoscopy.[78]
Result
may show a source of bleeding
small-bowel biopsy
Test
Small-bowel biopsy is advised during upper gastrointestinal endoscopy (if done), regardless of coeliac serology result.
Result
features of coeliac disease if present
lower gastrointestinal endoscopy (colonoscopy)
Test
Performed if the patient has any lower gastrointestinal (GI) symptoms. If the patient is asymptomatic, both upper and lower GI endoscopy are indicated.
All men (without history of obvious blood loss from an area other than the GI tract) and all women who are post-menopausal should be evaluated with upper and lower GI endoscopy.[78]
Result
may show a source of bleeding
CT colonography
Test
Can be done if colonoscopy is not available or suitable for the patient.[78]
Result
diverticulosis, ulcerative colitis, or neoplasm may be found
transferrin receptor-ferritin index
Test
This index has a very high sensitivity and specificity for IDA.[77]
Transferrin receptor-ferritin index can help diagnose IDA in patients with infection or chronic disease (e.g., cancer, autoimmune disorders).
Result
high ratio of transferrin receptor to log ferritin
bone marrow biopsy
Test
Haemosiderin in the bone marrow can be quantitated by assessing these golden-yellow refractile granules on an unstained bone marrow slide or by using Prussian blue staining. This staining is graded from 0 to 6+ by an experienced pathologist.[4]
Bone marrow biopsy is considered the most specific and sensitive test for IDA diagnosis but is not completely free of error.[4][12] It is usually reserved for patients with unclear serum studies in order to differentiate IDA from anaemia of chronic disease.
Result
absent iron stores
monitored trial of iron
Test
Daily oral iron supplements are given for 4 weeks, then FBC is repeated. Useful to distinguish between IDA and anaemia of chronic disease. May be helpful in children with suspected dietary iron deficiency.[102]
Result
rise in haemoglobin of 20 g/L (2 g/dL) (10 g/L [1 g/dL] in children) in 4 weeks with iron supplementation
faecal occult blood tests
Test
Faecal occult blood tests are generally not useful in evaluation of IDA.[78] If a patient has already been shown to have iron deficiency, a site for potential bleeding must be sought through endoscopy.
A faecal occult blood test may; however, be useful in frail patients to screen for gastrointestinal bleeding to avoid unnecessary invasive testing (e.g., endoscopy).[81]
Result
may be positive
Emerging tests
urinary hepcidin
percentage of hypochromic erythrocytes
Test
This could be calculated manually but would be very time-intensive. It can also be calculated in selected haematology analysers, which are not widely available. As with decreased MCV, this is a late finding in IDA.[100]
Result
increased percentage of hypochromic erythrocytes (>5%)
reticulocyte haemoglobin content
Test
Reticulocyte haemoglobin content shows the amount of available iron for erythropoiesis in the previous 3 to 4 days, and is an early indicator of iron status.[104]
Reticulocyte haemoglobin content decreases within the first few days of IDA.
This appears to have a high sensitivity and questionable specificity but is not widely available.[100] Patients with other causes of high MCV or thalassaemia may have false-normal values.
Result
low (<28 picograms)
erythrocyte protoporphyrin
Test
Erythrocyte protoporphyrin is the immediate precursor of haemoglobin and its levels increase when there is insufficient iron available for haemoglobin production.[8] Zinc protoporphyrin is a product of abnormal haem synthesis. An elevated level is found in patients with IDA and in patients with anaemia of chronic disease.[105]
Results can be falsely elevated with lead toxicity or high bilirubin.[100] In children and adolescents aged 6 months to 17 years, this has an estimated sensitivity of 42% and specificity of 61%.[8]
Result
>80 mmol/mol
Use of this content is subject to our disclaimer