Epidemiology
Histoplasma capsulatum is endemic in temperate regions of the world including the Ohio, Mississippi, and Missouri River valleys in the US, southern Mexico, the Caribbean, and Central and South America.[3][4] One study using surveillance data from 12 US states during 2011–2014 found that annual incidence rates were highest in Arkansas, Illinois, Indiana, Michigan, and Minnesota, with state-specific annual incidence rates ranging from 0 to 4.3 cases per 100,000 population, and average county-level incidence ranging from 0 to 39 cases per 100,000 population.[5] One retrospective analysis of data from 2007-2016 found that histoplasmosis was diagnosed in significant numbers outside the historical geographic distribution, with 94% of US states above the clinically relevant threshold for histoplasmosis in at least one county.[6] Surveillance data from 2019 found that the overall incidence in 12 US states where histoplasmosis is reportable was 1.8 cases per 100,000 population.[7] It was more common in males and in people aged 41 to 80 years.[7]
In Europe, histoplasmosis is much less common, and most cases are thought to occur as a result of travel to an endemic area or to exposure to microfoci of H capsulatum (e.g., bird roosts, caves, and areas inhabited by bats and birds).[8] In addition to H capsulatum, certain areas of Africa are endemic for H capsulatum var duboisii, the cause of African histoplasmosis, a clinically distinct form of histoplasmosis. Disease occurs sporadically in endemic areas and is extremely uncommon outside these regions.
H capsulatumgrows well in soil, and the presence of bird or bat droppings enhances its sporulation.[4] Air currents can carry spores (conidia) over very long distances. Outbreaks have occurred in association with activities that involve exposure to contaminated sites and dispersal of soil microconidia (e.g., cave exploration, being around bird roosts and old farm buildings, excavation, and gathering and cutting wood). Outbreaks may occur in both rural and urban areas. In some areas, up to 90% of the population show evidence of unrecognised prior infection (e.g., detection with a positive skin test).[9] Of HIV-infected patients in these areas, 10% to 25% develop disseminated histoplasmosis. Although most cases are either asymptomatic or self-limiting, 1 in 2000 acute infections results in disseminated histoplasmosis, usually in patients with impaired immunity.[10] In endemic areas, histoplasmosis is a frequent opportunistic pathogen of patients with AIDS.
[Figure caption and citation for the preceding image starts]: Histoplasma capsulatum in a soil sample Dr Libero Ajello, Public Health Image Library, US Centers for Disease Control and Prevention [Citation ends].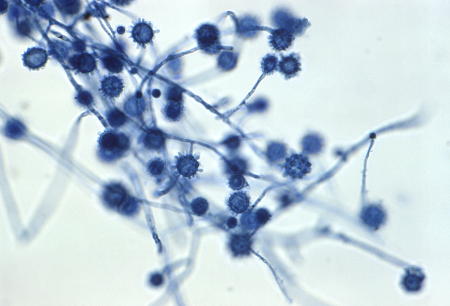
Use of this content is subject to our disclaimer