Investigations
1st investigations to order
serum alkaline phosphatase
serum gamma-GT
Test
Indication of bile duct injury and/or obstruction. Supports liver origin of elevated serum alkaline phosphatase (rather than bone origin).
Result
elevated
serum aminotransferases (aspartate aminotransferase, alanine aminotransferase)
Test
Indication of hepatocellular injury.
Most patients have mild to moderate elevation in serum aminotransferase levels (typically 2-3 times the upper limit of normal).
Predominant aminotransferase levels, or levels more than 5 times the upper limit of normal, may suggest overlapping autoimmune hepatitis, but precise criteria for PSC-autoimmune hepatitis overlap are not available.[3]
Result
mild to moderate elevation (typically <300 international units/L)
serum total bilirubin
serum albumin
Test
Normal in patients with early-stage disease, low in patients with advanced liver disease, and may be low in patients with active inflammatory bowel disease.
Result
normal or low
FBC
Test
Indication of liver synthetic dysfunction due to advanced liver disease and suggestive of portal hypertension.[28]
Result
normal or thrombocytopenia ± anaemia, leukopenia
prothrombin time
Test
Indication of liver synthetic dysfunction and could also reflect vitamin K deficiency due to malabsorption from cholestasis. Usually within normal range because the majority of patients have intact liver synthetic function at the time of diagnosis.
Result
normal or prolonged
abdominal ultrasound
Test
Non-invasive initial test to investigate for bile duct abnormality and may also provide evidence of more advanced liver disease.[2] Does not provide an adequate evaluation of the biliary tree to diagnose or exclude PSC.
Result
abnormal bile ducts (± cirrhotic liver, ascites, splenomegaly)
magnetic resonance cholangiopancreatography (MRCP)
Test
MRCP is the preferred diagnostic test for suspected PSC in adults and children.[2][3][34] MRCP can also be used to investigate the features of autoimmune hepatitis in children with PSC and to look for PSC in children with autoimmune hepatitis.[2] A 3D MRI/MRCP with T1- and T2-weighted axial images and contrast enhancement should be obtained.[3] MRCP is non-invasive, has comparable performance to ERCP with high sensitivity and specificity for diagnosis, and is not associated with risk of pancreatitis, bleeding, cholangitis, or perforation.[30][35][36]
There is both intrahepatic and extrahepatic duct involvement in 50% to 70% of cases. There is intrahepatic duct-only involvement in 15% to 25% of cases. There is extrahepatic duct-only involvement in <5% of cases.[5][8][11]
Normal in patients with small-duct PSC; MRI/MRCP should be repeated every 3-5 years to monitor for the development of large-duct PSC.[3][8][11][12]
Result
normal or multi-focal intrahepatic and/or extrahepatic strictures and dilations ± relevant stricture
serum IgG4
Test
Elevated levels of IgG4 have been associated with a multi-organ lymphoplasmocytic sclerosing disease that can include a sclerosing cholangitis. IgG4-associated cholangitis is often associated with autoimmune pancreatitis and responds readily to corticosteroid immunosuppression.
Up to 15% of patients with PSC have elevated IgG4 serum levels, but use of corticosteroids or immunosuppressive therapy is not suggested for those with mild elevated serum IgG4 levels (<2x upper limit of normal).[2][3] A diagnosis of IgG4-associated sclerosing cholangitis is suggested by an IgG4 >5.6 g/L, whereas it can be excluded by a serum IgG4 of 1.4 to 2.8 g/L in combination with a IgG4/IgG1 ratio of <0.24.[2][3] US guidance recommends testing all patients with possible PSC for IgG4, whereas European guidelines recommend determining serum IgG4 levels in all adults with large-duct PSC at the time of diagnosis.[2][3][30]
Result
normal or elevated
Investigations to consider
endoscopic retrograde cholangiopancreatography (ERCP)
Test
ERCP should generally be avoided for the diagnosis of PSC.[3] ERCP is indicated when MRCP is non-diagnostic or when therapeutic intervention is anticipated (e.g., brush cytology to evaluate for co-existing malignancy, extraction of bile duct stones, and dilation of prominent bile duct strictures).[30][35][36][Figure caption and citation for the preceding image starts]: Typical endoscopic retrograde cholangiopancreatography findings in a patient with PSC: multi-focal strictures of the intra- and extrahepatic bile ductsDr Kris Kowdley's collection [Citation ends].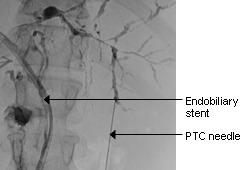 [Figure caption and citation for the preceding image starts]: Normal endoscopic retrograde cholangiopancreatographyDr Michael Saunders' collection [Citation ends].
[Figure caption and citation for the preceding image starts]: Normal endoscopic retrograde cholangiopancreatographyDr Michael Saunders' collection [Citation ends]. [Figure caption and citation for the preceding image starts]: Normal cholangiogram-pancreatogramDr Michael Saunders' collection [Citation ends].
[Figure caption and citation for the preceding image starts]: Normal cholangiogram-pancreatogramDr Michael Saunders' collection [Citation ends].
ERCP is invasive and with around 10% risk of procedure-related complications (pancreatitis, bacterial cholangitis, bleeding, liver abscess, perforation).[48]
During interventional procedures accessing the biliary tract, brush cytology should be performed to rule out cholangiocarcinoma, although yields are notably as low as 18%.[45] Diagnosis of cholangiocarcinoma remains difficult, and work-up should include tumour markers such as CA 19-9, imaging, and fluorescence in situ hybridisation.[30][46] Cytology and fluorescence in situ hybridisation of ERCP biliary brushings should be performed for all patients with suspected perihilar or distal cholangiocarcinoma.[3]
Result
normal or multi-focal intrahepatic and/or extrahepatic strictures and dilations ± dominant biliary stricture
serum immunoglobulins
Test
Can indicate the presence of PSC, although also commonly associated with other liver diseases.
Result
IgG normal or elevated; IgM elevated
24 hour urine copper concentration
Test
Indicated when clinical history and abnormal liver tests suggest Wilson's disease. Typically elevated in Wilson's disease, but elevated levels can occur in patients with any form of cholestatic liver disease.
Result
normal or elevated
ceruloplasmin
Test
Indicated when clinical history and abnormal liver tests suggest Wilson's disease. Ceruloplasmin is typically low in Wilson's disease.
Result
normal or elevated
anti-nuclear antibody
Test
Commonly present in autoimmune hepatitis; present in 8% to 77% of patients with PSC.[16]
Result
positive or negative
anti-smooth muscle antibody
Test
Commonly present in autoimmune hepatitis; present in 0% to 83% of patients with PSC.[16]
Result
positive or negative
antimitochondrial antibody
Test
Tested if primary biliary cholangitis is considered. Nearly always present in patients with primary biliary cholangitis, but notably absent in patients with PSC.
Result
negative
abdominal CT scan
Test
Result
may reveal bile duct thickening, focal or saccular intrahepatic duct dilation, and lymphadenopathy; intrahepatic mass lesion if present suggests cholangiocarcinoma
liver biopsy
Test
Histological findings are wide ranging and non-specific. May include: periductal fibrosis and inflammation, bile ducts surrounded by concentric fibrosis with an 'onion skin' appearance, bile ducts completely obliterated by fibrosis, proliferation of bile ducts in some portal tracts and loss of bile ducts ('ductopenia') in other portal tracts, varying degrees of fibrosis (periportal, bridging, cirrhosis).[44]
Not routinely needed for the diagnosis of PSC but should be considered (US guidance)/is recommended (European guidelines) for diagnosing small-duct PSC or overlapping autoimmune hepatitis.[2][3][34]
Result
fibro-obliterative cholangitis (<12% of cases)
bone mineral density scan
colonoscopy
Test
Patients newly diagnosed with PSC should undergo ileocolonoscopy with biopsies regardless of whether or not they already have a diagnosis of inflammatory bowel disease (IBD).
Ileocolonoscopy should be repeated (US guidance) or can be considered (European guidelines) every 5 years if IBD is not present or whenever the patient has symptoms suggestive of IBD.[2][3]
From the age of 15 years, patients with co-existing IBD should undergo high-definition surveillance colonoscopy regularly due to a high risk of colorectal cancer. US guidance suggests 1- to 2-year surveillance intervals, whereas European guidelines recommend surveillance annually, with 1- to 2-year intervals if there is no inflammatory activity.[2][3][30][34][40] Children with PSC can undergo initial non-invasive screening for IBD via measurement of faecal calprotectin levels, with endoscopic assessment reserved for those with raised faecal calprotectin levels or symptoms.[2]
Result
normal
transient elastography
Use of this content is subject to our disclaimer