Allergic bronchopulmonary aspergillosis (ABPA) is a hypersensitivity reaction to bronchial colonisation byAspergillus fumigatus mould, typically affecting patients with an underlying predisposition, specifically asthma or cystic fibrosis.
When predisposed individuals inhale the aspergillus spores, which are ubiquitous in the environment, the spores germinate in the lungs, setting off a complex immune cascade which results in the formation of immunoglobulin E and immunoglobulin G antibodies and immune-mediated lung destruction.
ABPA usually presents in a similar way to asthma but may be complicated by bronchial obstruction, fever, malaise, expectoration of brownish mucus plugs, peripheral blood eosinophilia, and haemoptysis in later stages.
Treatment involves corticosteroids with or without antifungal therapy. Monoclonal antibodies used for the treatment of asthma are under active investigation as a promising alternative treatment for ABPA.
Early diagnosis and rapid initiation of treatment can prevent the development of bronchiectasis or pulmonary fibrosis that otherwise occurs in the later stages of the disease.
ABPA is caused by a hypersensitivity reaction to the mould Aspergillus fumigatus colonising the airways of patients with pre-existing chronic airways disease, most commonly asthma or cystic fibrosis.[1]Agarwal R, Chakrabarti A, Shah A, et al. Allergic bronchopulmonary aspergillosis: review of literature and proposal of new diagnostic and classification criteria. Clin Exp Allergy. 2013 Aug;43(8):850-73.
https://onlinelibrary.wiley.com/doi/10.1111/cea.12141
http://www.ncbi.nlm.nih.gov/pubmed/23889240?tool=bestpractice.com
[2]Mahdavinia M, Grammer LC. Management of allergic bronchopulmonary aspergillosis: a review and update. Ther Adv Respir Dis. 2012;6:173-187.
http://www.ncbi.nlm.nih.gov/pubmed/22547692?tool=bestpractice.com
[3]Agarwal R, Muthu V, Sehgal IS, et al. Prevalence of aspergillus sensitization and allergic bronchopulmonary aspergillosis in adults with bronchial asthma: a systematic review of global data. J Allergy Clin Immunol Pract. 2023 Jun;11(6):1734-51.e3.
http://www.ncbi.nlm.nih.gov/pubmed/37088374?tool=bestpractice.com
Patients usually have a prior diagnosis of atopy, asthma, or cystic fibrosis.[4]Zander DS. Allergic bronchopulmonary aspergillosis: an overview. Arch Pathol Lab Med. 2005;129:924-928.
http://www.archivesofpathology.org/doi/full/10.1043/1543-2165%282005%29129%5B924%3AABAAO%5D2.0.CO%3B2
http://www.ncbi.nlm.nih.gov/pubmed/15974818?tool=bestpractice.com
Exposure of an atopic person to fungal elements results in the formation of IgE and IgG antibodies.[5]Tillie-Leblond I, Tonnel AB. Allergic bronchopulmonary aspergillosis. Allergy. 2005;60:1004-1013.
http://onlinelibrary.wiley.com/doi/10.1111/j.1398-9995.2005.00887.x/full
http://www.ncbi.nlm.nih.gov/pubmed/15969680?tool=bestpractice.com
Typically, the patient presents with bronchial obstruction, airway inflammation, and mucoid impaction that can lead to bronchiectasis, fibrosis, and respiratory compromise.
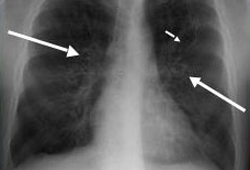
ABPA typically presents with a constellation of clinical, laboratory, and radiographic findings, including symptoms of bronchospasm, wheezing, and productive cough; laboratory markers of allergic inflammation such as eosinophilia and elevated IgE levels; evidence of Aspergillus allergy and sensitisation (e.g., formation of Aspergillus-specific IgE and IgG antibodies); as well as characteristic radiographic infiltrates. Untreated/uncontrolled disease can lead to long-term sequelae such as bronchiectasis, fibrosis, and respiratory compromise.