Approach
Loss of the meniscus diminishes the area of force distribution, increases force concentration, and eventually leads to arthritis; therefore, early diagnosis and efforts at saving meniscus volume are important.[32][33]
Non-operative care
Initially all patients should be treated with rest, ice, compression of the knee with an elastic bandage, and elevation of the leg above the level of the heart (RICE). This protocol helps to reduce pain, minimise swelling, and protect the injured tissue, all of which help speed up the healing process. In addition, physiotherapy programmes designed to improve knee joint range of motion, core and leg strength, and knee stability, and to normalise gait are recommended. The use of crutches or a knee brace may be helpful with painful displaced bucket-handle tears.
Non-steroidal anti-inflammatory drugs (NSAIDs) should be used only for short periods because of the negative effects on musculoskeletal healing.[34] Paracetamol is the preferred drug for reducing pain because it acts centrally and does not interfere with the healing process.[35]
Small meniscal tears (<1 cm) located in the far posterior horns and that are asymptomatic do not require operative intervention, and may simply be observed and treated conservatively with RICE and analgesia. Physiotherapy is not necessary for small meniscal tears to heal but is beneficial for addressing gait abnormalities and strengthening the leg muscles that surround and stabilise the knee joint.
For patients with degenerative meniscus tear, knee arthroscopy does not appear to confer any important benefit over conservative strategies (including sham surgery or exercise therapy).[36] A BMJ clinical practice guideline makes a strong recommendation against the use of arthroscopy in nearly all patients with degenerative knee disease, including those with meniscal tear.[37]
BMJ Rapid Recommendations: arthroscopic surgery for degenerative knee arthritis and meniscal tears: a clinical practice guideline
Opens in new window[Figure caption and citation for the preceding image starts]: BMJ Rapid Recommendations: arthroscopic surgery for degenerative knee arthritis and meniscal tears: a clinical practice guidelineBMJ 2017 May 10;357:j1982 [Citation ends]. MAGICapp: recommendations, evidence summaries and consultation decision aids
Opens in new window
MAGICapp: recommendations, evidence summaries and consultation decision aids
Opens in new window
In one randomised controlled trial, there was no statistically significant difference in the Knee Injury and Osteoarthritis Outcome Score (KOOS) between a strategy of exercise and education compared with early meniscal surgery in young and active adults with meniscal tear. This suggests that surgery may not be superior to exercise therapy in all patients, and that patient preferences should be taken into account during clinical decision-making.[38]
Operative care
If the meniscus tear is large (≥1 cm) or is a root tear (tear in the anterior or posterior meniscal roots where the meniscus attaches to the central tibial plateau), or if symptoms persist with non-operative care, arthroscopic surgery should be considered to prevent further damage. The degree of vascular penetration into the periphery of the meniscus ranges from 10% to 25% of the meniscal width. Consequently, most areas of the meniscus cannot heal by themselves because they are not vascularised.[15]
Surgical care should be directed at saving healthy meniscus tissue.[1] Suturing of the tissue is possible if a stable repair can be achieved (usually reserved for clear, clean pattern tears). Meniscal repair should only be used to heal peripheral meniscal lesions affecting healthy meniscal tissue (injury) in vascularised areas (red-red zone or red-white zone).[39] More than 80% of meniscal tears in the central third (red-white zone) can heal by surgery.[40] See Popliteal cyst for more information.
Partial meniscectomy for complex pattern tear should be limited as far as possible, and necessitates careful patient selection; there may be no difference in outcomes between those undergoing partial meniscectomy for traumatic tear or those for degenerative tear (for whom arthroscopy is no longer recommended).[1][41][42][43]
A complete meniscectomy, involving removal of the entire meniscus, is rarely performed and usually reserved for cases where the tear is large or cuts through the entire meniscus. Rarely, osteonecrosis of the knee can occur following meniscectomy.[44]
Associated ligamentous injury of the knee leads to knee instability. Therefore, in meniscal tears associated with such injuries, concomitant repair of the affected ligament should be considered, as meniscal repairs should be carried out on a stable knee.[39][Figure caption and citation for the preceding image starts]: Arthroscopic view of horizontal cleavage tear of lateral meniscus (arrow)From the collection of Dr Kevin R. Stone [Citation ends]. [Figure caption and citation for the preceding image starts]: Arthroscopic view of suture repair of lateral meniscus (arrow)From the collection of Dr Kevin R. Stone [Citation ends].
[Figure caption and citation for the preceding image starts]: Arthroscopic view of suture repair of lateral meniscus (arrow)From the collection of Dr Kevin R. Stone [Citation ends].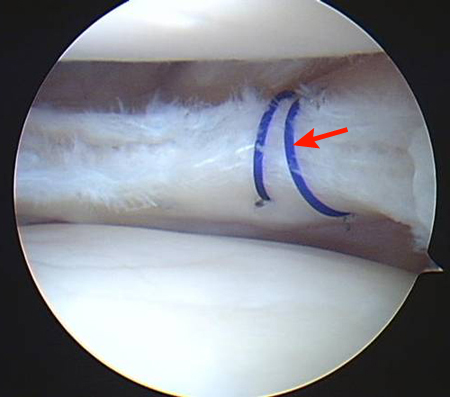
Post-operative care
Post-operative care of the repaired or resected meniscus focuses on limiting axial load and rotational movement for the first month, followed by range-of-motion and strengthening exercises.
Immediate post-operative care of the partial meniscectomy patient involves icing and elevation of the knee above the level of the heart, regularly throughout the day and night. Intra-articular hyaluronic acid injection may decrease post-operative knee pain and swelling following meniscectomy.[45] Patients use crutches for the first post-operative week and progress to weight bearing as tolerated.
Post-operative measures after a meniscus repair are similar to those after partial meniscectomy. However, weight bearing is approached more cautiously, and full weight bearing should be delayed for at least 4-6 weeks after surgery to reduce strain on the repair site. In addition, limiting the range of knee motion, especially full flexion, can protect the repair site.
A knee brace is not usually indicated following meniscectomy. After meniscal repair the need for a brace depends on patient activity and condition of repair.
Use of this content is subject to our disclaimer