Removal of polyps significantly reduces the risk of death from colorectal cancer.[55]Winawer SJ, Zauber AG, Ho MN, et al. Prevention of colorectal cancer by colonoscopic polypectomy. N Engl J Med. 1993 Dec 30;329(27):1977-81.
https://www.nejm.org/doi/10.1056/NEJM199312303292701
http://www.ncbi.nlm.nih.gov/pubmed/8247072?tool=bestpractice.com
[56]Zauber AG, Winawer SJ, O'Brien MJ, et al. Colonoscopic polypectomy and long-term prevention of colorectal-cancer deaths. N Engl J Med. 2012 Feb 23;366(8):687-96.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3322371
http://www.ncbi.nlm.nih.gov/pubmed/22356322?tool=bestpractice.com
[57]Stryker SJ, Wolff BG, Culp CE, et al. Natural history of untreated colonic polyps. Gastroenterology. 1987 Nov;93(5):1009-13.
http://www.ncbi.nlm.nih.gov/pubmed/3653628?tool=bestpractice.com
Polyps are removed for histological examination to exclude malignancy and/or to manage polyp-associated symptoms or complications. Endoscopic resection of non-malignant polyps is preferred to surgical resection, where possible, because it is associated with lower morbidity and mortality.[58]Ma C, Teriaky A, Sheh S, et al. Morbidity and mortality after surgery for nonmalignant colorectal polyps: a 10-year nationwide analysis. Am J Gastroenterol. 2019 Nov;114(11):1802-10.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6830963
http://www.ncbi.nlm.nih.gov/pubmed/31634261?tool=bestpractice.com
Large broad-based polyps, or those situated in anatomically inaccessible areas, are usually unsuitable for endoscopic resection and require open or laparoscopic bowel resection.[59]National Institute for Health and Care Excellence. Combined endoscopic and laparoscopic removal of colonic polyps. September 2014 [internet publication].
https://www.nice.org.uk/guidance/ipg503
Polypectomy techniques
Endoscopic polypectomy is usually performed by simple snare excision or by 'hot biopsy' (in which monopolar diathermy is used to excise the polyp and simultaneously coagulate its base).
Endoscopic mucosal resection (EMR) and endoscopic submucosal dissection (ESD) utilise saline injections to lift the area of mucosa to be resected, followed by resection of the mucosa and upper submucosa using either suction and a snare or a submucosal resection device. [Figure caption and citation for the preceding image starts]: Colonic adenoma pre-excisionFrom the personal collection of Dr G. Malietzis; used with permission [Citation ends].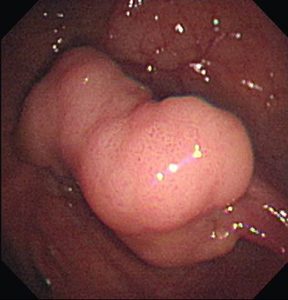 [Figure caption and citation for the preceding image starts]: Post-polypectomyFrom the personal collection of Dr G. Malietzis; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Post-polypectomyFrom the personal collection of Dr G. Malietzis; used with permission [Citation ends]. These are particularly useful if the polyp is sessile (flat) rather than pedunculated (with a stalk). The effectiveness of EMR and ESD for treating large colorectal polyps has been confirmed by systematic reviews.[60]Puli SR, Kakugawa Y, Gotoda T, et al. Meta-analysis and systematic review of colorectal endoscopic mucosal resection. World J Gastroenterol. 2009 Sep 14;15(34):4273-7.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2744182
http://www.ncbi.nlm.nih.gov/pubmed/19750569?tool=bestpractice.com
[61]Puli SR, Kakugawa Y, Saito Y, et al. Successful complete cure en-bloc resection of large nonpedunculated colonic polyps by endoscopic submucosal dissection: a meta-analysis and systematic review. Ann Surg Oncol. 2009 Aug;16(8):2147-51.
http://www.ncbi.nlm.nih.gov/pubmed/19479308?tool=bestpractice.com
These are particularly useful if the polyp is sessile (flat) rather than pedunculated (with a stalk). The effectiveness of EMR and ESD for treating large colorectal polyps has been confirmed by systematic reviews.[60]Puli SR, Kakugawa Y, Gotoda T, et al. Meta-analysis and systematic review of colorectal endoscopic mucosal resection. World J Gastroenterol. 2009 Sep 14;15(34):4273-7.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2744182
http://www.ncbi.nlm.nih.gov/pubmed/19750569?tool=bestpractice.com
[61]Puli SR, Kakugawa Y, Saito Y, et al. Successful complete cure en-bloc resection of large nonpedunculated colonic polyps by endoscopic submucosal dissection: a meta-analysis and systematic review. Ann Surg Oncol. 2009 Aug;16(8):2147-51.
http://www.ncbi.nlm.nih.gov/pubmed/19479308?tool=bestpractice.com
Polyps that do not rise easily with submucosal saline or hyaluronidase infiltration are highly suspicious for invasive malignancy. Successful endoscopic mucosal resection is unlikely if three or more quadrants do not rise easily with fluid infiltration; surgical management is more suitable in these cases.
Surgical polypectomy may be required if a polyp is very low in the rectum and its distal margin cannot be safely endoscopically resected. Small polyps (up to 8 mm) may be removed using a cold snare technique where electrocautery is not required. This technique has confirmed efficacy.[62]Paspatis GA, Tribonias G, Konstantinidis K, et al. A prospective randomized comparison of cold vs hot snare polypectomy in the occurrence of postpolypectomy bleeding in small colonic polyps. Colorectal Dis. 2011 Oct;13(10):e345-8.
http://www.ncbi.nlm.nih.gov/pubmed/21689363?tool=bestpractice.com
Management of polyps with invasive cancer
Polyps are considered malignant if cancer invades through the muscularis mucosa into the submucosa. Carcinoma in situ is not considered malignant because it is unable to metastasise to regional lymph nodes.[63]National Comprehensive Cancer Network. NCCN clinical practice guidelines in oncology: colon cancer [internet publication].
https://www.nccn.org/guidelines/category_1
Management of polyps containing invasive cancer depends on the type of polyp and the presence or absence of favourable histological features.[63]National Comprehensive Cancer Network. NCCN clinical practice guidelines in oncology: colon cancer [internet publication].
https://www.nccn.org/guidelines/category_1
Favourable histological features are:[63]National Comprehensive Cancer Network. NCCN clinical practice guidelines in oncology: colon cancer [internet publication].
https://www.nccn.org/guidelines/category_1
[64]Bujanda L, Cosme A, Gil I, et al. Malignant colorectal polyps. World J Gastroenterol. 2010 Jul 7;16(25):3103-11.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2896747
http://www.ncbi.nlm.nih.gov/pubmed/20593495?tool=bestpractice.com
Well-differentiated or moderately differentiated (grade 1 or 2) adenocarcinoma
No angiolymphatic invasion
Negative margin of resection.
Surgery is not required for patients with completely resected pedunculated polyps with favourable histological features.[63]National Comprehensive Cancer Network. NCCN clinical practice guidelines in oncology: colon cancer [internet publication].
https://www.nccn.org/guidelines/category_1
Patients with completely resected sessile polyps with favourable histological features may be considered for observation or for colectomy with en bloc removal of regional lymph nodes.[63]National Comprehensive Cancer Network. NCCN clinical practice guidelines in oncology: colon cancer [internet publication].
https://www.nccn.org/guidelines/category_1
Patients with sessile polyps may have increased risk of disease recurrence, mortality, and metastases compared with patients with pedunculated polyps.[65]Cooper HS. Surgical pathology of endoscopically removed malignant polyps of the colon and rectum. Am J Surg Pathol. 1983 Oct;7(7):613-23.
http://www.ncbi.nlm.nih.gov/pubmed/6638257?tool=bestpractice.com
See Colorectal cancer for further details on surgery for invasive colorectal cancer.
If a specimen is fragmented, resection margins cannot be assessed, or there are unfavourable histological features, the patient should undergo further investigations to assess the extent of disease prior to colectomy with en bloc removal of regional lymph nodes.[63]National Comprehensive Cancer Network. NCCN clinical practice guidelines in oncology: colon cancer [internet publication].
https://www.nccn.org/guidelines/category_1
See Colorectal cancer for further detail on the investigation and management of such patients.
Surveillance after polypectomy
Surveillance after polypectomy is individualised to the patient's risk of colorectal cancer. Colorectal cancer risk is determined by the presence, number, and size of polyps found at index colonoscopy, as well as by factors such as age and family history.
The US Multi-Society Task Force on Colorectal Cancer recommends that patients with 1 to 2 small (<1 cm) low-grade tubular adenomas should undergo repeat colonoscopy in 5 to 10 years.[66]Lieberman DA, Rex DK, Winawer SJ, et al. Guidelines for colonoscopy surveillance after screening and polypectomy: a consensus update by the US Multi-Society Task Force on Colorectal Cancer. Gastroenterology. 2012 Sep;143(3):844-57.
https://www.gastrojournal.org/article/S0016-5085(12)00812-8/fulltext
http://www.ncbi.nlm.nih.gov/pubmed/22763141?tool=bestpractice.com
Finding 3 to 10 adenomas, or any adenoma ≥1 cm, displaying high-grade dysplasia, or with villous features, should prompt repeat colonoscopy at 3 years; >10 adenomas at a single examination should prompt follow-up in <3 years and a familial syndrome should be considered.[66]Lieberman DA, Rex DK, Winawer SJ, et al. Guidelines for colonoscopy surveillance after screening and polypectomy: a consensus update by the US Multi-Society Task Force on Colorectal Cancer. Gastroenterology. 2012 Sep;143(3):844-57.
https://www.gastrojournal.org/article/S0016-5085(12)00812-8/fulltext
http://www.ncbi.nlm.nih.gov/pubmed/22763141?tool=bestpractice.com
Sessile adenomas removed piecemeal should be reviewed within 1 year to ensure complete removal.[66]Lieberman DA, Rex DK, Winawer SJ, et al. Guidelines for colonoscopy surveillance after screening and polypectomy: a consensus update by the US Multi-Society Task Force on Colorectal Cancer. Gastroenterology. 2012 Sep;143(3):844-57.
https://www.gastrojournal.org/article/S0016-5085(12)00812-8/fulltext
http://www.ncbi.nlm.nih.gov/pubmed/22763141?tool=bestpractice.com
The US National Comprehensive Cancer Network guidelines recommend colonoscopy 6 months after piecemeal resection; the European Society for Gastroenterology recommends colonoscopy at 3-6 months for any piecemeal endoscopic resection of polyps ≥2 cm.[47]National Comprehensive Cancer Network. NCCN clinical practice guidelines in oncology: colorectal cancer screening [internet publication].
https://www.nccn.org/guidelines/category_2
[67]Hassan C, Antonelli G, Dumonceau JM, et al. Post-polypectomy colonoscopy surveillance: European Society of Gastrointestinal Endoscopy (ESGE) guideline - update 2020. Endoscopy. 2020 Aug;52(8):687-700.
http://www.ncbi.nlm.nih.gov/pubmed/32572858?tool=bestpractice.com
People with high-risk adenomas have a three- to fourfold higher risk of incident colorectal cancer during follow-up, compared with people with no adenomas or low-risk adenomas.[49]Lieberman D, Ladabaum U, Brill JV, et al. Reducing the burden of colorectal cancer: AGA position statements. Gastroenterology. 2022 Aug;163(2):520-6.
https://www.doi.org/10.1053/j.gastro.2022.05.011
http://www.ncbi.nlm.nih.gov/pubmed/35715380?tool=bestpractice.com
UK guidelines state that if two or more pre-malignant polyps (including at least one advanced colorectal polyp) or five or more pre-malignant polyps are found, the patient should undergo a one-off surveillance colonoscopy at 3 years.[45]Rutter MD, East J, Rees CJ, et al. British Society of Gastroenterology/Association of Coloproctology of Great Britain and Ireland/Public Health England post-polypectomy and post-colorectal cancer resection surveillance guidelines. Gut. 2020 Feb;69(2):201-23.
https://gut.bmj.com/content/69/2/201.long
http://www.ncbi.nlm.nih.gov/pubmed/31776230?tool=bestpractice.com
If a patient has had invasive adenocarcinoma in a polyp that was completely excised, colonoscopy is recommended 1 year after index colonoscopy.[63]National Comprehensive Cancer Network. NCCN clinical practice guidelines in oncology: colon cancer [internet publication].
https://www.nccn.org/guidelines/category_1
If an advanced adenoma (villous polyp, polyp >10 mm, or high-grade dysplasia) is present, colonoscopy should be repeated after 1 year. If there is no advanced adenoma, colonoscopy is recommended at 3 years, and then every 5 years.[63]National Comprehensive Cancer Network. NCCN clinical practice guidelines in oncology: colon cancer [internet publication].
https://www.nccn.org/guidelines/category_1
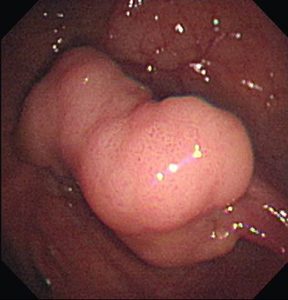 [Figure caption and citation for the preceding image starts]: Post-polypectomyFrom the personal collection of Dr G. Malietzis; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Post-polypectomyFrom the personal collection of Dr G. Malietzis; used with permission [Citation ends]. These are particularly useful if the polyp is sessile (flat) rather than pedunculated (with a stalk). The effectiveness of EMR and ESD for treating large colorectal polyps has been confirmed by systematic reviews.[60][61]
These are particularly useful if the polyp is sessile (flat) rather than pedunculated (with a stalk). The effectiveness of EMR and ESD for treating large colorectal polyps has been confirmed by systematic reviews.[60][61]