Aetiology
The primary differential diagnoses to consider for a maculopapular rash are:
Anaphylaxis
Drug-induced eruptions
Viral exanthems
Bacterial infections
Rickettsial diseases
Rheumatological diseases
Systemic diseases.
Initial clues to the correct category are derived from the history and clinical setting.
Anaphylaxis
Anaphylaxis is an acute-onset reaction (within minutes to several hours of exposure) involving the skin, mucosa, or both and respiratory (dyspnoea, wheezing, hypoxia) or cardiovascular (hypotension, syncope, shock) compromise.[1][2] The mucocutaneous signs and symptoms may include generalised urticaria, swollen lips or tongue, or pruritus. The gastrointestinal system may be affected as well, with symptoms including crampy abdominal pain, nausea, and diarrhoea. This reaction is most often related to:
Drug or food allergy
Insect bite or sting.
Other symptoms may include dizziness, agitation, confusion, and a sense of impending doom. Patients may appear flushed or pale and may have tachypnoea and/or tachycardia.
Drug-induced eruptions
Drug-induced eruption is the most common cause of maculopapular rash in adults. Maculopapular rash is the most common presentation of a drug eruption.
Cutaneous eruptions are observed in 1% to 3% of patients taking any particular medication and in up to 6.7% of hospital inpatients.[3][4][5] Severe drug reactions are estimated to occur in 0.1% of all hospitalised patients.[6]
Onset is usually 6 to 10 days after the first drug exposure, or within 3 days of a second exposure.[7] However, these eruptions can occur after the first dose or may not develop until 3 weeks after drug initiation. Chronological factors may guide diagnosis with respect to potential drug-drug interactions, response to removal of the suspected agent, and response to rechallenge.
In one long-term hospital study of nearly 50,000 patients, drug eruptions presented as maculopapular rash in 91% of cases.[8]
A drug may trigger very different kinds of reactions across individuals, or even in the same individual.[9]
Anticonvulsants, antibiotics (especially penicillins, cephalosporins, macrolides, trimethoprim), antifungals, antiretrovirals, non-steroidal anti-inflammatory drugs, and allopurinol are commonly implicated.[3]
Chemotherapeutic agents, particularly cytarabine, dacarbazine, hydroxyurea, paclitaxel, and procarbazine, have also been associated with maculopapular eruption.[10] The immunotherapeutic drugs pembrolizumab, nivolumab, and ipilimumab are associated with maculopapular eruptions.[11] Epidermal growth factor receptor inhibitors (e.g., cetuximab, panitumumab) may also cause cutaneous eruptions.[12][13]
Non-immediate reactions to iodinated contrast media also frequently include maculopapular eruption.[14]
In addition to the type of drug, risk factors for drug eruption include female sex, older age, polypharmacy, history of drug hypersensitivity reactions, hepatic failure, renal failure, and immunosuppression.[15][16]
[Figure caption and citation for the preceding image starts]: Hypersensitivity rash due to penicillinCDC Public Health Image Library [Citation ends]. [Figure caption and citation for the preceding image starts]: Drug eruption due to phenytoinPhotograph courtesy of Brian L. Swick [Citation ends].
[Figure caption and citation for the preceding image starts]: Drug eruption due to phenytoinPhotograph courtesy of Brian L. Swick [Citation ends].
The aetiology of most drug eruptions generally relates to delayed immunological hypersensitivity to the drug or a metabolite, with both humoral and cell-mediated mechanisms contributing. Most maculopapular eruptions are believed to be delayed-type (type IV) cell-mediated (often T-cell) reactions.[17] The reactions are often unpredictable, dose-independent, and idiosyncratic.[18]
Severe cutaneous drug eruptions
Stevens-Johnson syndrome and toxic epidermal necrolysis (SJS/TEN) are severe mucocutaneous reactions most often triggered by medications. SJS/TEN are considered part of a disease spectrum and are distinguished by percentage of body surface affected, with SJS involving <10% and TEN involving >30%.[19][20] SJS/TEN is a life-threatening condition with mortality rates of up to 30%.[20] Common offending medications include: anticonvulsants, sulfonamides, non-steroidal anti-inflammatory drugs, and allopurinol. Particular human leukocyte antigen (HLA) alleles confer higher risk of developing SJS/TEN after receiving a drug.
Patients with SJS/TEN have prodromal symptoms of malaise, fever, photophobia, and anorexia, followed by mucocutaneous inflammation and pain. Typically dusky red or purple ill-defined macules appear on the trunk, face, and proximal limbs. The conjunctival, buccal, and/or genital mucosa become painful, erythematous, and oedematous and develop bullous lesions followed by progressive sloughing of the skin and positive Nikolsky's sign (epidermal layer sloughs off easily when lateral pressure is applied).[19] These eruptions typically start 4 to 28 days after drug exposure.[21]
[Figure caption and citation for the preceding image starts]: Stevens-Johnson syndrome: epidermal loss on soles of feetFrom the personal collection of Dr A. Kowal-Vern [Citation ends].

[Figure caption and citation for the preceding image starts]: Toxic epidermal necrolysis with epidermal loss, ocular involvement, and ecthyma gangrenosumFrom the personal collection of Dr A. Kowal-Vern [Citation ends].

[Figure caption and citation for the preceding image starts]: Stevens-Johnson syndrome: targetoid lesions and epidermal lossFrom the personal collection of Dr A. Kowal-Vern [Citation ends].

Drug reaction with eosinophilia and systemic symptoms (DRESS) presents initially as a maculopapular drug eruption with fever, malaise, and lymphadenopathy 2 to 6 weeks after the initiation of the offending medication.[22][23] The latency between drug exposure and onset of symptoms is considerably longer in DRESS than in most drug eruptions and the patient is more ill, often with fever, abdominal pain, and facial swelling.[21][23] Organs are infiltrated with eosinophils or lymphocytes. About 80% of patients have hepatic involvement with alteration in liver function tests. Respiratory, cardiac, and renal inflammation can also occur. Mortality ranges from 5% to 10%, usually as a result of cardiac or pulmonary involvement or haemophagocytosis.[21][23] In excess of 40 causative drugs have been identified in literature reviews, with antibiotic and anticonvulsant drug classes most commonly implicated.[24]
Viral exanthems
A viral exanthem is a skin eruption occurring as a symptom of a general disease. Many of these eruptions are entirely non-specific. Possible causative agents include Epstein Barr virus, enterovirus, adenovirus, human herpesvirus-6 or 7, parvovirus B19, cytomegalovirus, acute HIV, acute viral hepatitis, Ebola virus, Zika virus, dengue virus, mpox, and chikungunya virus.[25][26][Figure caption and citation for the preceding image starts]: Viral exanthem presenting as a maculopapular eruption. Note urticarial appearance of non-scaling erythematous macules and papules on the trunk of this older childPhotograph courtesy of Hobart W. Walling [Citation ends]. [Figure caption and citation for the preceding image starts]: Viral exanthem presenting as a maculopapular eruption. Note the erythematous papules are larger than macules on the leg of a young adultPhotograph courtesy of Hobart W. Walling [Citation ends].
[Figure caption and citation for the preceding image starts]: Viral exanthem presenting as a maculopapular eruption. Note the erythematous papules are larger than macules on the leg of a young adultPhotograph courtesy of Hobart W. Walling [Citation ends].
Aetiological viruses tend to be seasonal, with enteroviruses and echoviruses predominating in the summer and autumn, and respiratory viruses predominating in the winter.
Enterovirus genus: coxsackievirus type A and B, echoviruses, and enteroviruses
These viruses can cause maculopapular rash and are typically transmitted by the faecal-oral or respiratory routes.
Infections are more common in the summer.
The usual incubation period is 3 to 6 days.
Rash is typically generalised and maculopapular, with petechiae, oral erosions, and conjunctival haemorrhage present.
Fever and pharyngitis are common.
Hand-foot-and-mouth disease is an example of an enterovirus (usually coxsackievirus types A16 and A7) illness, though the presentation is a vesicular eruption on the palms and soles with a vesicular stomatitis.[27]
Cytomegalovirus is a ubiquitous beta-herpes virus with seropositivity of approximately 60% in developed countries and 90% in developing countries.[28] The primary infection is often asymptomatic, although there may be fever and a non-specific maculopapular eruption. Cytomegalovirus can also cause infectious mononucleosis.
Epstein Barr virus (EBV, also known as human herpesvirus-4) is ubiquitous and causes infectious mononucleosis. Seropositivity for EBV may exceed 90% by early adulthood in developed countries.[29]
EBV preferentially affects the oropharyngeal mucosa and is transmitted primarily through infected saliva. Exposed children typically have a mild non-specific febrile illness that may go unnoticed. However, primary infection in adolescents and young adults results in infectious mononucleosis in about 50% of cases.
Most people with infectious mononucleosis are 14 to 25 years of age.
Incubation period of 4 to 8 weeks; triad of fever, lymphadenopathy, and exudative pharyngitis is common.
Rash begins on day 4 to 6 of illness, initially on the trunk and upper extremities, then extends to the forearms and face, with petechiae commonly present.
Ampicillin or penicillin induces a generalised eruption in most patients with infectious mononucleosis.[30] This rash usually occurs 1 week after taking the medication and is related to EBV antibodies cross-reacting with the drug. The rash lasts about 1 week before resolving with desquamation. When a maculopapular eruption occurs in a patient with EBV taking amoxicillin, the patient is not considered allergic to that medication.
Rubella (German measles) is responsible for a mild self-limited illness in children and adults, but in utero infections are associated with significant complications. Incidence has decreased remarkably since the introduction of the measles/mumps/rubella vaccine.
A prodrome including fever, headache, and upper respiratory symptoms develops after a 16- to 18-day incubation period.
One to 5 days later, a characteristic eruption of rose-pink macules begins on the face and extends cephalocaudally, lasting 2 to 3 days before fading in the same order.[Figure caption and citation for the preceding image starts]: Rubella presenting as a generalised abdominal rashCourtesy of the CDC Public Health Image Library [Citation ends].

The typical progression is more helpful in suspecting the diagnosis than is the rather non-specific-appearing eruption.
Petechial macules on the soft palate (Forscheimer spots) are characteristic of rubella.
Tender cervical lymphadenopathy is common.
Arthralgia and arthritis may occur, most commonly in adolescents and adults.
Hepatitis, peri/myocarditis, and anaemia are rare.
Rubeola (measles) has decreased in incidence with routine immunisation, though outbreaks continue to occur. A resurgence of the disease in 2019 has seen cases increase globally; atypical measles eruptions may arise in patients who fail immunisation or who have altered immunity.[31] In one measles outbreak in an undervaccinated community in the US (n=383 outbreak-related cases), fever was present in 99%, generalised rash in 100%, cough in 94%, conjunctivitis in 81%, and coryza in 77%.[32] Koplik's spots (grey-white papules on the buccal mucosa) appear during the prodrome and have long been considered pathognomonic of measles. However, in one cohort study Koplik spots were associated with other viral infections: for example, rubella, parvovirus, human herpesvirus 6.[33]
[Figure caption and citation for the preceding image starts]: Koplik's spotsCenters for Disease Control and Prevention [Citation ends].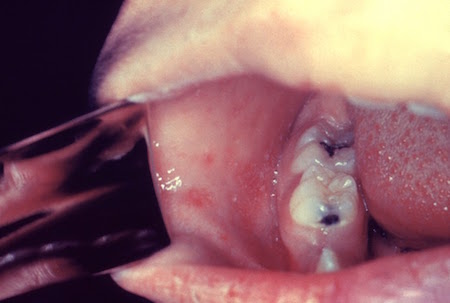
[Figure caption and citation for the preceding image starts]: Koplik's spotsCenters for Disease Control and Prevention [Citation ends].
Measles is caused by a paramyxovirus and is highly contagious. Virus spread occurs via airborne transmission of aerosolised droplet nuclei in closed areas.[34] The incubation period is 11 to 12 days.
During or after a prodrome of fever, cough, coryza, and conjunctivitis, the exanthem of erythematous macules and papules begins on the forehead and behind the ears then spreads cephalocaudally; the rash lasts about 5 days and then begins to fade.
The number of lesions generally increases in the first 2 to 3 days and can become confluent, especially on the face and trunk.[35]
Complications include pneumonia, otitis, myocarditis, encephalitis, and subacute sclerosing panencephalitis.[36]
Erythema infectiosum (fifth disease) is caused by parvovirus B19 and replicates in erythroid progenitor cells, as well as the respiratory epithelium.
Most common in winter and spring.[37]
Common in children aged 4 to 10 years worldwide; often occurs in community-wide epidemics.
The replication occurs during an incubation period of 4 to 14 days.
The rash appears following incubation, typically with bright facial erythema ('slapped cheeks') sparing the nose and perioral area.
One to 4 days later, the second stage of the rash develops, consisting of erythematous macules and papules in a reticulated lacy pattern, primarily on the arms and legs.
The rash lasts 1 to 3 weeks, during which time mild fever and joint pain may be present.
Joint symptoms are more common in adults.
Fetal mortality may be high during the first 20 weeks of gestation; intrauterine transfusion reduces the risk of fetal death.[38][39][40][Figure caption and citation for the preceding image starts]: Erythema infectiosum (Fifth disease) in a 10-year-old girlFrom the personal teaching collection of Hobart W. Walling [Citation ends].

Roseola infantum (sixth disease or exanthem subitum) is caused by human herpesvirus types 6 and 7. This viral illness is common in infancy and early childhood.
Most children are seropositive by age 12 months.[41]
Presents as a high fever for 3 to 5 days, then with the rather abrupt appearance of a generalised rose-pink rash on the trunk and proximal extremities during defervescence.
Red papules and erosions at the soft palate and uvula (Nagayama spots) are characteristic.
Febrile seizures may occur.
Mild upper respiratory symptoms and cervical or occipital lymphadenopathy may be present.
Recovery is usually complete, though re-activation of latent virus is possible.
Acute hepatitis B and C may present with variable cutaneous findings:
May occur during the viraemic phase of acute hepatitis B or hepatitis C infection
Rash may be maculopapular
Other cutaneous findings (including vasculitis, urticaria, lichen planus, cryoglobulinaemia, and porphyria cutanea tarda) may be seen at any stage of infection
Abdominal pain may be present.
Acute HIV infection - acute retroviral syndrome
Patients with suspected HIV exanthem screen positive for HIV viral RNA or core antigen.
After primary HIV infection, 10% to 12% of patients will develop an acute syndrome 3 to 6 weeks after exposure.
Signs and symptoms include a morbilliform eruption, fatigue, malaise, headache, sore throat, lymphadenopathy, and myalgia.[42]
Zika virus is an arthropod-borne flavivirus transmitted primarily by Aedes mosquitoes.
Majority of patients are asymptomatic, but about 20% of infections result in a mild, self-limited illness with vague symptoms, including maculopapular rash, fever, arthralgia, and conjunctivitis.
Rash is characteristic of infection and may be itchy.
Rash most commonly affects the trunk.
About 10% of patients have lower limb petechial purpura, gingival bleeding, or limb oedema.[43]
There is evidence that Zika virus can be sexually transmitted and is a cause of microcephaly and other congenital abnormalities.[44]
Ebola virus is a severe, often fatal, zoonotic infection caused by Ebolavirus.
Incubation period after infection is 1 to 21 days (typically 5-12 days), and patients are not considered infectious until they develop symptoms.
Maculopapular rash developed early in approximately 25% to 52% of patients in previous outbreaks.[45] However, it only developed in 1% to 5% of patients in the 2014 outbreak.[46][47][48]
Frequently described as non-pruritic, erythematous, and maculopapular.
This viral eruption may begin focally, then become diffuse, generalised, and confluent.
Rash may become purpuric or petechial later on in the infection in patients with coagulopathy.[49]
May be difficult to discern the rash in dark-skinned individuals.
Chikungunya is caused by the chikungunya virus and is transmitted to humans via Aedes mosquito bites.
Disease is usually self-limited and characterised by fever, severe arthralgia involving large joints, and rash.
In about half of cases, a maculopapular rash is described, usually associated with the onset of fever, but sometimes occurring after defervescence.
The rash is of global distribution, but most commonly affects the extremities.
The eruption is only occasionally pruritic.
Multiple other dermatological manifestations may occur, including hyperpigmentation of the skin, intertrigo, perigenital and perianal ulcers, skin desquamation especially of the palms and soles, and oral aphthous ulcers.
Dengue fever is a mosquito-borne viral infection caused by any one of four closely related dengue viruses.
Dengue fever is endemic in Southeast Asian and Western Pacific regions, the Caribbean, Latin America, and some regions in the US, Africa, and the Middle East, so travel history is important.
It presents with fever and flushing of the skin of the face and neck before a widespread maculopapular rash develops, affecting the whole body, which may be pruritic.
Other symptoms include myalgia, arthralgia, headache, anorexia, and nausea and vomiting.
If dengue haemorrhagic fever develops, there may be petechiae, epistaxis and signs of bleeding from other sites, hepatosplenomegaly, and subsequent shock.
Mpox, formerly known as monkeypox, is caused by a double-stranded DNA virus.
Incubation period is typically 6 to 13 days (range 1 to 21 days).[50][51]
Presents with characteristic rash that progresses in sequential stages from macules, to papules, vesicles, and pustules.[52][53]
The disease was previously endemic in West and Central Africa; however a global outbreak was identified in May 2022.[54] In the 2022 outbreak, chains of transmission were reported in countries without known epidemiological links to West and Central Africa. The World Health Organization declared the current mpox outbreak in Africa a public health emergency of international concern (PHEIC) in August 2024.[55]
Human‐to‐human transmission can occur through direct contact with skin lesions or infected skin, respiratory droplets and fomites, or through the transplacental route.[56]
The rash typically moves from the facial area distally to the extremities. However, lesions commencing in the genital area (which may be few and at different stages of development, often with only a single lesion observed), and a predisposition for rash to occur without a prodromal phase, have been reported during the 2022 outbreak.[56]
Bacterial infections
Non-toxin-mediated
Rash may be an early presenting sign of meningococcaemia. This exanthem is distinct from the more classic petechial or coalesced purpuric eruption that is frequently found later in the disease process.
Secondary syphilis may also present as a maculopapular eruption on the trunk and extremities, and particularly the palms and soles. Congenital syphilis can present in this way but may also have manifestations of periorificial scaling and vesicles on the palms and soles.[Figure caption and citation for the preceding image starts]: Syphilis presenting with a generalised rashCourtesy of the CDC Public Health Image Library [Citation ends].

Toxin-mediated
Three toxin-mediated bacterial infections may commonly present with a maculopapular eruption: staphylococcal scalded skin syndrome; toxic shock syndrome; scarlet fever.
Staphylococcal scalded skin syndrome is caused by exfoliative toxins ET-A and ET-B from phage group II strains.[57] These toxins target the granular layer of the epidermis, causing loss of adhesion and blistering.
Young children (age ≤6 years) are most commonly affected, though staphylococcal scalded skin syndrome may present in adults with underlying renal insufficiency or immune suppression.[58]
Prodrome of fever, malaise, and tender skin precedes the rash.
Erythema begins on the head and rapidly (hours) generalises.
Skin becomes swollen, and fragile superficial vesicles and bullae form.
Superficial desquamation/exfoliation occurs in 2 to 5 days, leaving denuded and crusted underlying skin. Perioral crusting is seen, with sparing of the oral mucosa.
The diagnosis of staphylococcal scalded skin syndrome is generally made clinically. Patients may develop Nikolsky's sign, in which the epidermal layer sloughs off easily when lateral pressure is applied.
Patients are at high risk for sepsis during the 1- to 2-week period when the skin re-epithelialises. Mortality is low in children (3%) but >50% in adults.[57]
Toxic shock syndrome results from the effects of a Staphylococcus aureus exotoxin (TSS-toxin-1).[59][60] Most cases are post-surgical, but initial reports were associated with menstruation.
Toxic shock syndrome is characterised by high fever (>39.6°C [>103°F]), hypotension (systolic BP <90 mmHg), pharyngitis, headache, gastrointestinal symptoms, and a diffuse scarlatiniform rash.
Diagnosis is made clinically in the presence of fever, hypotension, desquamating rash, and involvement of ≥3 organ systems (gastrointestinal, muscular, central nervous system, renal, hepatic, mucous membranes, or haematological [thrombocytopenia with platelet count <100 x 10⁹/L; 100 x 10³/microlitre]).
The rash starts on the trunk and spreads centripetally.[Figure caption and citation for the preceding image starts]: Morbilliform rash (resembling measles) resulting from toxic shock syndromeCourtesy of the CDC Public Health Image Library [Citation ends].

The extremities become oedematous, and the oral mucosa and tongue become hyperaemic.
Desquamation occurs 1 to 2 weeks after onset, starting on the palms and soles.
Scarlet fever (also known as 'scarlatina') is caused by a toxin produced by group A beta-haemolytic streptococci and is most common in children.[25]
Approximately 90% of cases occur in children younger than 10 years old.[61]
Features of the scarlatiniform rash include a sandpaper-like generalised erythematous rash with discrete skin-coloured papules; linear petechial streaks in skinfolds, particularly axillary, inguinal, and antecubital fossae (Pastia lines).[Figure caption and citation for the preceding image starts]: Scarlet fever rash on the forearm due to group A Streptococcus bacteriaCourtesy of the CDC Public Health Image Library [Citation ends].

The rash is often preceded by a sore throat (pharyngitis, tonsillitis). Other symptoms may include fever, malaise, and gastrointestinal upset. Pharyngeal erythema with exudates, palatal petechiae, and a red, swollen (strawberry) tongue are suggestive features.
In countries such as the UK, where rapid antigen detection tests (RADTs) for scarlet fever are not readily available, test confirmation of group A streptococcus infection is not required before starting antibiotics in patients with a clinical diagnosis of scarlet fever.[62] In countries where RADTs for scarlet fever are available, a positive test result may be required before starting antibiotics (patients with clear viral symptoms don't need testing for group A streptococcal bacteria).[63]
If there is uncertainty about the diagnosis, obtain a throat swab prior to commencing antibiotics.[63][64][65][66] Treatment of scarlet fever with antibiotics based on clinical diagnosis alone should follow in-country clinical guidelines.
According to the UK Health Security Agency, notifications of scarlet fever and invasive group A streptococcus (iGAS) disease in England were higher than expected from September 2022 to February 2023, with the peak observed in December 2022.[64][67] The notifications have significantly reduced since then and are now in line with the expected number for the time of year.[64] Other countries experiencing an increased incidence of scarlet fever and iGAS disease during this period include France, Ireland, the Netherlands, and Sweden. The increase was particularly marked during the second half of 2022.[68]
Erythema multiforme is typically an acute self-limiting, but often relapsing, mucocutaneous inflammatory condition. It is a hypersensitivity reaction associated with certain infections, vaccinations, and, less commonly, medications. The most commonly associated infections are herpes simplex virus and Mycoplasma pneumoniae. Associated drugs include penicillin and sulfonamides. The disease is characterised clinically by target lesions, which can be described as annular erythematous rings with an outer erythematous zone and central blistering sandwiching a zone of normal skin tone. In general, the lesions cover <10% of the total body surface area. Mild symptoms of an upper respiratory infection, including low-grade fever, can sometimes be noted prior to and at the start of an episode. Erosions, blisters, and crusts can be noted in any of the mucous membranes and are typically painful and tender. This can lead to difficulty eating and urinating, requiring hospitalisation.[69]
[Figure caption and citation for the preceding image starts]: Erythema multiforme with target lesionsCourtesy of the CDC Public Health Image Library [Citation ends]. [Figure caption and citation for the preceding image starts]: Erythema multiforme with perioral ulcerationCourtesy of the CDC Public Health Image Library [Citation ends].
[Figure caption and citation for the preceding image starts]: Erythema multiforme with perioral ulcerationCourtesy of the CDC Public Health Image Library [Citation ends].
Rickettsial diseases
Rickettsiae are short gram-negative bacillary organisms transmitted mostly by arthropod vectors (fleas, lice, mites, or ticks).
Tickborne spotted fever rickettsioses are the most frequently reported travel-associated rickettsial infections.
About 20 species are associated with spotted fevers.
Most cases occur in the summer or early autumn.
Approximately half of patients do not recall tick exposure.[70]
Other features of rickettsial disease may include:
Fever, with rash beginning on the wrists and ankles as petechial macules and spreading centrally; occasionally maculopapular lesions develop subsequently
Headache, gastrointestinal symptoms, and malaise (common)
Neurological involvement (uncommon).
Examples include Rocky Mountain spotted fever (US, Canada; Central and South America, including Brazil) and Mediterranean spotted fever (Africa, Europe, India, Middle East).[71]
Systemic or rheumatological disease
Acute graft-versus-host disease (aGVHD)
May occur after allogeneic haematopoietic stem cell transplant. aGVHD may be induced by donor immunocompetent T cells transferred into an immunocompromised host, where the reaction targets the skin (rash), gastrointestinal tract (diarrhoea), and liver (cholestatic hepatitis).
aGVHD incidence ranges from around 30% to more than 50%, but appears to be decreasing over time.[72][73] Frequency depends on the degree of donor and recipient match, occurring in up to 40% of HLA-identical siblings and in more than 50% of those who received transplants from unrelated donors.[73][74][75]
The maculopapular rash is typically erythematous and pruritic. The rash frequently begins on the hands and feet as acral erythema and also favours the upper back, ears, cheeks, and neck. Severe cases may be associated with diffuse erythroderma and desquamation, and mucous membranes (particularly conjunctiva) may be involved. Gastrointestinal tract and liver involvement occur several days after the cutaneous findings appear.[Figure caption and citation for the preceding image starts]: Acute graft-versus-host disease of the skin (grade I)Courtesy of Dr John Levine, Professor, Blood and Marrow Transplantation Program, University of MIchigan; used with permission [Citation ends].

The onset of the rash is usually 1 to 3 weeks after transplantation. The patient is clinically ill and fever is often present.
Half of patients with moderate to severe aGVHD may die as a consequence.[76]
Kawasaki disease (mucocutaneous lymph node syndrome)
An acute multi-system febrile disease that primarily affects children aged <5 years.
Males are more commonly affected than females and in the continental US there are more cases during winter and spring.[77]
The cause is unknown, though an infectious aetiology is surmised.
Diagnostic criteria include fever for 5 days plus at least four of the following five signs:[77][78]
Conjunctival injection
Cervical lymphadenopathy, usually unilateral
Oropharyngeal changes (including hyperaemia, oral fissures, cracked lips, and strawberry tongue)
Peripheral extremity changes (including desquamation of hands and feet, erythema, oedema)
Polymorphous rash.
The rash is typically generalised and maculopapular, without petechiae; perineal erythema is particularly pronounced. The rash resembles a viral exanthem, though recognition is critical due to the possibly life-threatening complications of untreated Kawasaki disease:
Cardiac involvement (the most serious complication), including aneurysms in the coronary arteries (the most common cause of death), myocarditis, and congestive heart failure
Multi-organ involvement (common) affecting the central nervous system, eyes, kidney, and gastrointestinal system (including hydrops of the gallbladder).
Vasculitis of small- and medium-sized vessels contributes to the pathology.
Systemic juvenile idiopathic arthritis (sJIA, formerly known as juvenile rheumatoid arthritis or Still disease) and adult-onset Still disease (when it begins in patients over 16 years of age)
Periodic high fever (often in the late afternoon, spiking in the evening, and resolving) and arthralgias typically precede the eruption.[79]
The eruption of the maculopapular rash associated with sJIA is typically transient (recurring with fever), erythematous, and non-pruritic. The trunk and sites of pressure are favoured.[80]
The maculopapular eruption associated with adult-onset Still disease is salmon-pink, non-pruritic, and accompanies the fever.
The diagnosis may be significantly delayed but is suspected in the context of periodic fevers in the absence of infectious causes, and arthritis.
Use of this content is subject to our disclaimer