Paraphimosis
- Overview
- Theory
- Diagnosis
- Management
- Follow up
- Resources
Treatment algorithm
Please note that formulations/routes and doses may differ between drug names and brands, drug formularies, or locations. Treatment recommendations are specific to patient groups: see disclaimer
with ischaemia and necrosis
emergency surgery
Patients with evidence of significant glans penis ischaemia, with necrosis and sloughing of the foreskin and/or glans, require involvement of a urology consultant.
They will require procedural sedation or general anaesthesia followed by immediate reduction using invasive techniques.
Devitalised tissue will require operative debridement.
acute type without ischaemia and necrosis
manual manipulation
This is performed to reduce swelling and to replace the foreskin over the glans penis.
Before manipulation, a topical analgesic or injection of a local anaesthetic is required. Young boys often require parenteral administration of opioids and sedative agents in addition to local anaesthesia. Acupuncture is a non-pharmacological option for pain management.[17]Tsai SL, Reynoso E, Shin DW, et al. Acupuncture as a nonpharmacologic treatment for pain in a pediatric emergency department. Pediatr Emerg Care. 2018 Sep 21 [Epub ahead of print]. http://www.ncbi.nlm.nih.gov/pubmed/30247457?tool=bestpractice.com
Ice, compression, or an osmotic agent may be applied after the anaesthesia.[18]Turner CD, Kim HL, Cromie WJ. Dorsal band traction for reduction of paraphimosis. Urology. 1999 Nov;54(5):917-8. http://www.ncbi.nlm.nih.gov/pubmed/10565759?tool=bestpractice.com
Ice packs can be applied to the penis after the penis has been wrapped in plastic.
Compression is commonly performed using a gloved hand but can also be achieved by a 2 x 2-inch bandage. The oedematous glans and foreskin should be compressed until swelling is noted to improve. This technique is successful in the majority of boys with paraphimosis.
Osmotic agent (e.g., fine granulated sugar) is applied in liberal amounts, on the principle that fluid flows down a concentration gradient; in this case the hypotonic fluid in the penis flows to the hypertonic agent on the outside of the skin.[20]Kerwat R, Shandall A, Stephenson B. Reduction of paraphimosis with granulated sugar. Br J Urol. 1998 Nov;82(5):755. http://www.ncbi.nlm.nih.gov/pubmed/9839597?tool=bestpractice.com
Once foreskin swelling has been reduced as much as possible, manual reduction is performed by pulling the phimotic ring while pushing down on the glans.[18]Turner CD, Kim HL, Cromie WJ. Dorsal band traction for reduction of paraphimosis. Urology. 1999 Nov;54(5):917-8.
http://www.ncbi.nlm.nih.gov/pubmed/10565759?tool=bestpractice.com
[Figure caption and citation for the preceding image starts]: Pre-reduction of paraphimosisFrom the collection of Dr Michelle Semins and Dr Adam Kern [Citation ends]. [Figure caption and citation for the preceding image starts]: Process of manual manipulation of paraphimosisFrom the collection of Dr Michelle Semins and Dr Adam Kern [Citation ends].
[Figure caption and citation for the preceding image starts]: Process of manual manipulation of paraphimosisFrom the collection of Dr Michelle Semins and Dr Adam Kern [Citation ends].
[Figure caption and citation for the preceding image starts]: Diagram illustrating the technique for manual reduction of paraphimosisFrom the collection of Dr Ranjiv Mathews [Citation ends].
puncture technique
This may be used after failed attempts at reduction using minimally invasive procedures.
Perforation of the foreskin at multiple locations (the Dundee technique) allows exudation of the oedematous fluid and reduction in swelling.[13]Reynard JM, Barua JM. Reduction of paraphimosis the simple way - the Dundee technique. BJU Int. 1999 May;83(7):859-60. http://www.ncbi.nlm.nih.gov/pubmed/10368214?tool=bestpractice.com [21]Barone JG, Fleisher MH. Treatment of paraphimosis using the "puncture" technique. Pediatr Emerg Care. 1993 Oct;9(5):298-9. http://www.ncbi.nlm.nih.gov/pubmed/8247937?tool=bestpractice.com
After appropriate local analgesia and sedation, multiple punctures are made in the oedematous foreskin using a 22-gauge hypodermic needle.
Subsequently, the foreskin is reduced by manual compression and reduction.
hyaluronidase
Additional treatment recommended for SOME patients in selected patient group
This natural protein may be used to augment the puncture technique.[22]DeVries CR, Miller AK, Packer MG. Reduction of paraphimosis with hyaluronidase. Urology. 1996 Sep;48(3):464-5. http://www.ncbi.nlm.nih.gov/pubmed/8804504?tool=bestpractice.com
Injection of hyaluronidase into the oedematous foreskin leads to degradation of hyaluronic acid and reduction of oedema.
As the swelling subsides, reduction can be attempted.
Primary options
hyaluronidase: refer to consultant for guidance on dose
surgical reduction followed by circumcision
This is reserved for patients who fail conservative attempts at reduction.
Although in very infirm and older people this can be performed at the bedside using a penile block (i.e., local anaesthetic plus procedural sedation), in most patients general anaesthesia will be required.
For the dorsal slit procedure, the phimotic ring is incised on the dorsal aspect of the penis until release of the foreskin is identified. [Figure caption and citation for the preceding image starts]: Dorsal slit for management of paraphimosisFrom the collection of Dr Ranjiv Mathews [Citation ends]. [Figure caption and citation for the preceding image starts]: Dorsal slit for management of paraphimosisFrom the collection of Dr Ranjiv Mathews [Citation ends].
[Figure caption and citation for the preceding image starts]: Dorsal slit for management of paraphimosisFrom the collection of Dr Ranjiv Mathews [Citation ends]. This allows the swelling to subside. The edges are closed using 4-0 chromic suture or similar.
This allows the swelling to subside. The edges are closed using 4-0 chromic suture or similar.
Completion of the circumcision is performed as a second procedure, once the swelling of the foreskin has subsided. [Figure caption and citation for the preceding image starts]: Completed dorsal slit and reduction of the paraphimosisFrom the collection of Dr Ranjiv Mathews [Citation ends].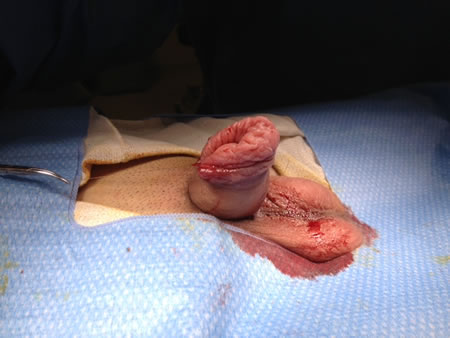
chronic type without ischaemia and necrosis
surgical reduction followed by circumcision
Patients with the chronic form of paraphimosis should undergo surgical reduction followed by circumcision as first-line therapy.
Although in very infirm and older people this can be performed at the bedside using a penile block (i.e., local anaesthetic plus procedural sedation), in most patients general anaesthesia will be required.
For the dorsal slit procedure, the phimotic ring is incised on the dorsal aspect of the penis until release of the foreskin is identified. [Figure caption and citation for the preceding image starts]: Dorsal slit for management of paraphimosisFrom the collection of Dr Ranjiv Mathews [Citation ends]. [Figure caption and citation for the preceding image starts]: Dorsal slit for management of paraphimosisFrom the collection of Dr Ranjiv Mathews [Citation ends].
[Figure caption and citation for the preceding image starts]: Dorsal slit for management of paraphimosisFrom the collection of Dr Ranjiv Mathews [Citation ends]. This allows the swelling to subside. The edges are closed using 4-0 chromic suture or similar.
This allows the swelling to subside. The edges are closed using 4-0 chromic suture or similar.
Completion of the circumcision is performed as a second procedure, once the swelling of the foreskin has subsided. [Figure caption and citation for the preceding image starts]: Completed dorsal slit and reduction of the paraphimosisFrom the collection of Dr Ranjiv Mathews [Citation ends].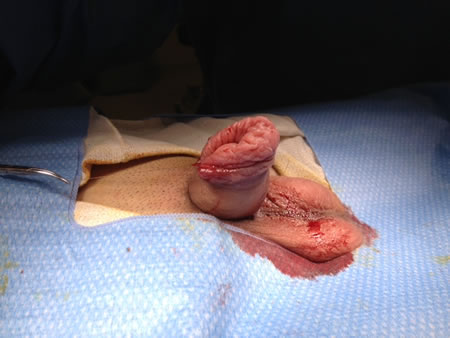

Choose a patient group to see our recommendations
Please note that formulations/routes and doses may differ between drug names and brands, drug formularies, or locations. Treatment recommendations are specific to patient groups. See disclaimer
Use of this content is subject to our disclaimer