The diagnosis of diphtheria is established by a combination of history, physical examination, and positive cultures from throat swabs, or other suspect lesions, for Corynebacterium diphtheriae. Polymerase chain reaction (PCR) testing can provide supporting evidence for the diagnosis of diphtheria and help to discriminate between toxigenic and non-toxigenic strains.The Elek test is a phenotypic test of toxin production.[40]Centers for Disease Control and Prevention. Manual for the surveillance of vaccine-preventable diseases: chapter 22: laboratory support for surveillance of vaccine-preventable diseases. Mar 2024 [internet publication].
https://www.cdc.gov/surv-manual/php/table-of-contents/chapter-22-laboratory-support.html
[41]UK Health Security Agency. Public health control and management of diphtheria in England: 2023 guidelines. Nov 2023 [internet publication].
https://assets.publishing.service.gov.uk/media/654944a9bdb7ef000d4af91c/diphtheria-guidelines-version19-November2023.pdf
[42]World Health Organization. WHO laboratory manual for the diagnosis of diphtheria and other related infections. 2021 [internet publication].
https://apps.who.int/iris/handle/10665/352275
History
In respiratory diphtheria, symptoms typically begin with a sore throat and fever. As the disease progresses, dysphagia, dysphonia, dyspnoea, and a croupy cough can develop, which signal pharyngeal and laryngeal extension of the pseudomembrane and/or neurological involvement of the posterior pharyngeal and laryngeal nerves.[13]Sharma NC, Efstratiou A, Mokrousov I, et al. Diphtheria. Nat Rev Dis Primers. 2019 Dec 5;5(1):81.
https://www.doi.org/10.1038/s41572-019-0131-y
http://www.ncbi.nlm.nih.gov/pubmed/31804499?tool=bestpractice.com
[28]World Health Organization. Diphtheria vaccines: WHO position paper - August 2017. Wkly Epidemiol Rec. 2017 Aug 4;92(31):417-35.
https://www.who.int/publications/i/item/who-wer9231
http://www.ncbi.nlm.nih.gov/pubmed/28776357?tool=bestpractice.com
The risk of death from respiratory compromise and aspiration increases significantly when this occurs.
Obtaining a thorough history of previous immunisations, including diphtheria vaccination, is vital. Where possible, obtain an immunisation history from close contacts as well. A history of travel and/or exposure to sick individuals should also be sought.
Diphtheria remains endemic in Haiti and the Dominican Republic, and many countries in Asia, the South Pacific, and the Middle East.[12]Centers for Disease Control and Prevention. CDC Yellow Book 2024: health information for international travel. Section 5: travel-associated infections & diseases: diphtheria. May 2023 [internet publication].
https://wwwnc.cdc.gov/travel/yellowbook/2024/infections-diseases/diphtheria
In cutaneous diphtheria, a history of underlying skin dermatoses in the setting of residential crowding or homelessness is typical. Cutaneous diphtheria should also be considered in travellers with wound infections who have arrived from countries where infection is endemic.[31]Griffith J, Bozio CH, Poel AJ, et al. Imported toxin-producing cutaneous diphtheria - Minnesota, Washington, and New Mexico, 2015-2018. MMWR Morb Mortal Wkly Rep. 2019 Mar 29;68(12):281-4.
https://www.cdc.gov/mmwr/volumes/68/wr/mm6812a2.htm?s_cid=mm6812a2_w
http://www.ncbi.nlm.nih.gov/pubmed/30921303?tool=bestpractice.com
Initially, infected skin lesions tend to be shallow, painful, tender, and erythematous; by the time of presentation they are often ulcerated. Skin lesions tend to form on the extremities as these parts of the body have the greatest risk of acquiring cuts and abrasions, which then become secondarily infected with C diphtheriae.
Physical examination
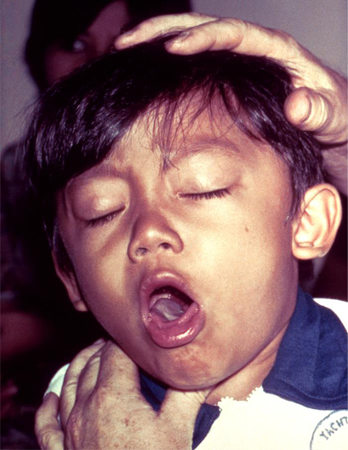
If the upper respiratory tract is involved, a typical brown-greyish pseudomembrane begins to form over the tonsils and/or pharynx after 2 to 5 days of sore throat. It will typically bleed after attempts to remove or dislodge it.[12]Centers for Disease Control and Prevention. CDC Yellow Book 2024: health information for international travel. Section 5: travel-associated infections & diseases: diphtheria. May 2023 [internet publication].
https://wwwnc.cdc.gov/travel/yellowbook/2024/infections-diseases/diphtheria
Without prompt treatment, this pseudomembrane can thicken and spread to involve other parts of the oropharynx, nasopharynx, larynx, and trachea. Swelling of the neck and lymphadenopathy lead to a characteristic bull-neck appearance.
In cutaneous diphtheria, sharply defined, painful lesions that frequently ulcerate and are covered by a brownish-grey membrane may be noted.[2]Centers for Disease Control and Prevention. Diphtheria: clinical features of diphtheria. Feb 2024 [internet publication].
https://www.cdc.gov/diphtheria/hcp/clinical-signs
[13]Sharma NC, Efstratiou A, Mokrousov I, et al. Diphtheria. Nat Rev Dis Primers. 2019 Dec 5;5(1):81.
https://www.doi.org/10.1038/s41572-019-0131-y
http://www.ncbi.nlm.nih.gov/pubmed/31804499?tool=bestpractice.com
[Figure caption and citation for the preceding image starts]: A typical pseudomembrane in a diphtheria patientPublic Health Image Library (PHIL), CDC [Citation ends].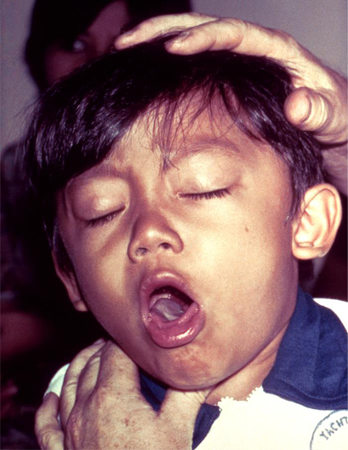 [Figure caption and citation for the preceding image starts]: Corynebacterium diphtheriae taken from an 18-hour culture, using Albert stainPublic Health Image Library (PHIL), CDC [Citation ends].
[Figure caption and citation for the preceding image starts]: Corynebacterium diphtheriae taken from an 18-hour culture, using Albert stainPublic Health Image Library (PHIL), CDC [Citation ends]. [Figure caption and citation for the preceding image starts]: Cutaneous diphtheria: note the deep ulcer with well-defined marginsPublic Health Image Library (PHIL), CDC [Citation ends].
[Figure caption and citation for the preceding image starts]: Cutaneous diphtheria: note the deep ulcer with well-defined marginsPublic Health Image Library (PHIL), CDC [Citation ends]. [Figure caption and citation for the preceding image starts]: Skin lesion caused by the Corynebacterium diphtheriaePublic Health Image Library (PHIL), CDC [Citation ends].
[Figure caption and citation for the preceding image starts]: Skin lesion caused by the Corynebacterium diphtheriaePublic Health Image Library (PHIL), CDC [Citation ends].
Laboratory testing
The diagnosis of diphtheria requires confirmation by microbiological culture and microscopy. This requires the use of blood agar and a blood agar medium containing tellurite (Hoyle’s), or Tinsdale media.[42]World Health Organization. WHO laboratory manual for the diagnosis of diphtheria and other related infections. 2021 [internet publication].
https://apps.who.int/iris/handle/10665/352275
Nose and throat swabs are taken for culture or molecular testing in suspected respiratory diphtheria patients and their close contacts. Where possible, swabs should be taken from beneath the pseudomembrane, taking care not to dislodge it, exacerbate respiratory obstruction, or cause it to bleed.
Culture distinguishes C diphtheriae from other Corynebacterium species that are part of the natural flora of the nasopharynx and skin (e.g., diphtheroids).[40]Centers for Disease Control and Prevention. Manual for the surveillance of vaccine-preventable diseases: chapter 22: laboratory support for surveillance of vaccine-preventable diseases. Mar 2024 [internet publication].
https://www.cdc.gov/surv-manual/php/table-of-contents/chapter-22-laboratory-support.html
Even if the patient's culture is negative, isolation of C diphtheriae from close contacts may enable confirmation of the diagnosis.[1]Centers for Disease Control and Prevention. Manual for the surveillance of vaccine-preventable diseases. Chapter 1: diphtheria. Dec 2022 [internet publication].
https://www.cdc.gov/vaccines/pubs/surv-manual/chpt01-dip.html
A modified Elek test is the gold standard to determine the toxigenicity of isolated C diphtheriae strains, but this is a technically difficult test and is not always available, particularly in outbreak settings.[40]Centers for Disease Control and Prevention. Manual for the surveillance of vaccine-preventable diseases: chapter 22: laboratory support for surveillance of vaccine-preventable diseases. Mar 2024 [internet publication].
https://www.cdc.gov/surv-manual/php/table-of-contents/chapter-22-laboratory-support.html
[42]World Health Organization. WHO laboratory manual for the diagnosis of diphtheria and other related infections. 2021 [internet publication].
https://apps.who.int/iris/handle/10665/352275
In the US, the Centers for Disease Control and Prevention (CDC) has the only laboratory able to perform Elek testing.[12]Centers for Disease Control and Prevention. CDC Yellow Book 2024: health information for international travel. Section 5: travel-associated infections & diseases: diphtheria. May 2023 [internet publication].
https://wwwnc.cdc.gov/travel/yellowbook/2024/infections-diseases/diphtheria
PCR is therefore often useful as an initial toxigenicity test. PCR testing can help to discriminate between toxigenic and non-toxigenic strains by detecting genes associated with the diphtheria toxin (dtxR and tox).[40]Centers for Disease Control and Prevention. Manual for the surveillance of vaccine-preventable diseases: chapter 22: laboratory support for surveillance of vaccine-preventable diseases. Mar 2024 [internet publication].
https://www.cdc.gov/surv-manual/php/table-of-contents/chapter-22-laboratory-support.html
[41]UK Health Security Agency. Public health control and management of diphtheria in England: 2023 guidelines. Nov 2023 [internet publication].
https://assets.publishing.service.gov.uk/media/654944a9bdb7ef000d4af91c/diphtheria-guidelines-version19-November2023.pdf
[42]World Health Organization. WHO laboratory manual for the diagnosis of diphtheria and other related infections. 2021 [internet publication].
https://apps.who.int/iris/handle/10665/352275
It discriminates toxigenic from non-toxigenic bacteria in most cases, though it is important to remember that non-toxigenic toxin gene bearing strains of C diphtheriae occasionally occur.[42]World Health Organization. WHO laboratory manual for the diagnosis of diphtheria and other related infections. 2021 [internet publication].
https://apps.who.int/iris/handle/10665/352275
As culture-based isolation of C diphtheriae is often unsuccessful once antibiotic treatment has been initiated, PCR can also be useful because it still identifies non-viable C diphtheriae organisms from clinical specimens.
Diphtheria antibody levels can also be measured. If levels are high, the disease is less likely to produce a severe illness. However, serology is infrequently available and of limited utility; it is not useful after antitoxin has been administered. If antibody titres are low (a non-protective diphtheria antibody titre is <0.01 IU/mL), a diagnosis of diphtheria cannot be excluded.[40]Centers for Disease Control and Prevention. Manual for the surveillance of vaccine-preventable diseases: chapter 22: laboratory support for surveillance of vaccine-preventable diseases. Mar 2024 [internet publication].
https://www.cdc.gov/surv-manual/php/table-of-contents/chapter-22-laboratory-support.html
[42]World Health Organization. WHO laboratory manual for the diagnosis of diphtheria and other related infections. 2021 [internet publication].
https://apps.who.int/iris/handle/10665/352275
Reporting
In the UK, US, and other countries, diphtheria is a notifiable disease, with local or national guidelines indicating the reporting requirements.[1]Centers for Disease Control and Prevention. Manual for the surveillance of vaccine-preventable diseases. Chapter 1: diphtheria. Dec 2022 [internet publication].
https://www.cdc.gov/vaccines/pubs/surv-manual/chpt01-dip.html
[41]UK Health Security Agency. Public health control and management of diphtheria in England: 2023 guidelines. Nov 2023 [internet publication].
https://assets.publishing.service.gov.uk/media/654944a9bdb7ef000d4af91c/diphtheria-guidelines-version19-November2023.pdf
[42]World Health Organization. WHO laboratory manual for the diagnosis of diphtheria and other related infections. 2021 [internet publication].
https://apps.who.int/iris/handle/10665/352275
Suspected diphtheria cases should be reported promptly to relevant public health authorities so that diphtheria antitoxin can be obtained.
 [Figure caption and citation for the preceding image starts]: Corynebacterium diphtheriae taken from an 18-hour culture, using Albert stainPublic Health Image Library (PHIL), CDC [Citation ends].
[Figure caption and citation for the preceding image starts]: Corynebacterium diphtheriae taken from an 18-hour culture, using Albert stainPublic Health Image Library (PHIL), CDC [Citation ends]. [Figure caption and citation for the preceding image starts]: Cutaneous diphtheria: note the deep ulcer with well-defined marginsPublic Health Image Library (PHIL), CDC [Citation ends].
[Figure caption and citation for the preceding image starts]: Cutaneous diphtheria: note the deep ulcer with well-defined marginsPublic Health Image Library (PHIL), CDC [Citation ends]. [Figure caption and citation for the preceding image starts]: Skin lesion caused by the Corynebacterium diphtheriaePublic Health Image Library (PHIL), CDC [Citation ends].
[Figure caption and citation for the preceding image starts]: Skin lesion caused by the Corynebacterium diphtheriaePublic Health Image Library (PHIL), CDC [Citation ends].