Investigations
1st investigations to order
brain MRI
Test
MRI is the most specific and sensitive test for evaluation of tumour and assessment of associated brain or spinal metastases.
MRI is performed with and without gadolinium.[3][35]
Order test in: patients with morning headaches, intermittent headaches increasing in frequency or intensity, or persistent daily headaches lasting >1 week; infants with an increasing head circumference or a bulging fontanelle; patients with an impaired upward gaze; and ataxic patients.[24]
The advantage of MRI over CT is that it gives a better anatomical view of the brain with no exposure to radiation.[32][Figure caption and citation for the preceding image starts]: MRI: axial view of medulloblastoma, T1WI with gadolinium, showing an avidly enhancing solid and cystic lesion filling the fourth ventricleFrom the collection of Peter B. Storm; used with permission [Citation ends].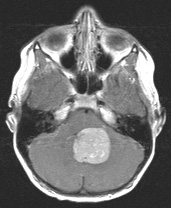 [Figure caption and citation for the preceding image starts]: MRI: coronal view of medulloblastoma, T1WI with gadolinium, showing an avidly enhancing solid and cystic lesion filling the fourth ventricle; obstructive hydrocephalus presentFrom the collection of Peter B. Storm; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: MRI: coronal view of medulloblastoma, T1WI with gadolinium, showing an avidly enhancing solid and cystic lesion filling the fourth ventricle; obstructive hydrocephalus presentFrom the collection of Peter B. Storm; used with permission [Citation ends].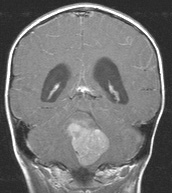
Brain MRI may be complemented by advanced neuroimaging techniques such as MR perfusion imaging, MR spectroscopy, and PET, to enhance diagnostic capability, differentiate active neoplasm, and guide biopsy.
Result
lateral cerebellar hemisphere or fourth ventricular mass arising from the cerebellar vermis or dorsal brain stem with enhancement after gadolinium; obstructive hydrocephalus
brain CT
Test
CT is useful for rapid assessment in the acute setting, or if MRI is unavailable/contraindicated.[3] Advantages of CT over MRI are that it is quicker, does not require sedation, and is easier to obtain urgently. CT is not appropriate for staging tumours.
Order test in: patients with morning headaches, intermittent headaches increasing in frequency or intensity, or persistent daily headaches lasting >1 week; infants with an increasing head circumference or a bulging fontanelle; patients with an impaired upward gaze; ataxic patients.[24]
Result
lateral cerebellar hemisphere or fourth ventricular mass arising from the cerebellar vermis or dorsal brain stem with enhancement after gadolinium; hyperdense, rarely calcified; obstructive hydrocephalus
histology
Test
Variable cellular atypia is seen, ranging from small cells with rare mitoses to extreme atypia with mitotically active cells.
Homer Wright rosette is a spherical group of dark tumour cells around a pale, eosinophilic, central area that contains neurofibrils but lacks a lumen.
Additional immunostaining may be useful for initial molecular characterisation.
In consultation with pathology, molecular analysis of the tumour should be performed for diagnosis, molecular subgrouping, and risk classification purposes. Analysis may include next generation whole exome/genome DNA sequencing, RNA sequencing and DNA methylation. A blood sample from the patient for corresponding germline sequencing should also be obtained and analysed in concert with the tumour sample. Germline testing may identify underlying germline cancer predispositions that could impact treatment and prognosis.
Result
variable depending on the sub-type; classical medulloblastoma has typical appearances with monotonous small cells, atypia, Homer Wright rosette; immunohistochemistry will show positivity for INI-1 (tumour suppressor gene) and the glycoprotein synaptophysin, variable reactivity for GFAP, EMA and cytokeratin; wingless (WNT)-activated medulloblastoma will be positive for nuclear beta-catenin, often with positive YAP1; sonic hedgehog (SHH)-activated medulloblastoma will be positive for GAB1 and YAP1, with cytoplasmic beta-catenin staining; non-WNT/non-SHH medulloblastoma will be negative for all three markers
cervical, thoracic, and lumbar spine MRI
Test
A careful metastatic evaluation with a non-enhanced and contrast-enhanced MRI of the brain and whole spine is mandatory.[3][Figure caption and citation for the preceding image starts]: MRI: sagittal view of medulloblastoma, T1WI with gadolinium, showing multiple avidly enhancing drop metastases from the patient's posterior fourth ventricular medulloblastomaFrom the collection of Peter B. Storm; used with permission [Citation ends].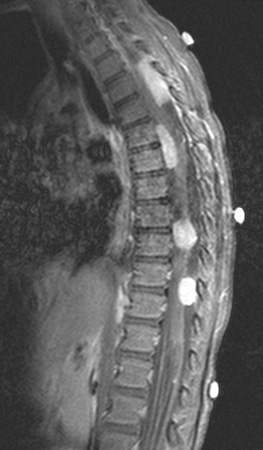
Result
possible evidence of leptomeningeal metastases
lumbar puncture
Test
Cerebrospinal fluid (CSF) should be examined for tumour cells following recovery from surgery. CSF taken by lumbar puncture at least 10 days after surgery has been shown to be more reliable than ventricular CSF for staging purposes.[3][25][34] All patients should have a lumbar puncture even in the absence of metastatic tumour on brain and spine MRI.[33]
Result
malignant cells if has spread to the CSF
postoperative MRI
Test
Postoperative MRI is essential to evaluate the extent of resection and should be performed within 72 hours of tumour resection, ideally within 24 hours, after which time postoperative changes render interpretation of residual disease difficult.[3] If it cannot be performed in that timeframe, then it should not be performed for at least 10 days after surgery.
Result
possible residual disease
Use of this content is subject to our disclaimer