Surgery is almost always performed, regardless of age, in order to:[2]Van Effenterre R, Boch AL. Craniopharyngioma in adults and children: a study of 122 surgical cases. J Neurosurg. 2002 Jul;97(1):3-11.
http://www.ncbi.nlm.nih.gov/pubmed/12134929?tool=bestpractice.com
[11]Garre ML, Cama A. Craniopharyngioma: modern concepts in pathogenesis and treatment. Curr Opin Pediatr. 2007 Aug;19(4):471-9.
http://www.ncbi.nlm.nih.gov/pubmed/17630614?tool=bestpractice.com
[14]Puget S, Garnett M, Wray A, et al. Pediatric craniopharyngiomas: classification and treatment according to the degree of hypothalamic involvement. J Neurosurg. 2007 Jan;106(1 suppl):3-12.
http://www.ncbi.nlm.nih.gov/pubmed/17233305?tool=bestpractice.com
[28]Fischer EG, Welch K, Shillito J, et al. Craniopharyngiomas in children. Long-term effects of conservative surgical procedures combined with radiation therapy. J Neurosurg. 1990 Oct;73(4):534-40.
http://www.ncbi.nlm.nih.gov/pubmed/2398383?tool=bestpractice.com
[29]Clark AJ, Cage TA, Aranda D, et al. Treatment-related morbidity and the management of pediatric craniopharyngioma: a systematic review. J Neurosurg Pediatr. 2012 Oct;10(4):293-301.
http://www.ncbi.nlm.nih.gov/pubmed/22920295?tool=bestpractice.com
[30]Hankinson TC, Palmeri NO, Williams SA, et al. Patterns of care for craniopharyngioma: survey of members of the american association of neurological surgeons. Pediatr Neurosurg. 2013;49(3):131-6.
http://www.ncbi.nlm.nih.gov/pubmed/24577430?tool=bestpractice.com
[31]Mortini P, Losa M, Pozzobon G, et al. Neurosurgical treatment of craniopharyngioma in adults and children: early and long-term results in a large case series. J Neurosurg. 2011 May;114(5):1350-9.
http://www.ncbi.nlm.nih.gov/pubmed/21214336?tool=bestpractice.com
Surgery relieves raised intracranial pressure, if present (with or without cerebrospinal fluid [CSF] shunting), and may reverse visual compromise due to compression by tumour (improvement in nearly 40% of patients).
Surgery may include biopsy only, cyst aspiration, CSF shunting, or tumour resection (either partial or complete).
Contrast-enhanced brain imaging (magnetic resonance imaging [MRI]/computed tomography [CT]) helps determine the surgical approach and provides a baseline for evaluating residual disease and response to treatment.
Baseline endocrine and ophthalmological evaluations with appropriate consultations must be performed to aid in monitoring effects of surgery upon endocrine function.[6]Defoort-Dhellemmes S, Moritz F, Bouacha I, et al. Craniopharyngioma: ophthalmological aspects at diagnosis. J Pediatr Endocrinol Metab. 2006 Apr;19(suppl 1):321-4.
http://www.ncbi.nlm.nih.gov/pubmed/16700306?tool=bestpractice.com
[8]Halac I, Zimmerman D. Endocrine manifestations of craniopharyngioma. Childs Nerv Syst. 2005 Aug;21(8-9):640-8.
https://link.springer.com/article/10.1007%2Fs00381-005-1246-x
http://www.ncbi.nlm.nih.gov/pubmed/16047216?tool=bestpractice.com
[9]Hopper N, Albanese A, Ghirardello S, et al. The preoperative endocrine assessment of craniopharyngiomas. J Pediatr Endocrinol Metab. 2006 Apr;19(suppl 1):325-7.
http://www.ncbi.nlm.nih.gov/pubmed/16700307?tool=bestpractice.com
[24]Sorva R, Heiskanen O, Perheetupa J. Craniopharyngioma surgery in children: endocrine and visual outcome. Childs Nerv Syst. 1988 Apr;4(2):97-9.
http://www.ncbi.nlm.nih.gov/pubmed/3401877?tool=bestpractice.com
However, detailed endocrinological evaluation should not delay surgery in cases of rapid deterioration of vision.
Following primary surgery, radiotherapy may be required.[32]Stripp DC, Maity A, Janss AJ, et al. Surgery with or without radiation therapy in the management of craniopharyngiomas in children and young adults. Int J Radiat Oncol Biol Phys. 2004 Mar 1;58(3):714-20.
http://www.ncbi.nlm.nih.gov/pubmed/14967425?tool=bestpractice.com
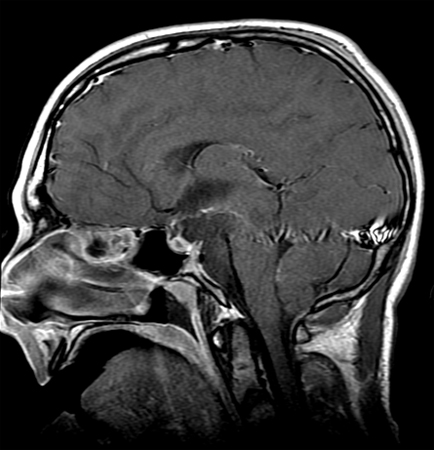
As endocrinopathies are common (both pre- and postoperatively), hormone replacement therapy is usually necessary, depending upon the specific endocrine deficiencies.[Figure caption and citation for the preceding image starts]: Craniopharyngioma: sagittal post-contrast MRIFrom the collection of Marc C. Chamberlain [Citation ends].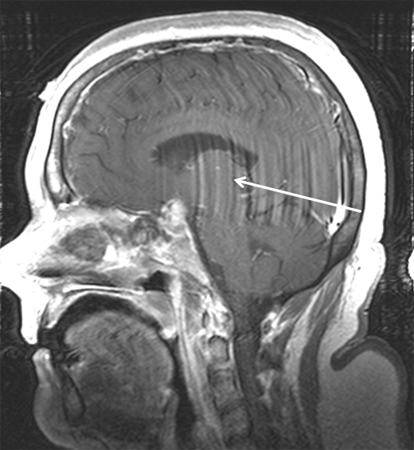 [Figure caption and citation for the preceding image starts]: Craniopharyngioma (postoperative): sagittal post-contrast MRIFrom the collection of Marc C. Chamberlain [Citation ends].
[Figure caption and citation for the preceding image starts]: Craniopharyngioma (postoperative): sagittal post-contrast MRIFrom the collection of Marc C. Chamberlain [Citation ends].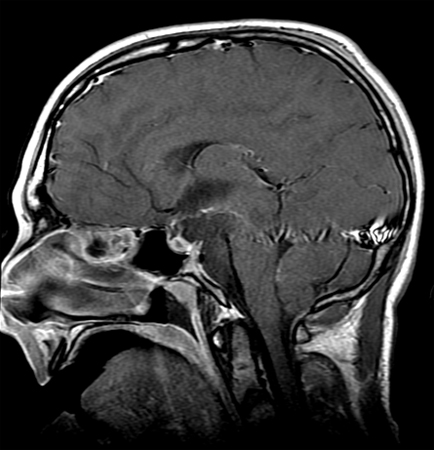
Surgery
The extent of surgical resection and the potential risks of surgery depend on tumour size and location.[10]Dhellemmes P, Vinchon M. Radical resection for craniopharyngiomas in children: surgical technique and clinical results. J Pediatr Endocrinol Metab. 2006 Apr;19(suppl 1):329-35.
http://www.ncbi.nlm.nih.gov/pubmed/16700308?tool=bestpractice.com
[14]Puget S, Garnett M, Wray A, et al. Pediatric craniopharyngiomas: classification and treatment according to the degree of hypothalamic involvement. J Neurosurg. 2007 Jan;106(1 suppl):3-12.
http://www.ncbi.nlm.nih.gov/pubmed/17233305?tool=bestpractice.com
[29]Clark AJ, Cage TA, Aranda D, et al. Treatment-related morbidity and the management of pediatric craniopharyngioma: a systematic review. J Neurosurg Pediatr. 2012 Oct;10(4):293-301.
http://www.ncbi.nlm.nih.gov/pubmed/22920295?tool=bestpractice.com
[33]Komotar RJ, Starke RM, Raper DM, et al. Endoscopic skull base surgery: a comprehensive comparison with open transcranial approaches. Br J Neurosurg. 2012 Oct;26(5):637-48.
http://www.ncbi.nlm.nih.gov/pubmed/22324437?tool=bestpractice.com
[34]Hoffman HJ, De Silva M, Humphreys RP, et al. Aggressive surgical management of craniopharyngiomas in children. J Neurosurg. 1992 Jan;76(1):47-52.
http://www.ncbi.nlm.nih.gov/pubmed/1727168?tool=bestpractice.com
Gross total resection should be achieved if possible; however, while maximising resection, long-term side effects should also be minimised, bearing in mind the availability of adjuvant radiotherapy for subtotally resected lesions.
When adherent to nearby structures, such as the basilar artery, hypothalamus, or optic chiasm, surgery may be limited. In these cases, tissue biopsy for diagnosis and decompression of important anatomical structures is often attempted, without complete resection. Caution is required if intracystic therapies are used, as leakage carries toxicity to the optic structures and perforator vessels.
Surgical approach
Depends upon the anatomy (relationship to the sella, optic chiasm, and third ventricle) and size of the tumour as determined preoperatively by cranial MRI.[27]Curran JG, O'Connor E. Imaging of craniopharyngioma. Childs Nerv Syst. 2005 Aug;21(8-9):635-9.
http://www.ncbi.nlm.nih.gov/pubmed/16078078?tool=bestpractice.com
A number of surgical approaches may be used:
Transcortical or transcallosal approaches allow a transventricular (from above) approach, which is indicated for tumours that involve the third ventricle and are above the optic chiasm
Sub-frontal and interhemispheric approaches (from underneath or between the frontal lobes) are indicated for tumours located anterior to the optic chiasm or just behind the lamina terminalis
Pterional approach (fronto-temporal window, through the opened Sylvian fissure) is used for small tumours in close proximity to the optic chiasm
Trans-sphenoidal approach (either transnasal or sub-labial) is utilised if the tumour is partly or totally intrasellar (pituitary fossa)
Endoscopic endonasal surgery is increasingly used (especially in children) for suprasellar as well as sellar tumours, due to a decreased risk of hypothalamic injury and higher chance of gross total resection.[35]Fong RP, Babu CS, Schwartz TH. Endoscopic endonasal approach for craniopharyngiomas. J Neurosurg Sci. 2021 Apr;65(2):133-9.
http://www.ncbi.nlm.nih.gov/pubmed/33890754?tool=bestpractice.com
[36]Soldozy S, Yeghyayan M, Yağmurlu K, et al. Endoscopic endonasal surgery outcomes for pediatric craniopharyngioma: a systematic review. Neurosurg Focus. 2020 Jan 1;48(1):E6.
https://thejns.org/focus/view/journals/neurosurg-focus/48/1/article-pE6.xml
http://www.ncbi.nlm.nih.gov/pubmed/31896083?tool=bestpractice.com
It is typically trans-sphenoidal, with more expanded approaches used for larger craniopharyngiomas.
For multi-compartmental tumours, a combined approach using two or more of these options may be used.[10]Dhellemmes P, Vinchon M. Radical resection for craniopharyngiomas in children: surgical technique and clinical results. J Pediatr Endocrinol Metab. 2006 Apr;19(suppl 1):329-35.
http://www.ncbi.nlm.nih.gov/pubmed/16700308?tool=bestpractice.com
[34]Hoffman HJ, De Silva M, Humphreys RP, et al. Aggressive surgical management of craniopharyngiomas in children. J Neurosurg. 1992 Jan;76(1):47-52.
http://www.ncbi.nlm.nih.gov/pubmed/1727168?tool=bestpractice.com
Surgical complications include risk of arterial injury (anterior cerebral arteries and the basilar artery), pituitary dysfunction, diabetes insipidus, visual loss, and hypothalamic dysfunction. A higher incidence of hormone deficiency has been reported among paediatric patients undergoing complete resection compared with those managed with conservative surgery followed by adjuvant radiotherapy.[37]Tan TSE, Patel L, Gopal-Kothandapani JS, et al. The neuroendocrine sequelae of paediatric craniopharyngioma: a 40-year meta-data analysis of 185 cases from three UK centres. Eur J Endocrinol. 2017 Mar;176(3):359-69.
https://eje.bioscientifica.com/view/journals/eje/176/3/359.xml
http://www.ncbi.nlm.nih.gov/pubmed/28073908?tool=bestpractice.com
Radiotherapy
Radiotherapy is typically used in the treatment of patients who have had either surgical biopsy or incompletely resected tumours.[38]Clark AJ, Cage TA, Aranda D, et al. A systematic review of the results of surgery and radiotherapy on tumor control for pediatric craniopharyngioma. Childs Nerv Syst. 2013 Feb;29(2):231-8.
http://www.ncbi.nlm.nih.gov/pubmed/23089933?tool=bestpractice.com
[39]Weiss M, Sutton L, Marcial V, et al. The role of radiation therapy in the management of childhood craniopharyngioma. Int J Radiat Oncol Biol Phys. 1989 Dec;17(6):1313-21.
http://www.ncbi.nlm.nih.gov/pubmed/2689398?tool=bestpractice.com
[40]Habrand JL, Ganry O, Couanet D, et al. The role of radiation therapy in the management of craniopharyngioma: a 25-year experience and review of the literature. Int J Radiat Oncol Biol Phys. 1999 May 1;44(2):255-63.
http://www.ncbi.nlm.nih.gov/pubmed/10760417?tool=bestpractice.com
[41]Varlotto JM, Flickinger JC, Kondziolka D, et al. External beam irradiation of craniopharyngioma: long-term analysis of tumor control and morbidity. Int J Radiat Oncol Biol Phys. 2002 Oct 1;54(2):492-9.
http://www.ncbi.nlm.nih.gov/pubmed/12243827?tool=bestpractice.com
Although complete resection remains the mainstay for select patients, data from retrospective studies suggest that long-term outcomes with subtotal resection followed by adjuvant radiotherapy continue to improve.[16]Zacharia BE, Bruce SS, Goldstein H, et al. Incidence, treatment and survival of patients with craniopharyngioma in the surveillance, epidemiology and end results program. Neuro Oncol. 2012 Aug;14(8):1070-8.
http://www.ncbi.nlm.nih.gov/pubmed/22735773?tool=bestpractice.com
[42]Yang I, Sughrue ME, Rutkowski MJ, et al. Craniopharyngioma: a comparison of tumor control with various treatment strategies. Neurosurg Focus. 2010 Apr;28(4):E5.
https://thejns.org/focus/view/journals/neurosurg-focus/28/4/article-pE5.xml
http://www.ncbi.nlm.nih.gov/pubmed/20367362?tool=bestpractice.com
Advanced radiotherapy modalities serve to reduce adverse effects while maintaining high cure rates. No prospective randomised clinical trials have compared complete resection with subtotal resection followed by adjuvant radiotherapy.
Advances in radiotherapy technique have made this option more effective and safe, and definitive radiotherapy may be an option in some patients. Whilst this remains controversial, observational data suggest that outcomes with definitive radiotherapy (radiotherapy alone) are comparable to those of established craniopharyngioma treatment modalities.[43]Hill TK, Baine MJ, Verma V, et al. Patterns of care in pediatric craniopharyngioma: outcomes following definitive radiotherapy. Anticancer Res. 2019 Feb;39(2):803-7.
http://www.ncbi.nlm.nih.gov/pubmed/30711960?tool=bestpractice.com
[44]Zhang C, Verma V, Lyden ER, et al. The role of definitive radiotherapy in craniopharyngioma: a SEER analysis. Am J Clin Oncol. 2018 Aug;41(8):807-12.
http://www.ncbi.nlm.nih.gov/pubmed/28263230?tool=bestpractice.com
Head-to-head prospective studies are required.
Modality
The radiotherapy technique used (conventional fractionated external beam radiation, conformal external beam radiation; or advanced techniques including intensity-modulated radiation, stereotactic radiosurgery, and proton beam therapy) is dependent upon the size of the residual tumour, its anatomic relationship to surrounding neural structures (in particular, the optic nerve and chiasm), and availability. Conventional fractionated external-beam radiotherapy (photon-based) administered daily for 5 to 6 weeks with a median tumour dose of 54 Gy is considered the standard of care for most tumours.[40]Habrand JL, Ganry O, Couanet D, et al. The role of radiation therapy in the management of craniopharyngioma: a 25-year experience and review of the literature. Int J Radiat Oncol Biol Phys. 1999 May 1;44(2):255-63.
http://www.ncbi.nlm.nih.gov/pubmed/10760417?tool=bestpractice.com
[41]Varlotto JM, Flickinger JC, Kondziolka D, et al. External beam irradiation of craniopharyngioma: long-term analysis of tumor control and morbidity. Int J Radiat Oncol Biol Phys. 2002 Oct 1;54(2):492-9.
http://www.ncbi.nlm.nih.gov/pubmed/12243827?tool=bestpractice.com
Stereotactic radiosurgery involves the delivery of a single large fraction, or several fractions, of radiation dosage, either via a linear accelerator (LINAC) or as multiple cobalt beams (Gamma Knife). Limited studies exist, although experience with other extra-axial intracranial tumours (e.g., meningiomas) suggests this is credible and effective therapy. The application of stereotactic radiosurgery is limited by tumour location in relation to the optic chiasm and nerve, and tumour size and geometry. The technique is best suited for the treatment of small (<2 cm), spherical tumours, or low-volume residual disease.[40]Habrand JL, Ganry O, Couanet D, et al. The role of radiation therapy in the management of craniopharyngioma: a 25-year experience and review of the literature. Int J Radiat Oncol Biol Phys. 1999 May 1;44(2):255-63.
http://www.ncbi.nlm.nih.gov/pubmed/10760417?tool=bestpractice.com
[45]Niranjan A, Kano H, Mathieu D, et al. Radiosurgery for craniopharyngioma. Int J Radiat Oncol Biol Phys. 2010 Sep 1;78(1):64-71.
http://www.ncbi.nlm.nih.gov/pubmed/20005637?tool=bestpractice.com
[46]Chung WY, Pan DH, Shiau CY, et al. Gamma knife radiosurgery for craniopharyngiomas. J Neurosurg. 2000 Dec;93(suppl 3):47-56.
http://www.ncbi.nlm.nih.gov/pubmed/11143262?tool=bestpractice.com
[47]Scarzello G, Buzzaccarini MS, Perilongo G, et al. Acute and late morbidity after limited resection and focal radiation therapy in craniopharyngiomas. J Pediatr Endocrinol Metab. 2006 Apr;19 Suppl 1:399-405.
http://www.ncbi.nlm.nih.gov/pubmed/16700317?tool=bestpractice.com
[48]Minniti G, Saran F, Traish D, et al. Fractionated stereotactic conformal radiotherapy following conservative surgery in the control of craniopharyngiomas. Radiother Oncol. 2007 Jan;82(1):90-5.
http://www.ncbi.nlm.nih.gov/pubmed/17161483?tool=bestpractice.com
Radiotherapy in many instances will result in hypopituitarism and consequently the need for hormone replacement therapy.[24]Sorva R, Heiskanen O, Perheetupa J. Craniopharyngioma surgery in children: endocrine and visual outcome. Childs Nerv Syst. 1988 Apr;4(2):97-9.
http://www.ncbi.nlm.nih.gov/pubmed/3401877?tool=bestpractice.com
[47]Scarzello G, Buzzaccarini MS, Perilongo G, et al. Acute and late morbidity after limited resection and focal radiation therapy in craniopharyngiomas. J Pediatr Endocrinol Metab. 2006 Apr;19 Suppl 1:399-405.
http://www.ncbi.nlm.nih.gov/pubmed/16700317?tool=bestpractice.com
[49]Müller HL. Consequences of craniopharyngioma surgery in children. J Clin Endocrinol Metab. 2011 Jul;96(7):1981-91.
https://academic.oup.com/jcem/article/96/7/1981/2833879
http://www.ncbi.nlm.nih.gov/pubmed/21508127?tool=bestpractice.com
Other possible complications include loss of vision (secondary to a radiation-induced optic neuropathy), rarely radiation injury/necrosis of the anterior temporal lobes, radiation injury to the hypothalamus, and induction of neurocognitive deficits.[50]Poretti A, Grotzer MA, Ribi K, et al. Outcome of craniopharyngioma in children: long-term complications and quality of life. Dev Med Child Neurol. 2004 Apr;46(4):220-9.
http://onlinelibrary.wiley.com/doi/10.1111/j.1469-8749.2004.tb00476.x/pdf
http://www.ncbi.nlm.nih.gov/pubmed/15077699?tool=bestpractice.com
[51]Kiehna EN, Mulhem RK, Li C, et al. Changes in attentional performance of children and young adults with localized primary brain tumors after conformal radiation therapy. J Clin Oncol. 2006 Nov 20;24(33):5283-90.
https://ascopubs.org/doi/full/10.1200/JCO.2005.03.8547
http://www.ncbi.nlm.nih.gov/pubmed/17114662?tool=bestpractice.com
Endocrine therapy
Endocrine replacement therapy depends upon the specific endocrine deficiency.[4]Karavitaki N, Cudlip S, Adams CB, et al. Craniopharyngiomas. Endocr Rev. 2006 Jun;27(4):371-97.
https://academic.oup.com/edrv/article/27/4/371/2355225
http://www.ncbi.nlm.nih.gov/pubmed/16543382?tool=bestpractice.com
[8]Halac I, Zimmerman D. Endocrine manifestations of craniopharyngioma. Childs Nerv Syst. 2005 Aug;21(8-9):640-8.
https://link.springer.com/article/10.1007%2Fs00381-005-1246-x
http://www.ncbi.nlm.nih.gov/pubmed/16047216?tool=bestpractice.com
[9]Hopper N, Albanese A, Ghirardello S, et al. The preoperative endocrine assessment of craniopharyngiomas. J Pediatr Endocrinol Metab. 2006 Apr;19(suppl 1):325-7.
http://www.ncbi.nlm.nih.gov/pubmed/16700307?tool=bestpractice.com
[11]Garre ML, Cama A. Craniopharyngioma: modern concepts in pathogenesis and treatment. Curr Opin Pediatr. 2007 Aug;19(4):471-9.
http://www.ncbi.nlm.nih.gov/pubmed/17630614?tool=bestpractice.com
[49]Müller HL. Consequences of craniopharyngioma surgery in children. J Clin Endocrinol Metab. 2011 Jul;96(7):1981-91.
https://academic.oup.com/jcem/article/96/7/1981/2833879
http://www.ncbi.nlm.nih.gov/pubmed/21508127?tool=bestpractice.com
[52]Müller HL, Gebhardt U, Teske C, et al. Post-operative hypothalamic lesions and obesity in childhood craniopharyngioma: results of the multinational prospective trial KRANIOPHARYNGEOM 2000 after three year follow-up. Eur J Endocrinol. 2011 Jul;165(1):17-24.
https://eje.bioscientifica.com/view/journals/eje/165/1/17.xml
http://www.ncbi.nlm.nih.gov/pubmed/21490122?tool=bestpractice.com
[53]Winkfield KM, Tsai HK, Yao X, et al. Long-term clinical outcomes following treatment of childhood craniopharyngioma. Pediatr Blood Cancer. 2011 Jul 1;56(7):1120-6.
http://www.ncbi.nlm.nih.gov/pubmed/21488157?tool=bestpractice.com
No improvement is seen in baseline endocrine dysfunction following surgery (with the possible exception of hyperprolactinaemia). Indeed, the incidence increases following therapy as a consequence of surgery (lowest risk with trans-sphenoidal surgery).
Approximate prevalence of specific deficiencies includes growth hormone (75%), hypogonadotrophic hypogonadism (75%), adrenocorticotrophic hormone deficiency (25%), hypothyroidism (25%), and diabetes insipidus (>70% in children; 50% in adults).[4]Karavitaki N, Cudlip S, Adams CB, et al. Craniopharyngiomas. Endocr Rev. 2006 Jun;27(4):371-97.
https://academic.oup.com/edrv/article/27/4/371/2355225
http://www.ncbi.nlm.nih.gov/pubmed/16543382?tool=bestpractice.com
[8]Halac I, Zimmerman D. Endocrine manifestations of craniopharyngioma. Childs Nerv Syst. 2005 Aug;21(8-9):640-8.
https://link.springer.com/article/10.1007%2Fs00381-005-1246-x
http://www.ncbi.nlm.nih.gov/pubmed/16047216?tool=bestpractice.com
[9]Hopper N, Albanese A, Ghirardello S, et al. The preoperative endocrine assessment of craniopharyngiomas. J Pediatr Endocrinol Metab. 2006 Apr;19(suppl 1):325-7.
http://www.ncbi.nlm.nih.gov/pubmed/16700307?tool=bestpractice.com
[52]Müller HL, Gebhardt U, Teske C, et al. Post-operative hypothalamic lesions and obesity in childhood craniopharyngioma: results of the multinational prospective trial KRANIOPHARYNGEOM 2000 after three year follow-up. Eur J Endocrinol. 2011 Jul;165(1):17-24.
https://eje.bioscientifica.com/view/journals/eje/165/1/17.xml
http://www.ncbi.nlm.nih.gov/pubmed/21490122?tool=bestpractice.com
[53]Winkfield KM, Tsai HK, Yao X, et al. Long-term clinical outcomes following treatment of childhood craniopharyngioma. Pediatr Blood Cancer. 2011 Jul 1;56(7):1120-6.
http://www.ncbi.nlm.nih.gov/pubmed/21488157?tool=bestpractice.com
Management of recurrent/refractory disease
Recurrent or treatment refractory disease is established both clinically and radiographically. If present, repeat surgery may be indicated.[54]Liubinas SV, Munshey AS, Kaye AH. Management of recurrent craniopharyngioma. J Clin Neurosci. 2011 Apr;18(4):451-7.
http://www.ncbi.nlm.nih.gov/pubmed/21316970?tool=bestpractice.com
Radiotherapy may be used to treat recurrence, and observational data suggest that stereotactic radiosurgery is an effective, minimally invasive option in this context.[45]Niranjan A, Kano H, Mathieu D, et al. Radiosurgery for craniopharyngioma. Int J Radiat Oncol Biol Phys. 2010 Sep 1;78(1):64-71.
http://www.ncbi.nlm.nih.gov/pubmed/20005637?tool=bestpractice.com
Recurrences may manifest as a recalcitrant tumour cyst requiring surgical drainage (aspiration) and sometimes placement of an intratumoural cyst catheter and sub-galeal reservoir. This allows repeated fluid aspiration and, if necessary, instillation of intracavitary radioactive colloidal phosphorus/yttrium.[55]Julow J, Backlund E-O, Lanyi F, et al. Long-term results and late complications after intracavitary yttrium-90 colloid irradiation of recurrent cystic craniopharyngiomas. Neurosurgery. 2007 Aug;61(2):288-95.
http://www.ncbi.nlm.nih.gov/pubmed/17762741?tool=bestpractice.com
[56]Van den Berg JH, Blaauw G, Breeman WA, et al. Intracavitary brachytherapy of cystic craniopharyngiomas. J Neurosurg. 1992 Oct;77(4):545-50.
http://www.ncbi.nlm.nih.gov/pubmed/1527612?tool=bestpractice.com
[57]Pollack IF, Lunsford LD, Slamovits TI, et al. Stereotaxic intracavitary irradiation for cystic craniopharyngiomas. J Neurosurg. 1988 Feb;68(2):227-33.
http://www.ncbi.nlm.nih.gov/pubmed/3276836?tool=bestpractice.com
Alternatively, chemotherapy agents may be placed; a variety of drugs have been utilised, including bleomycin, methotrexate, and cytarabine.[58]Zhang S, Fang Y, Cai BW, et al. Intracystic bleomycin for cystic craniopharyngiomas in children. Cochrane Database Syst Rev. 2016 Jul 14;7:CD008890.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6457977
http://www.ncbi.nlm.nih.gov/pubmed/27416004?tool=bestpractice.com
Caution is required if intracystic therapies are used, as leakage carries toxicity to the optic structures and perforator vessels.
In exceptional instances (e.g., tumour still present despite prior surgery/radiotherapy and no longer operable), patients may be treated with systemic chemotherapy.[54]Liubinas SV, Munshey AS, Kaye AH. Management of recurrent craniopharyngioma. J Clin Neurosci. 2011 Apr;18(4):451-7.
http://www.ncbi.nlm.nih.gov/pubmed/21316970?tool=bestpractice.com
However, data for chemotherapy in refractory craniopharyngioma are limited, and there is no standard systemic regimen.
Long-term sequelae
In addition to immediate management of the craniopharyngioma and endocrine deficiencies, the detection and management of the potential longer-term sequelae (such as delayed optic atrophy, hypopituitarism, obesity, hyperlipidaemia, and diabetes mellitus) is essential, particularly in children.[49]Müller HL. Consequences of craniopharyngioma surgery in children. J Clin Endocrinol Metab. 2011 Jul;96(7):1981-91.
https://academic.oup.com/jcem/article/96/7/1981/2833879
http://www.ncbi.nlm.nih.gov/pubmed/21508127?tool=bestpractice.com
[59]Sahakitrungruang T, Klomchan T, Supornsilchai V, et al. Obesity, metabolic syndrome, and insulin dynamics in children after craniopharyngioma surgery. Eur J Pediatr. 2011 Jun;170(6):763-9.
http://www.ncbi.nlm.nih.gov/pubmed/21107605?tool=bestpractice.com
[60]Lo AC, Howard AF, Nichol A, et al. Long-term outcomes and complications in patients with craniopharyngioma: the British Columbia Cancer Agency experience. Int J Radiat Oncol Biol Phys. 2014 Apr 1;88(5):1011-8.
http://www.ncbi.nlm.nih.gov/pubmed/24661653?tool=bestpractice.com
Quality of life is significantly impacted. Craniopharyngioma is best thought of as a chronic disease that is multi-dimensional.[61]Müller HL. Childhood craniopharyngioma. Pituitary. 2013 Mar;16(1):56-67.
http://rd.springer.com/article/10.1007%2Fs11102-012-0401-0
http://www.ncbi.nlm.nih.gov/pubmed/22678820?tool=bestpractice.com
Additionally, adults with craniopharyngioma have a substantially elevated risk of cardiovascular disease relative to the general population, added to the reduced health already common to these patients.[62]Erfurth EM. Endocrine aspects and sequel in patients with craniopharyngioma. J Pediatr Endocrinol Metab. 2015 Jan;28(1-2):19-26.
http://www.ncbi.nlm.nih.gov/pubmed/25514328?tool=bestpractice.com
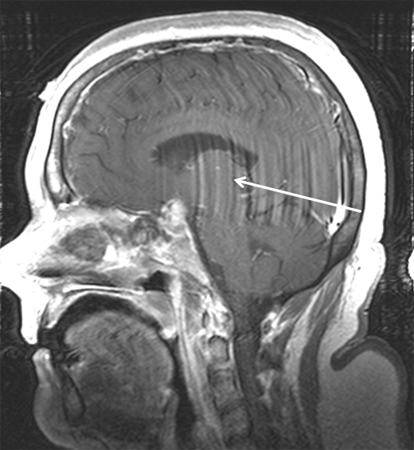 [Figure caption and citation for the preceding image starts]: Craniopharyngioma (postoperative): sagittal post-contrast MRIFrom the collection of Marc C. Chamberlain [Citation ends].
[Figure caption and citation for the preceding image starts]: Craniopharyngioma (postoperative): sagittal post-contrast MRIFrom the collection of Marc C. Chamberlain [Citation ends].